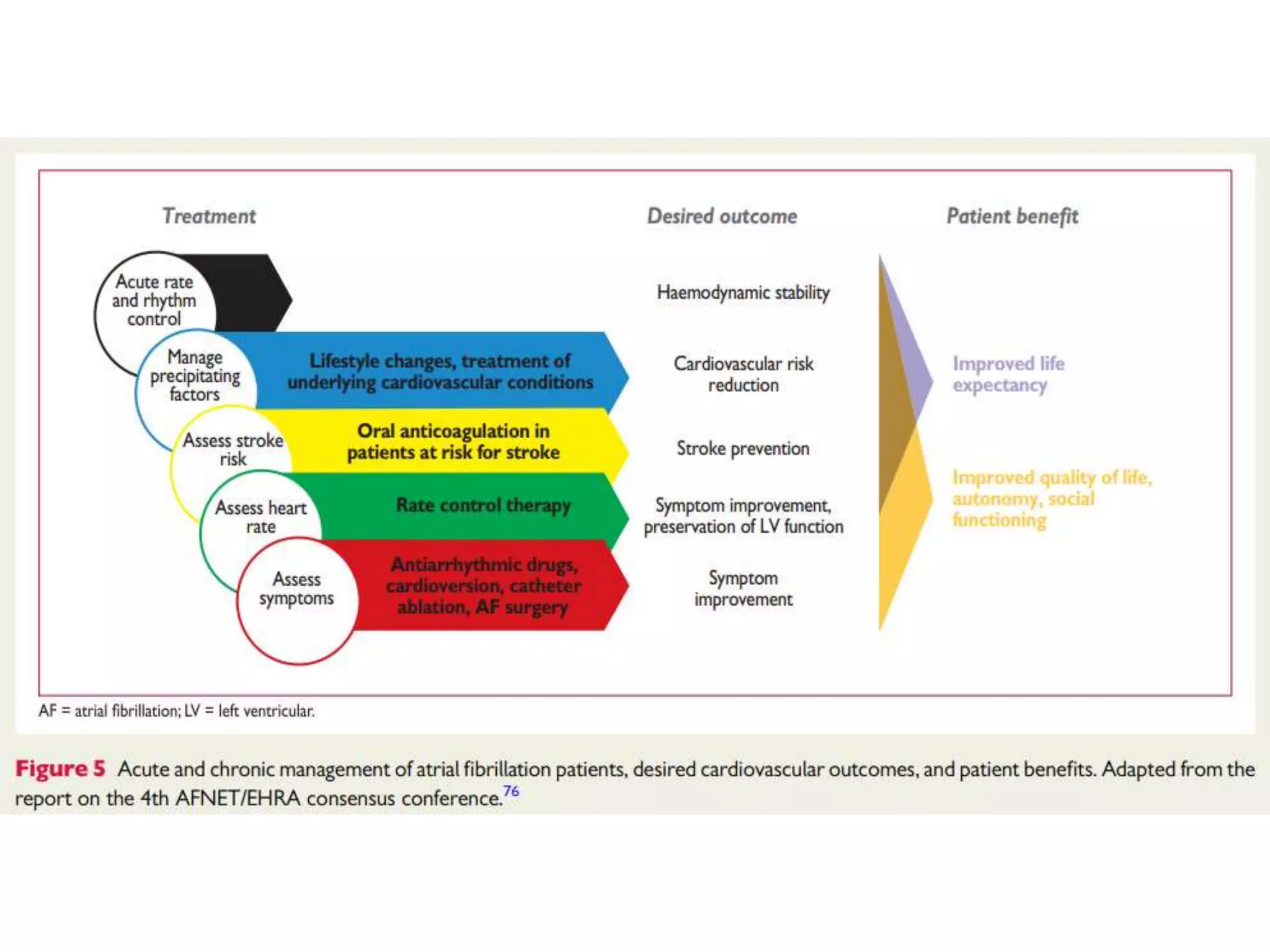
