Dr. Kumar presented on extubation problems and their management. Some key points:
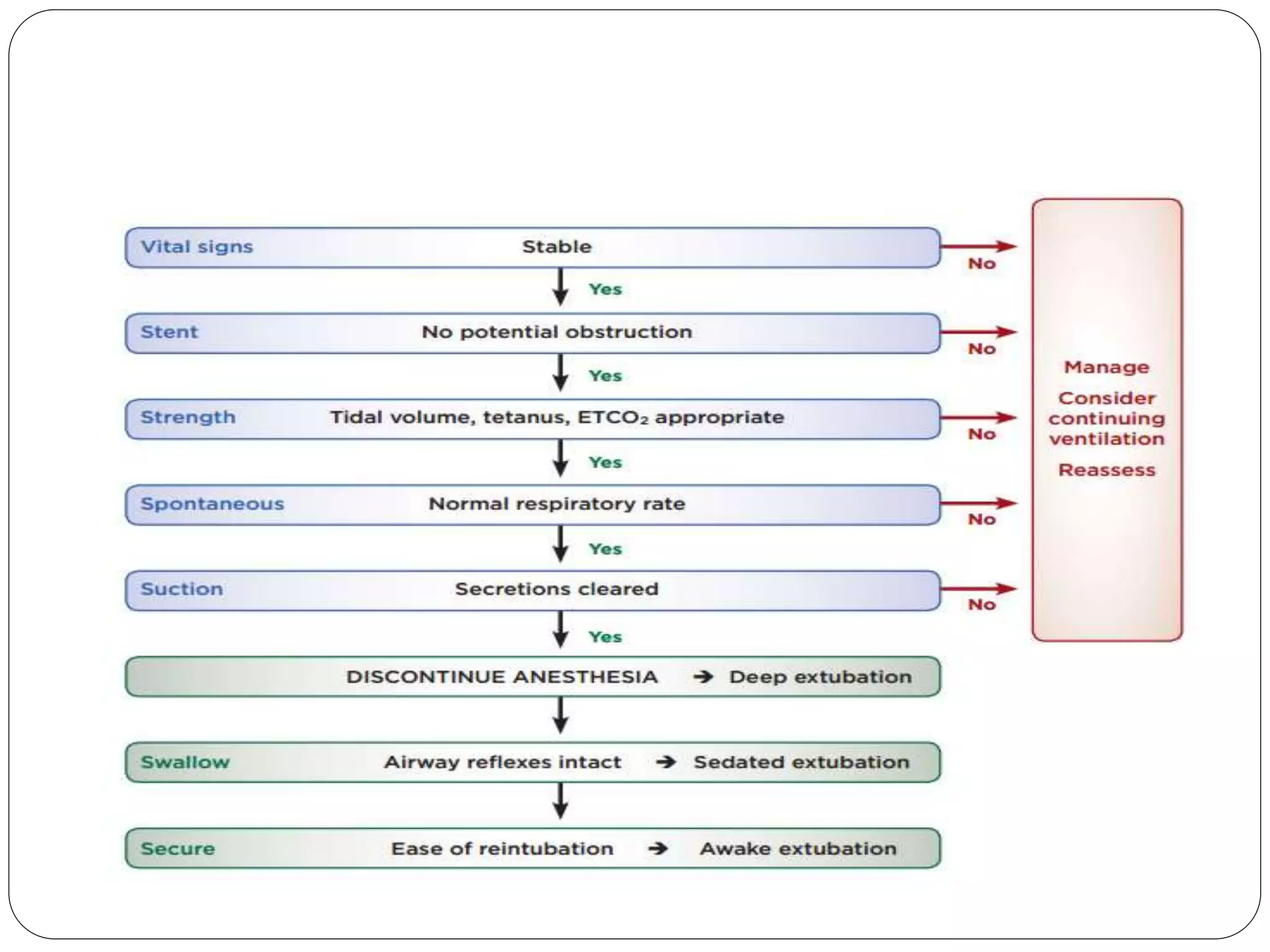
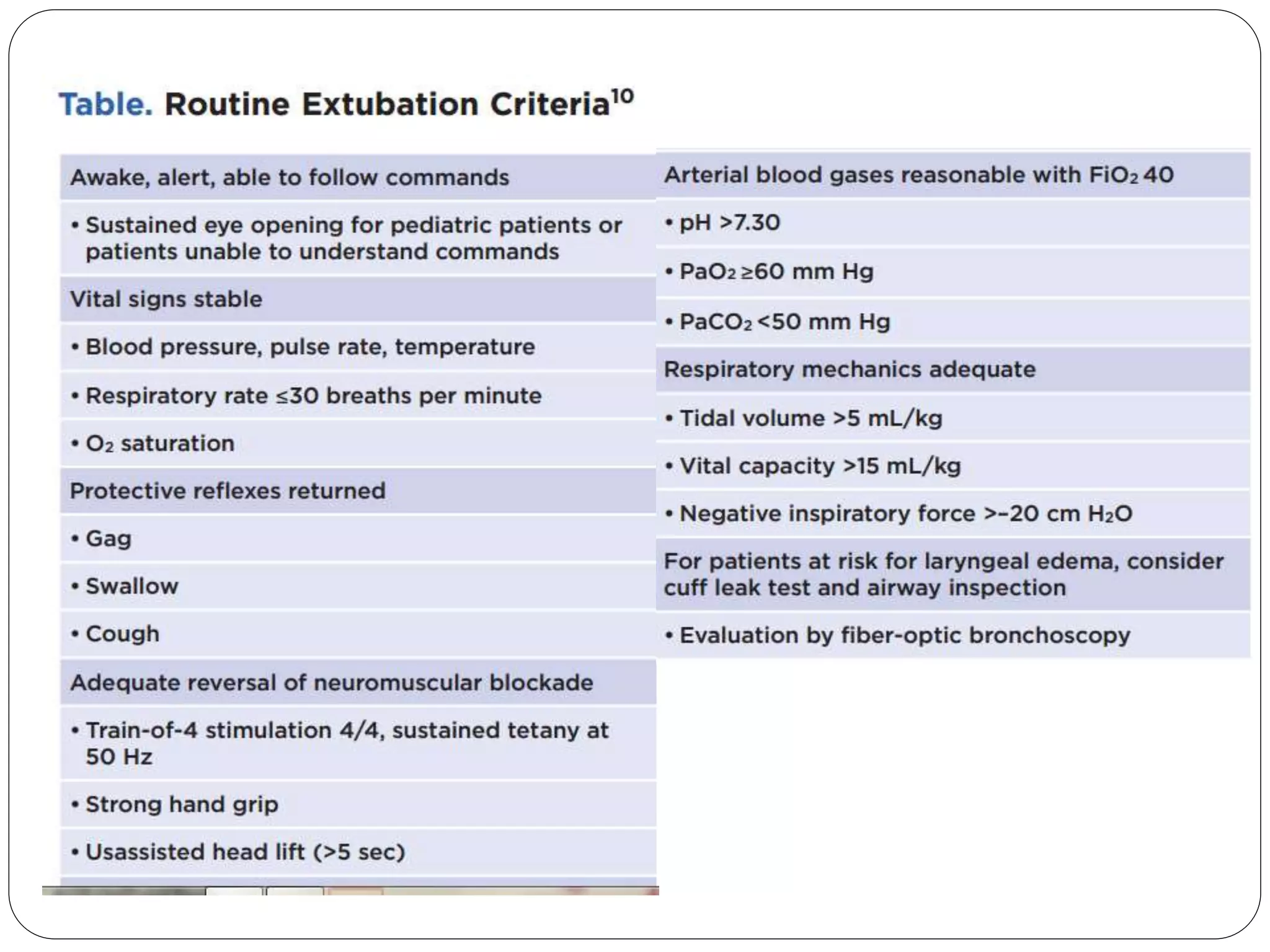
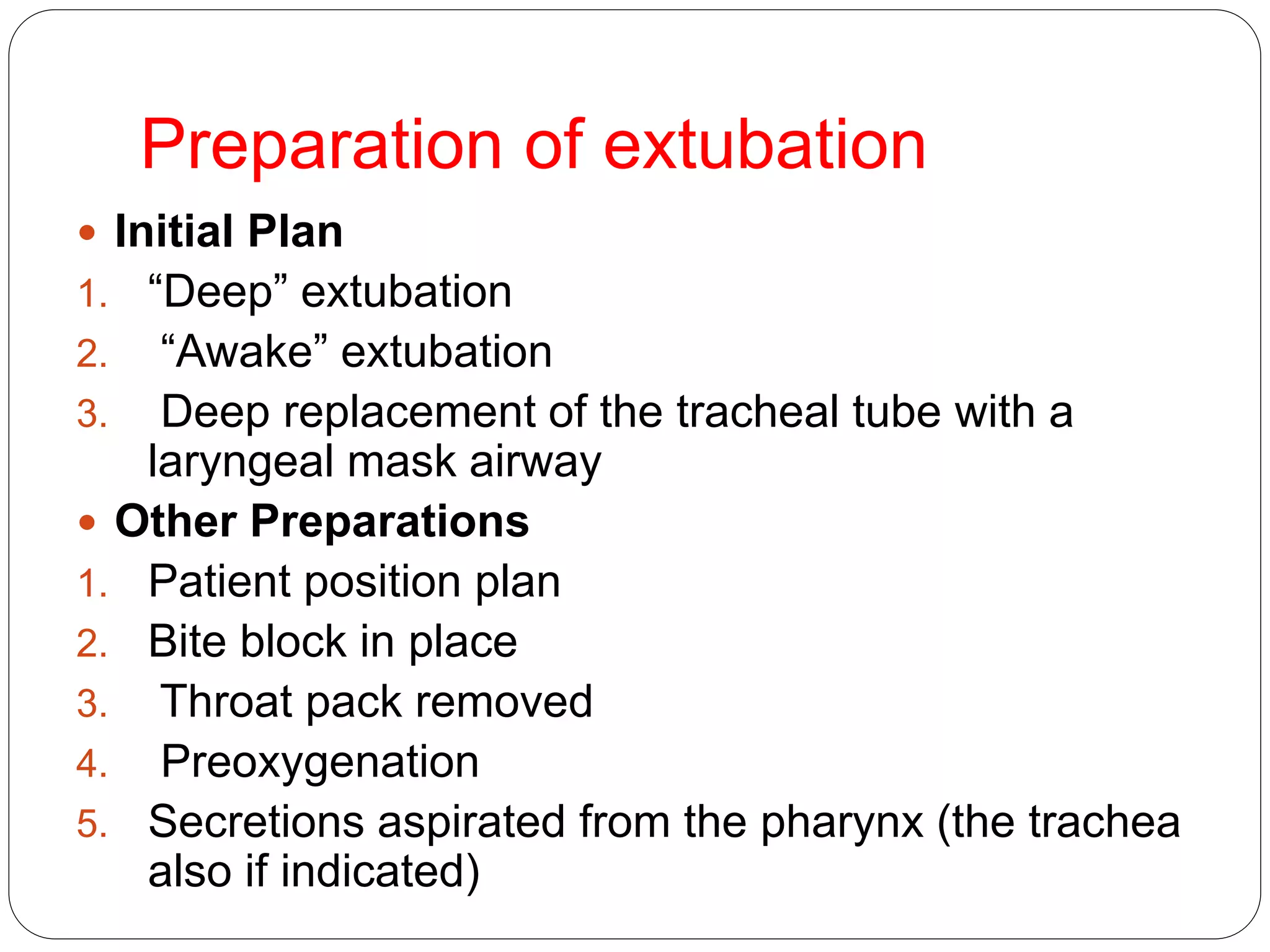
