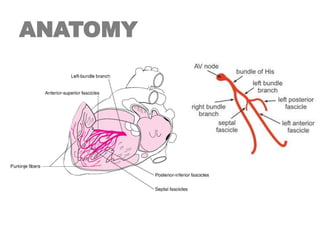
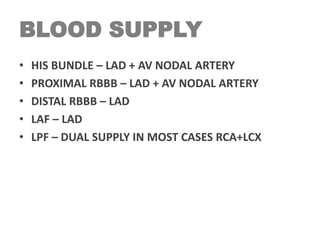
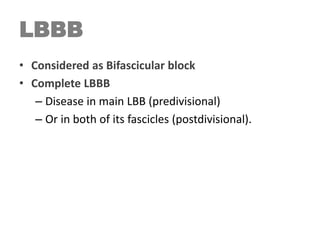
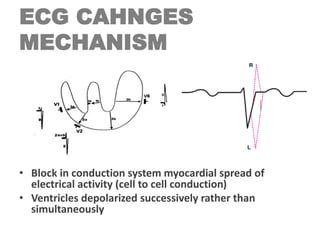
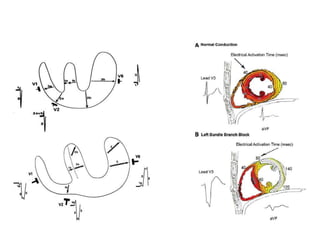
1. Left bundle branch block (LBBB) is a conduction abnormality caused by impaired conduction in the left bundle branch or its fascicles.
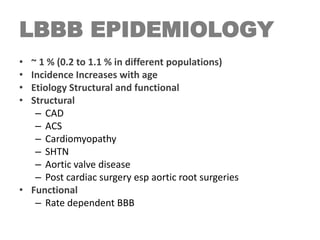
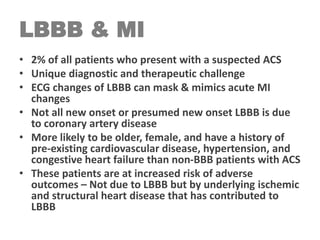
2. LBBB can be chronic or intermittent and is often caused by coronary artery disease or hypertension.
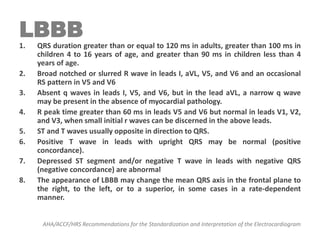
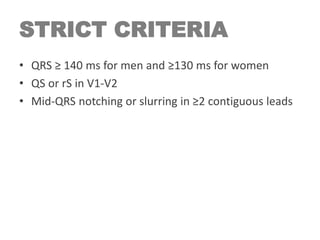
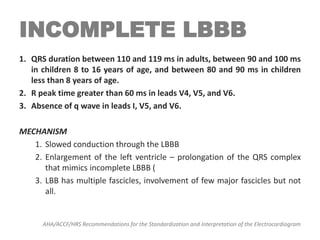
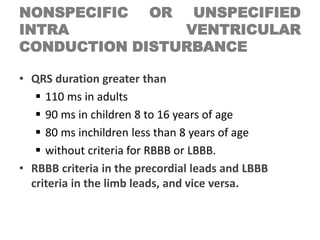
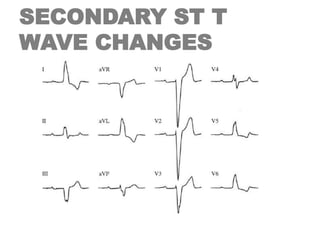
3. On ECG, LBBB is characterized by a QRS duration ≥120ms and other abnormalities including broad R waves and abnormal ST-T wave patterns.
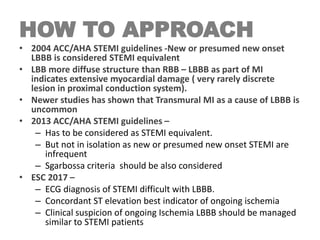
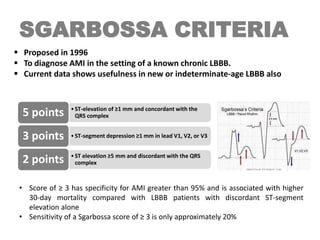
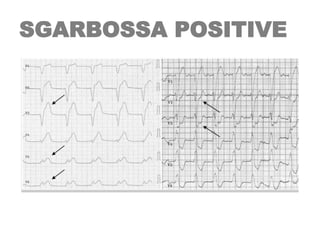
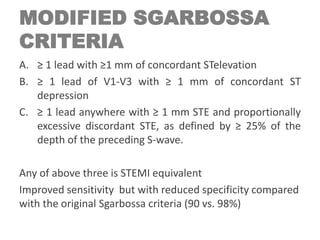
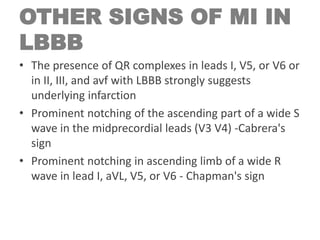
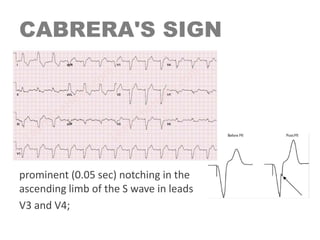
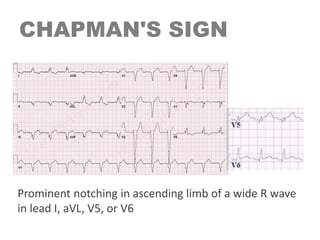
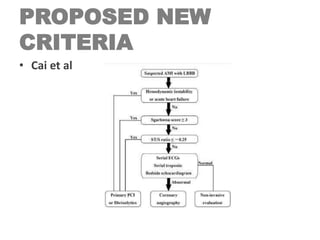
4. LBBB can make ECG diagnosis of myocardial infarction difficult and criteria like Sgarbossa scores are used to help identify MI in the setting of LBBB.