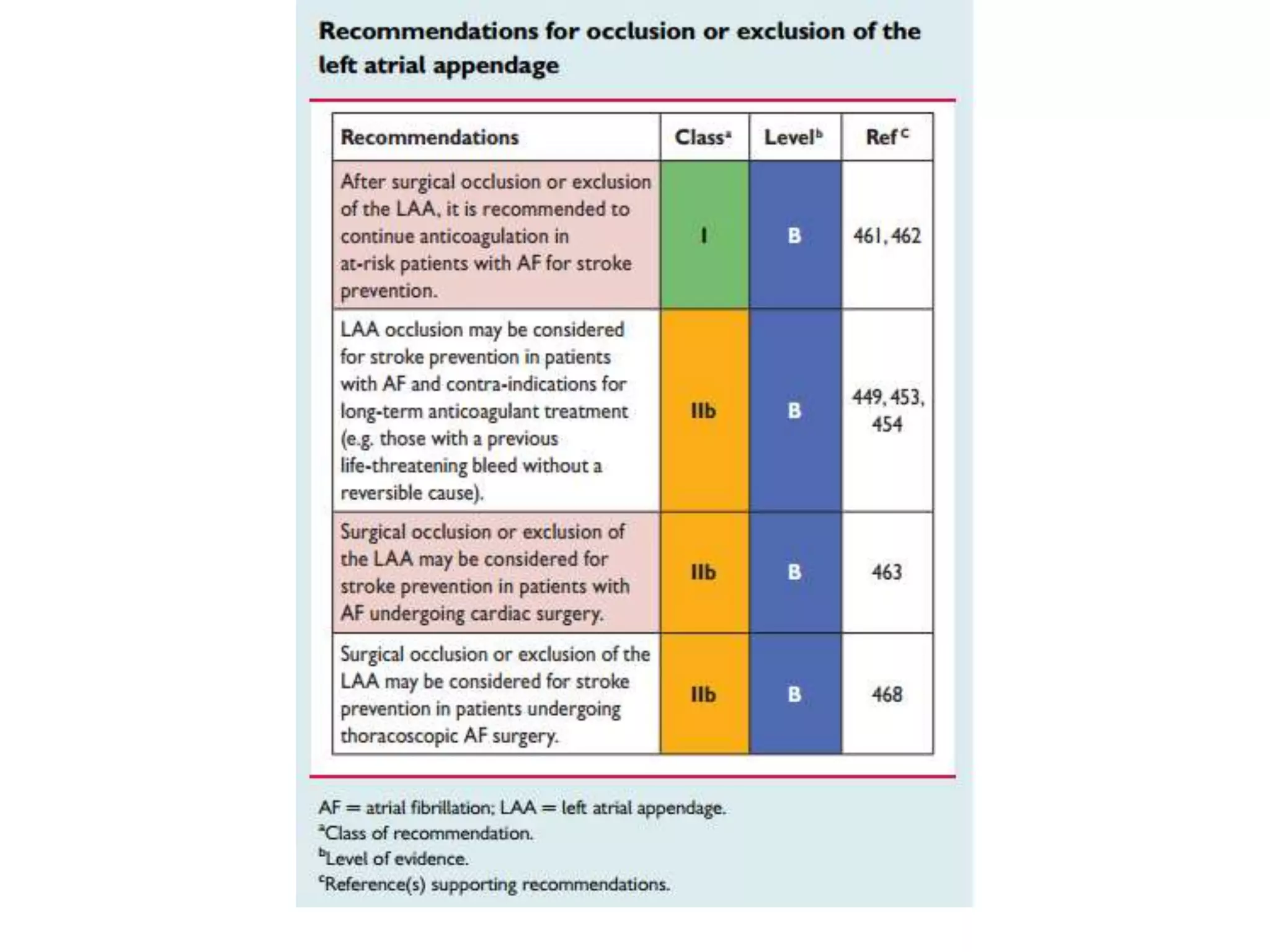