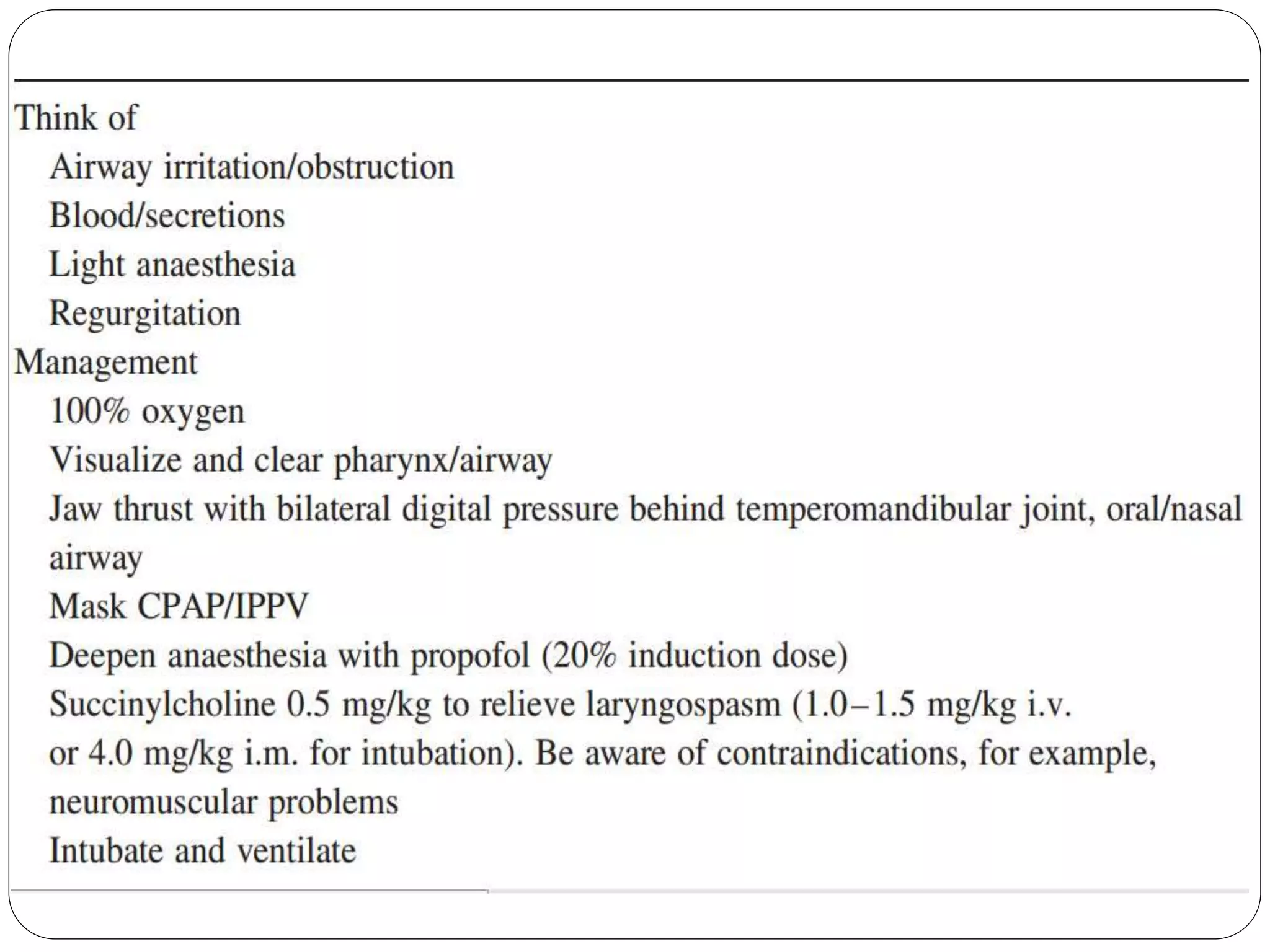
1. Tracheal extubation requires careful planning and preparation to prevent complications like laryngospasm, laryngeal edema, and pulmonary aspiration.