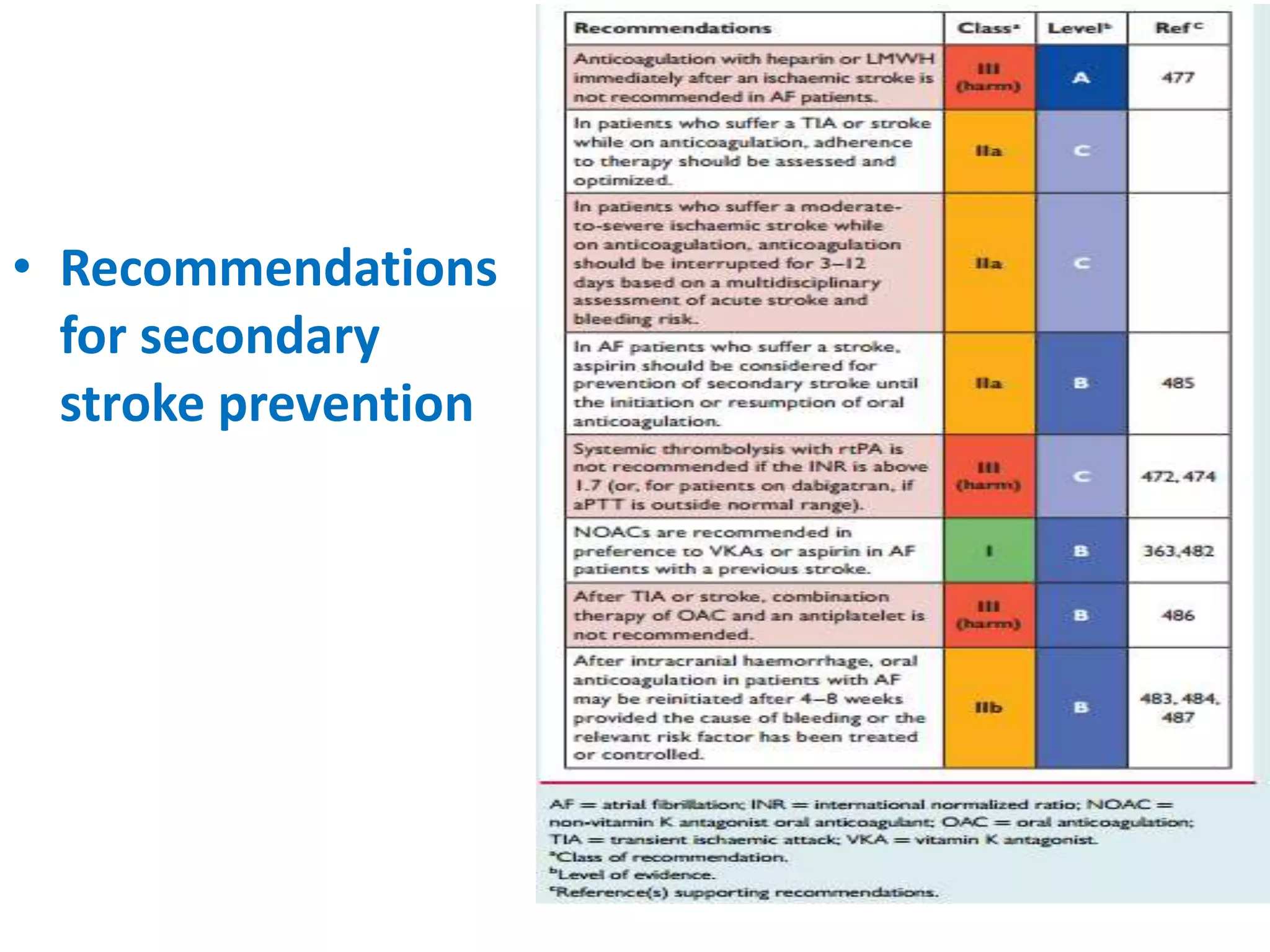