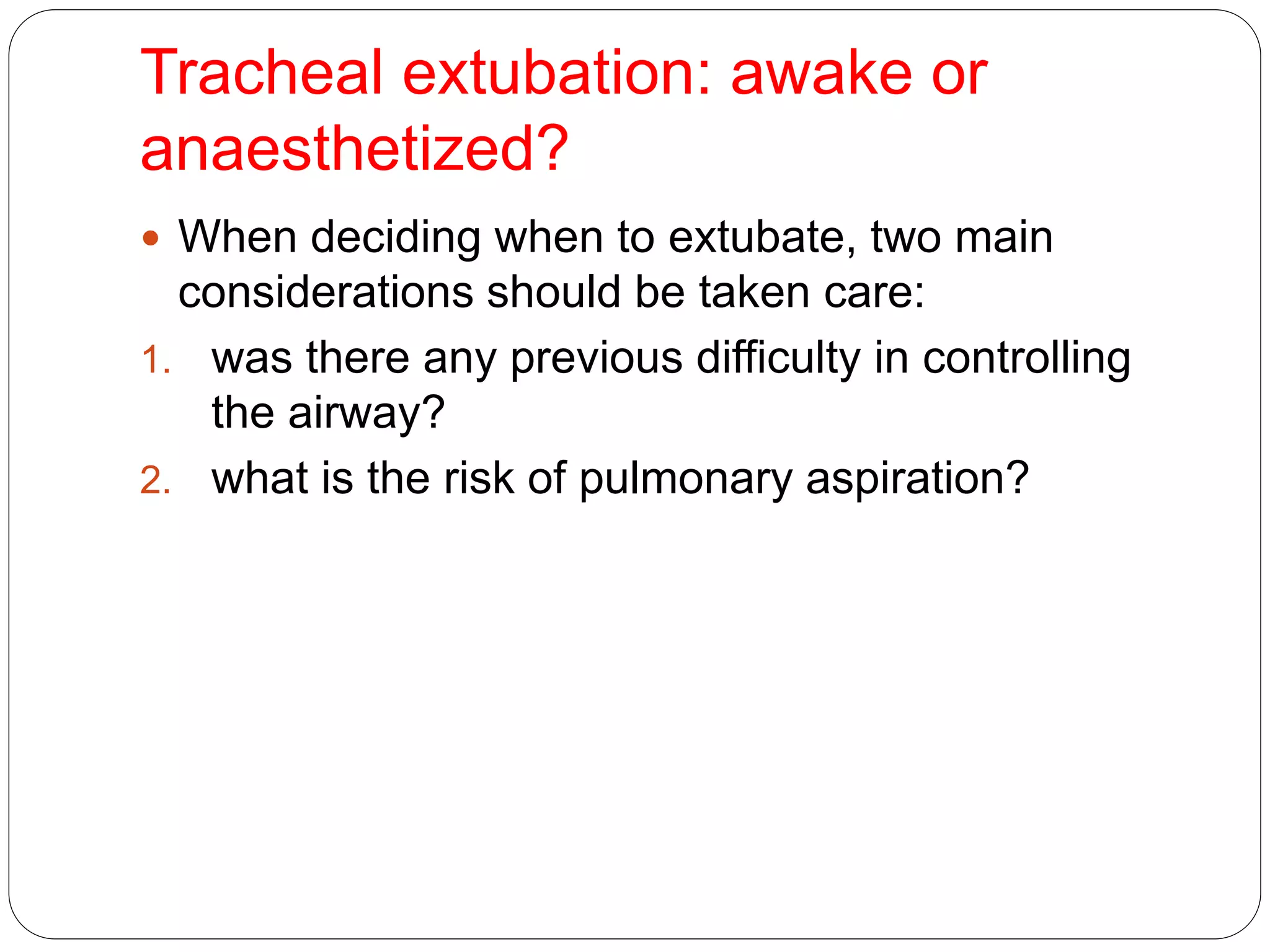
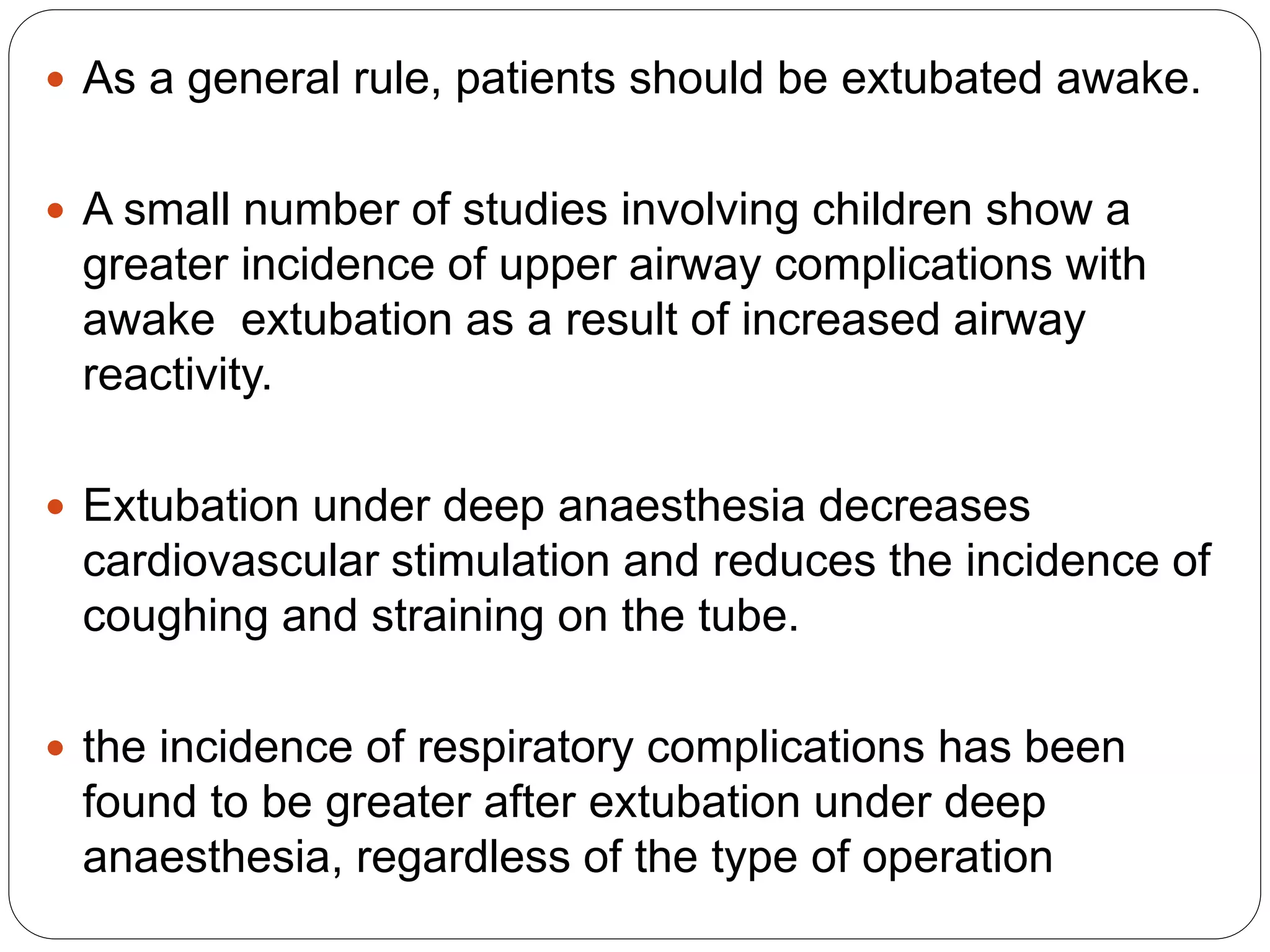
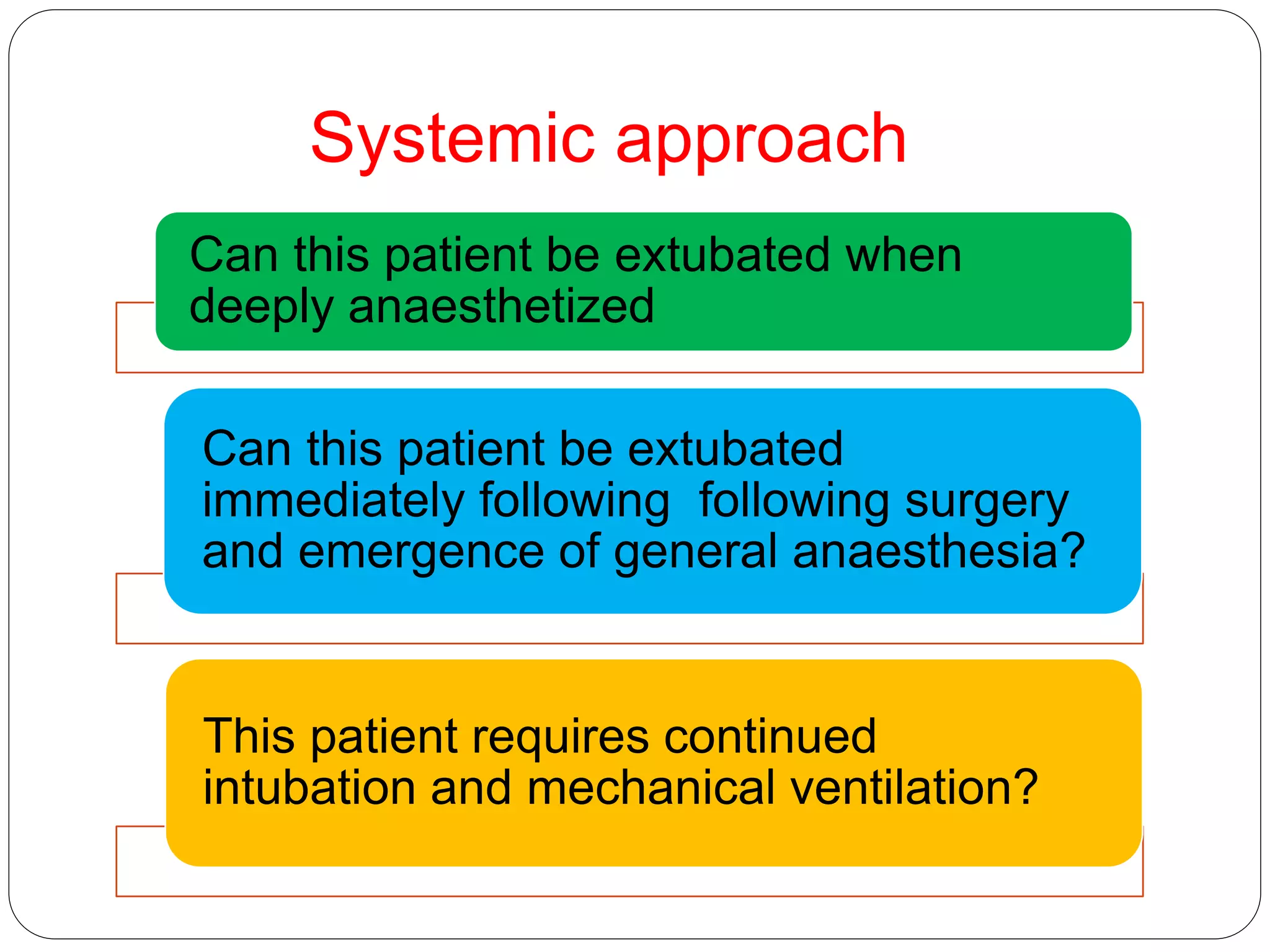
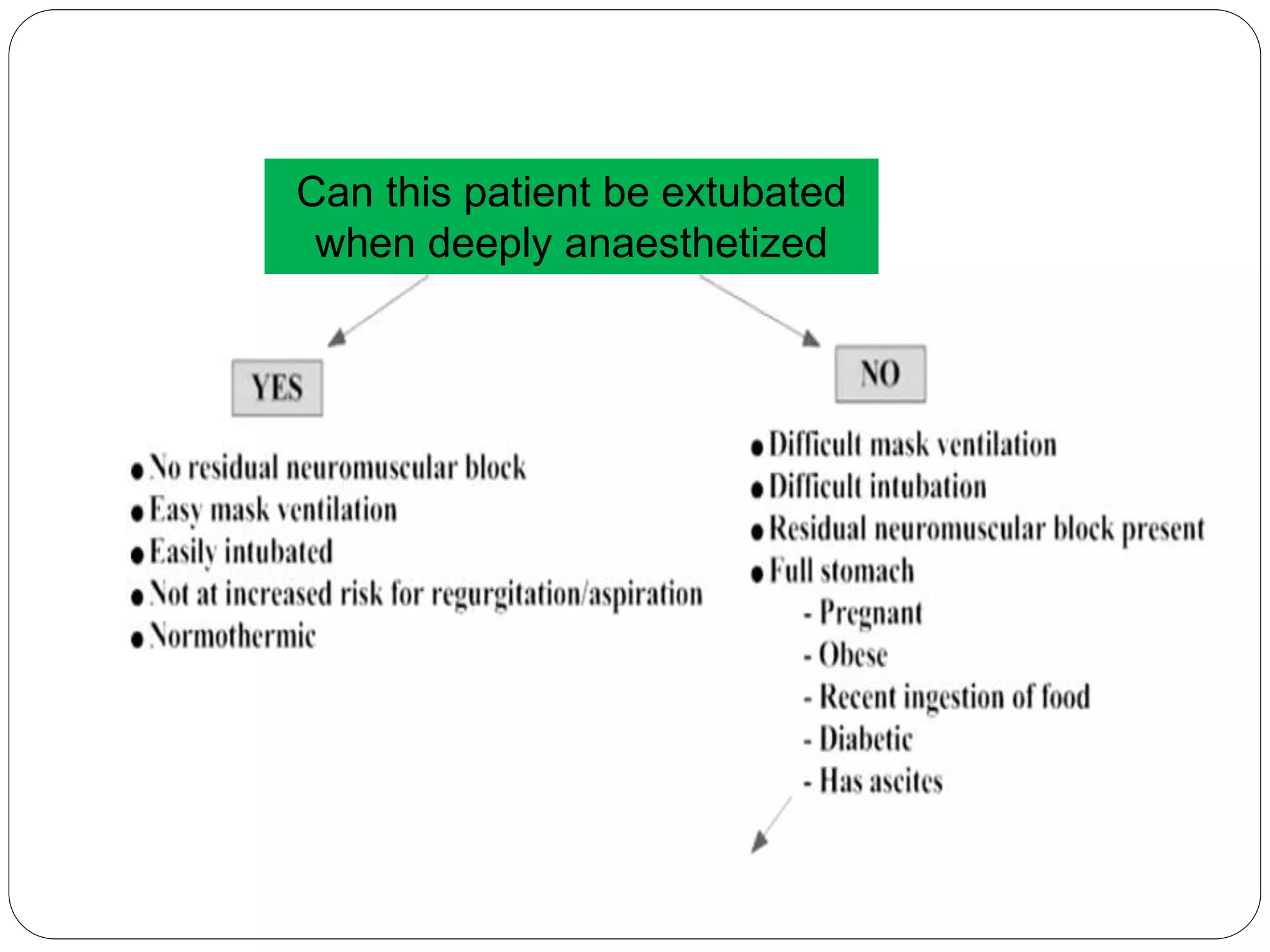
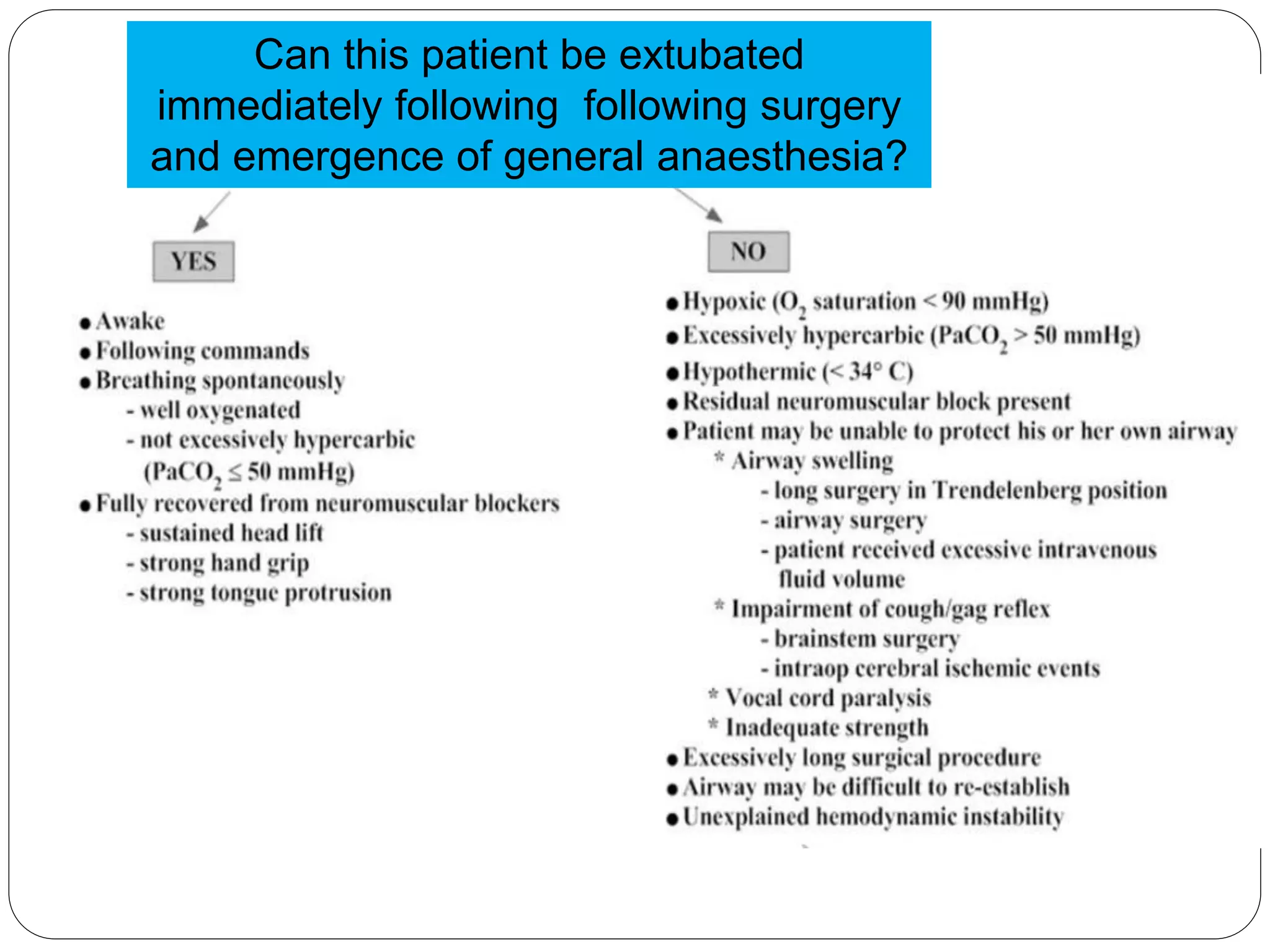
2. Patients should generally be extubated awake to allow for airway protection, but deep extubation may be considered to reduce cardiovascular stimulation.
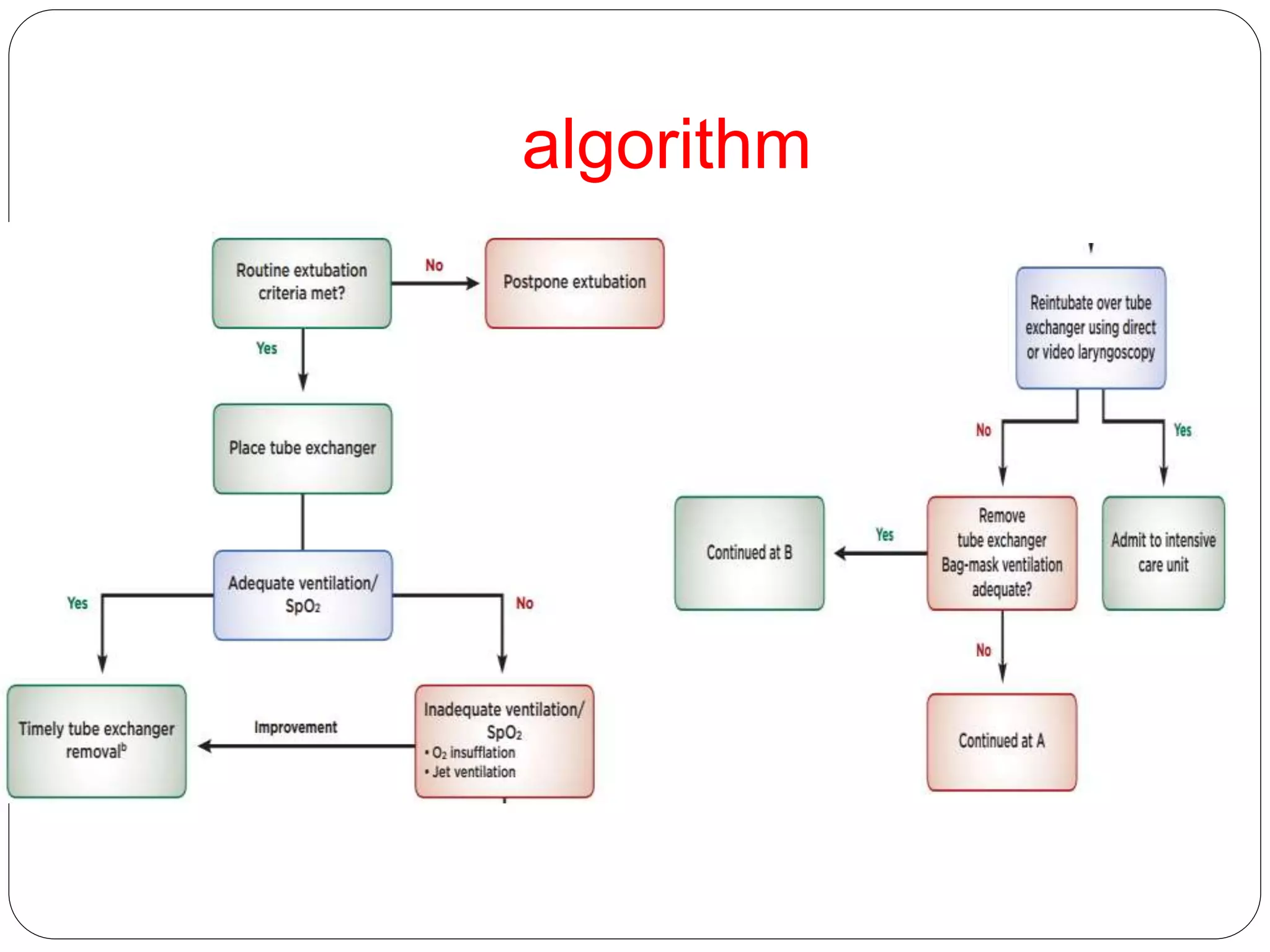
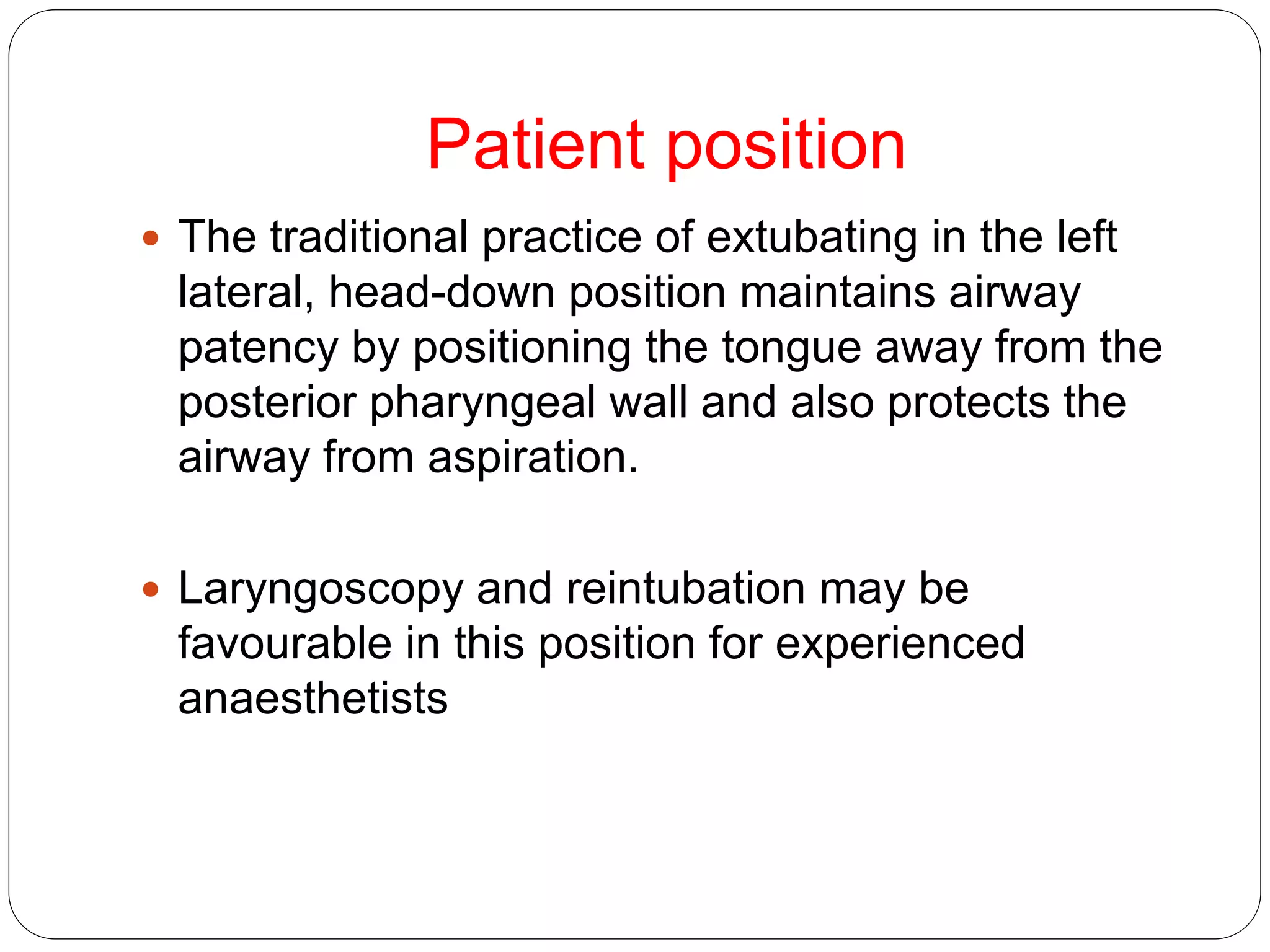
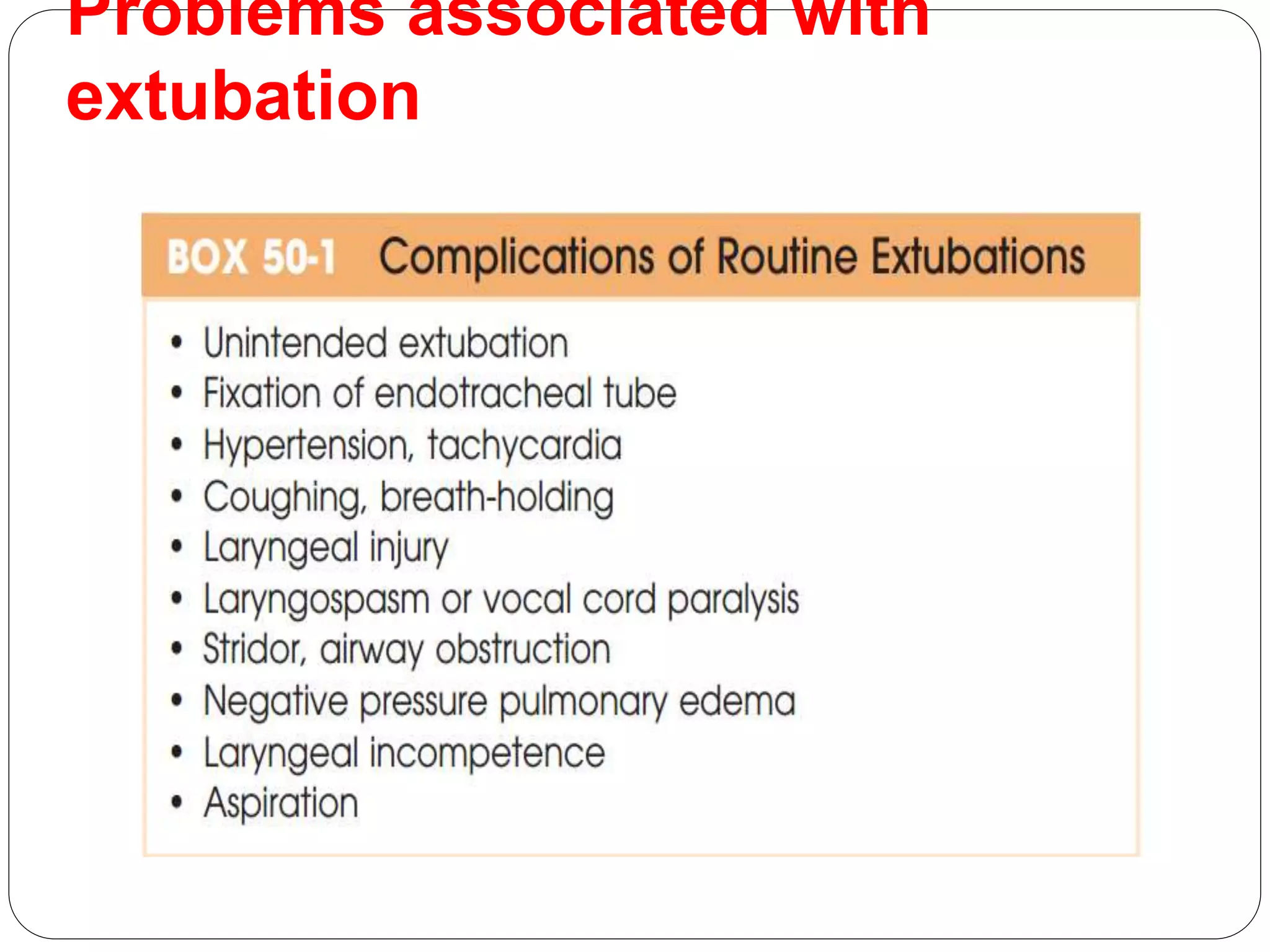
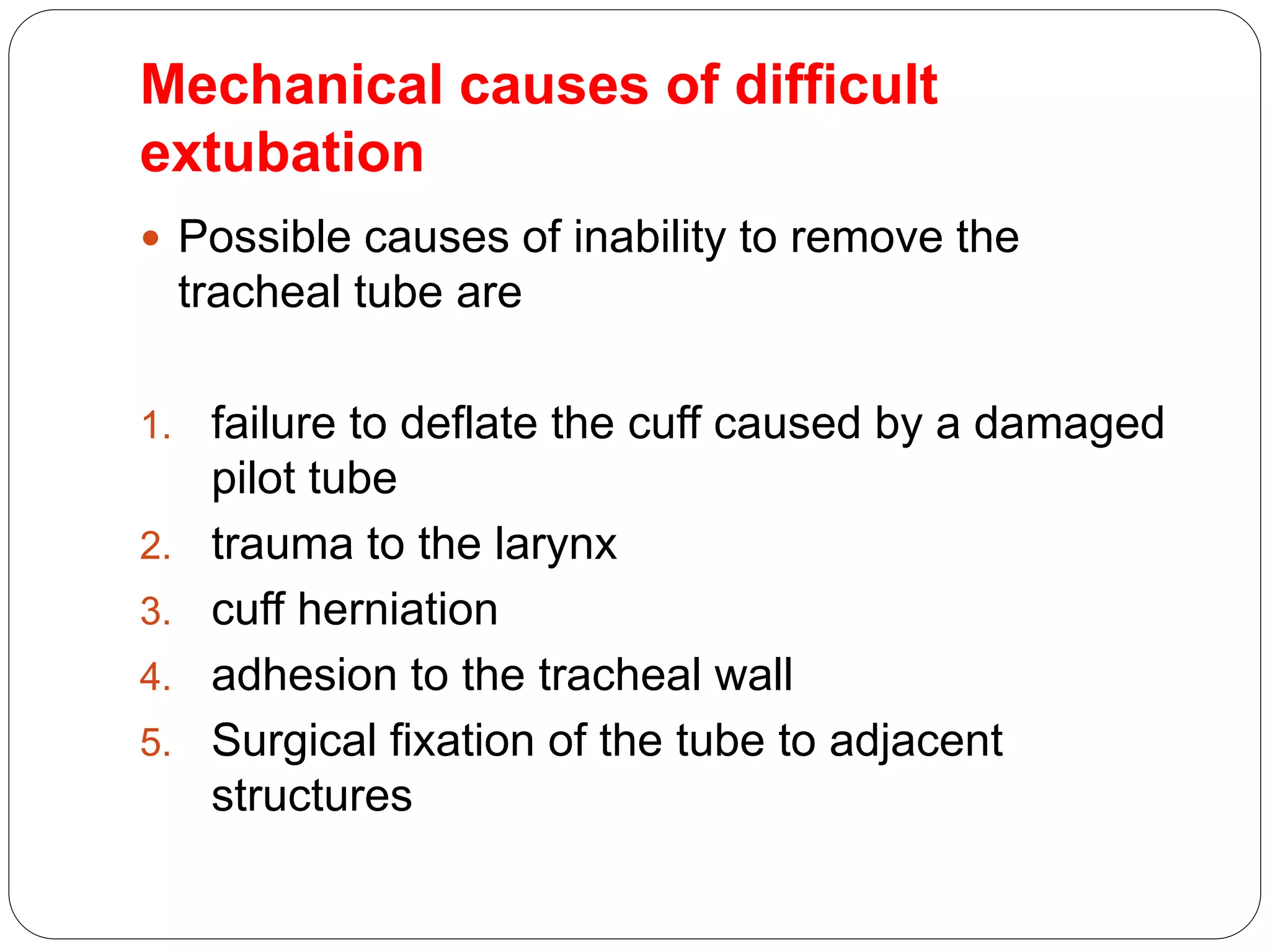
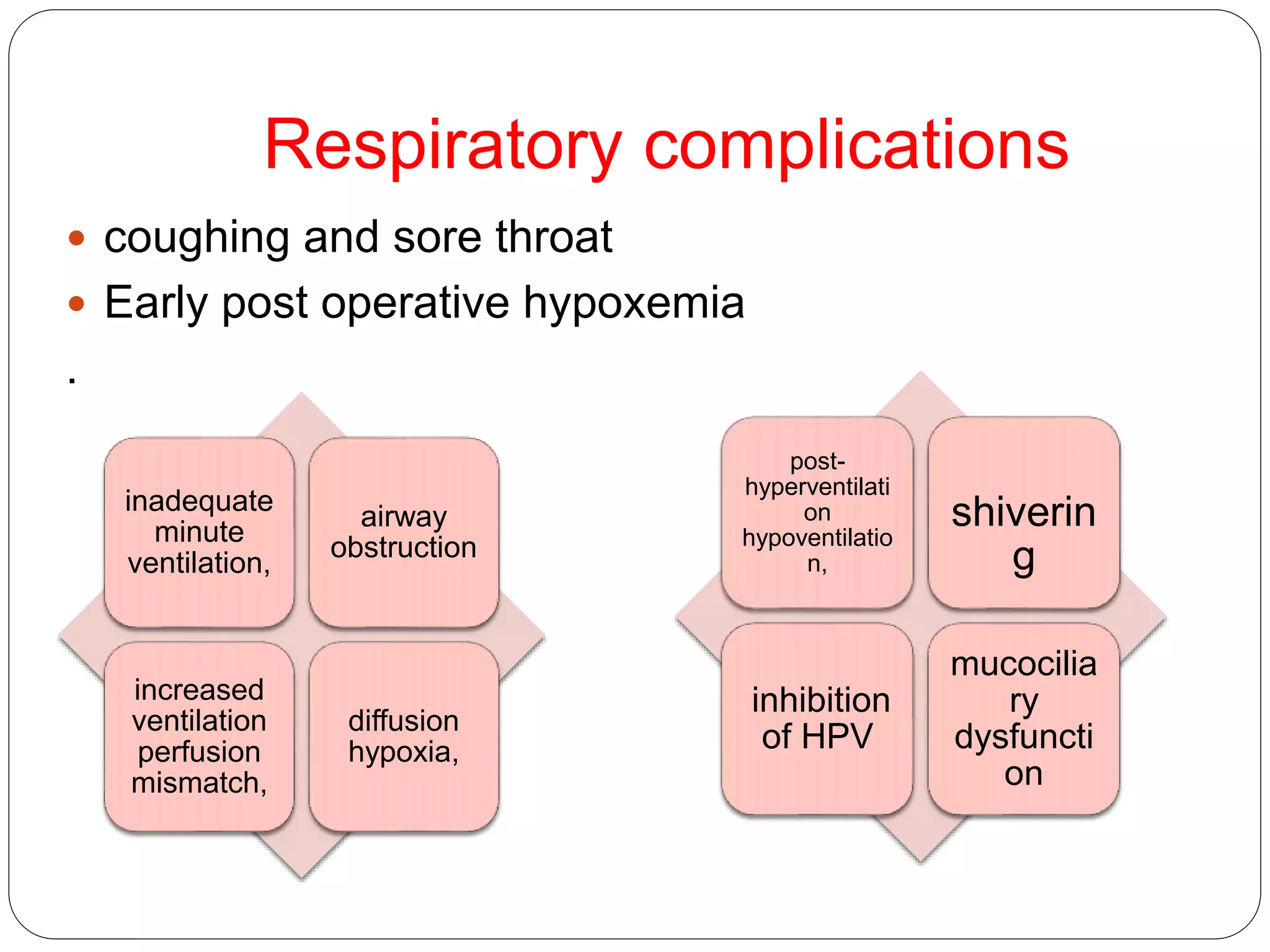
3. Potential problems include mechanical issues removing the tube, cardiovascular changes, respiratory complications, and airway obstruction. Management depends on the specific issue but may include medications, positioning, or alternative extubation techniques.
4. Careful evaluation of each patient's risk factors and planning is necessary to safely perform extubation and prevent
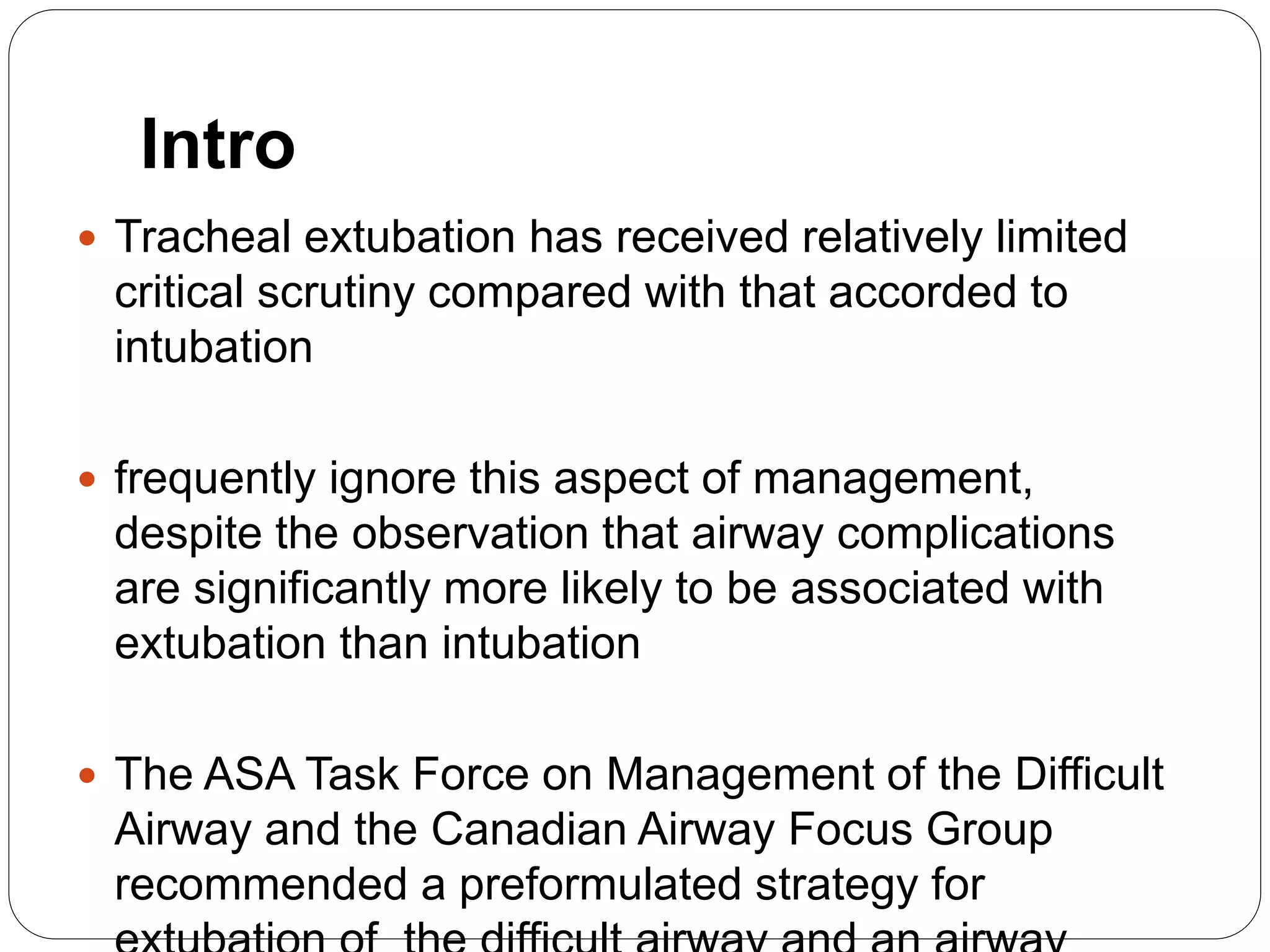
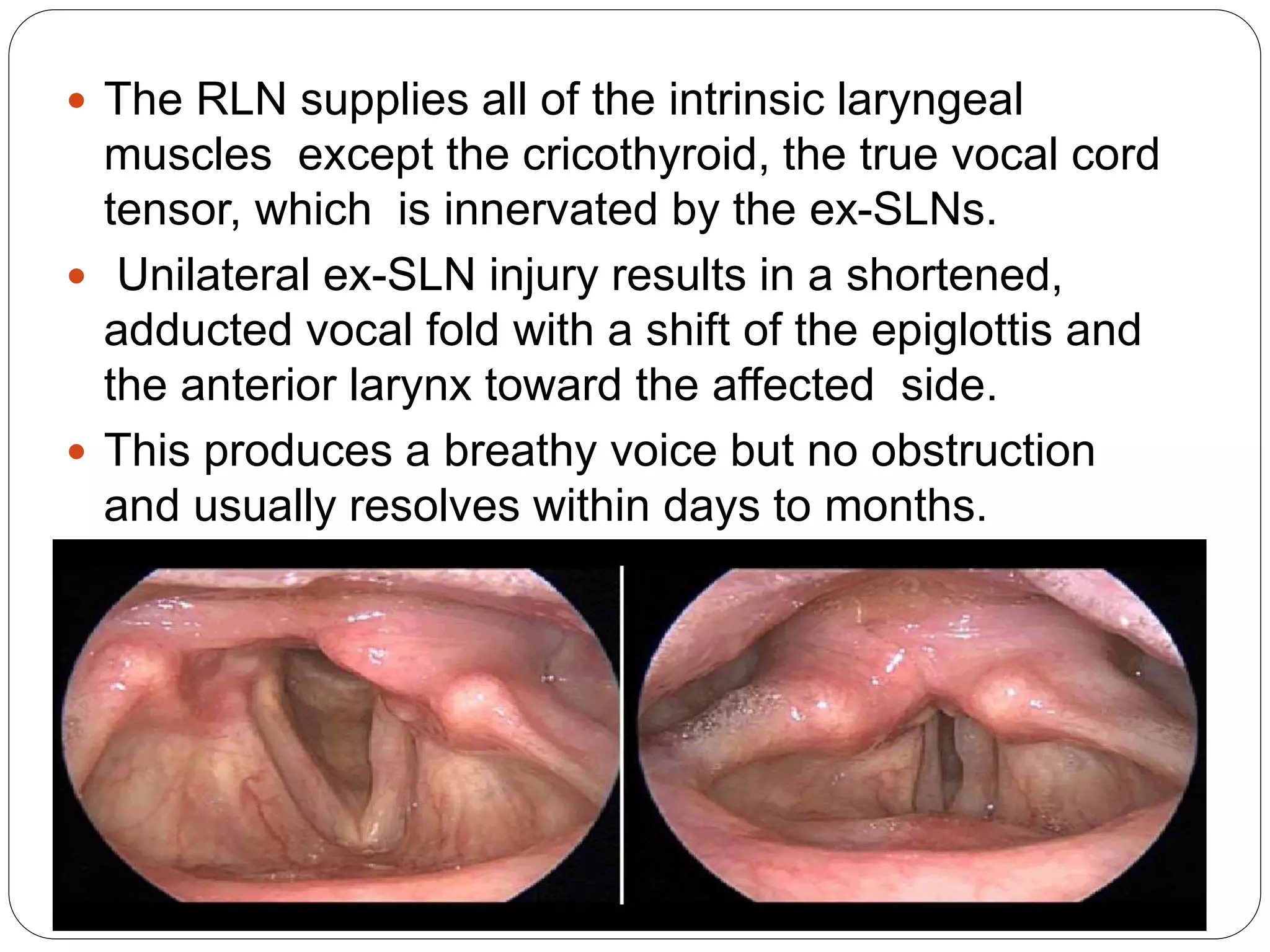
![Vocal cord paralysis
Vocal fold paralysis results from injury to the vagus or
one of its branches (i.e., recurrent laryngeal nerve
[RLN] or external division of the superior laryngeal
nerve [ex-SLN]
When vocal fold paralysis occurs as a surgical
complication, it is usually associated with neck,
thyroid, or thoracic surgery.
The left RLN can also be compressed by
I. thoracic tumors,
II. aortic aneurysmal dilatation
III. left atrial enlargement](https://image.slidesharecdn.com/extubationproblems-150602065440-lva1-app6891/75/Extubation-problems-and-its-management-31-2048.jpg)