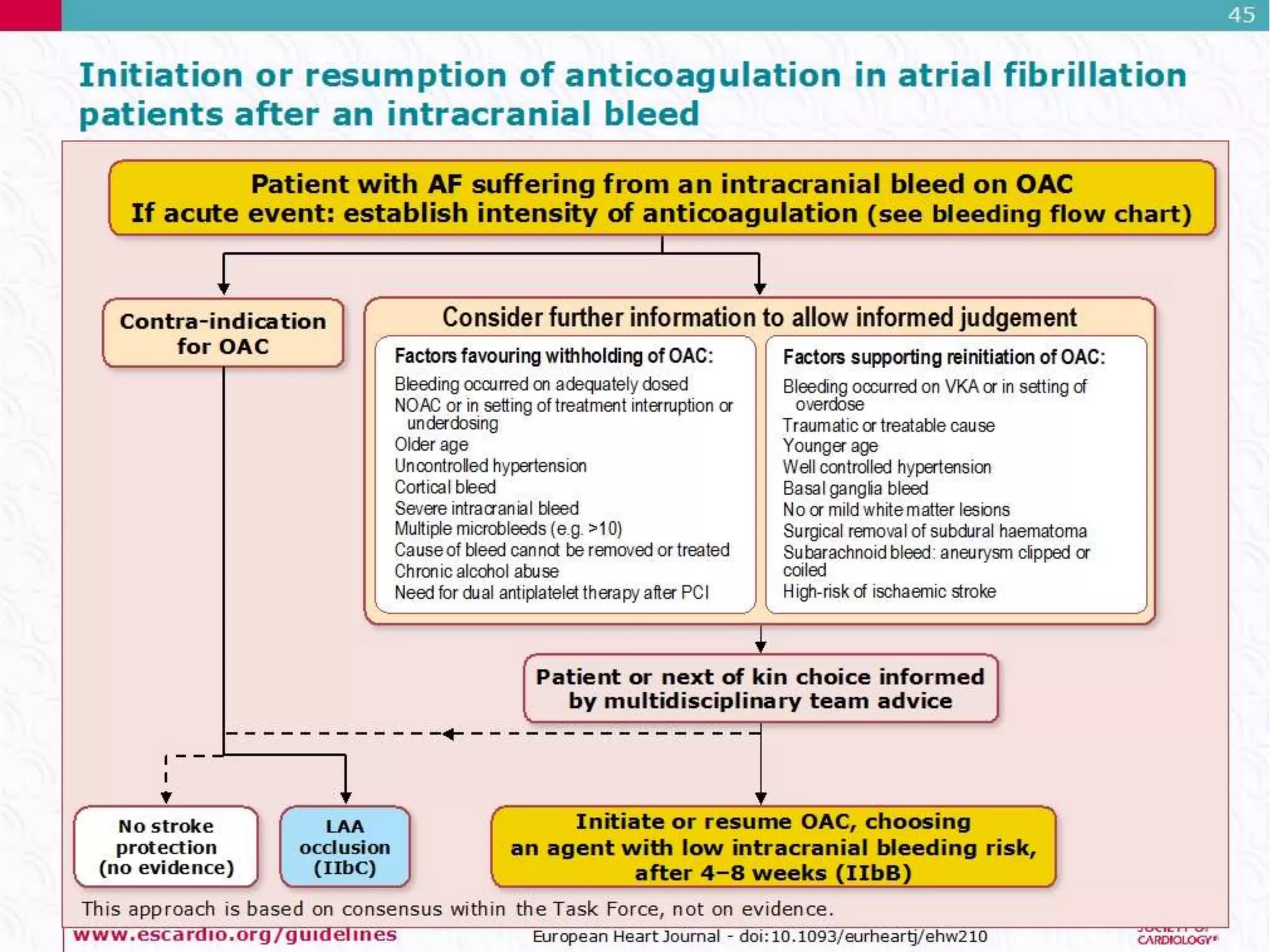
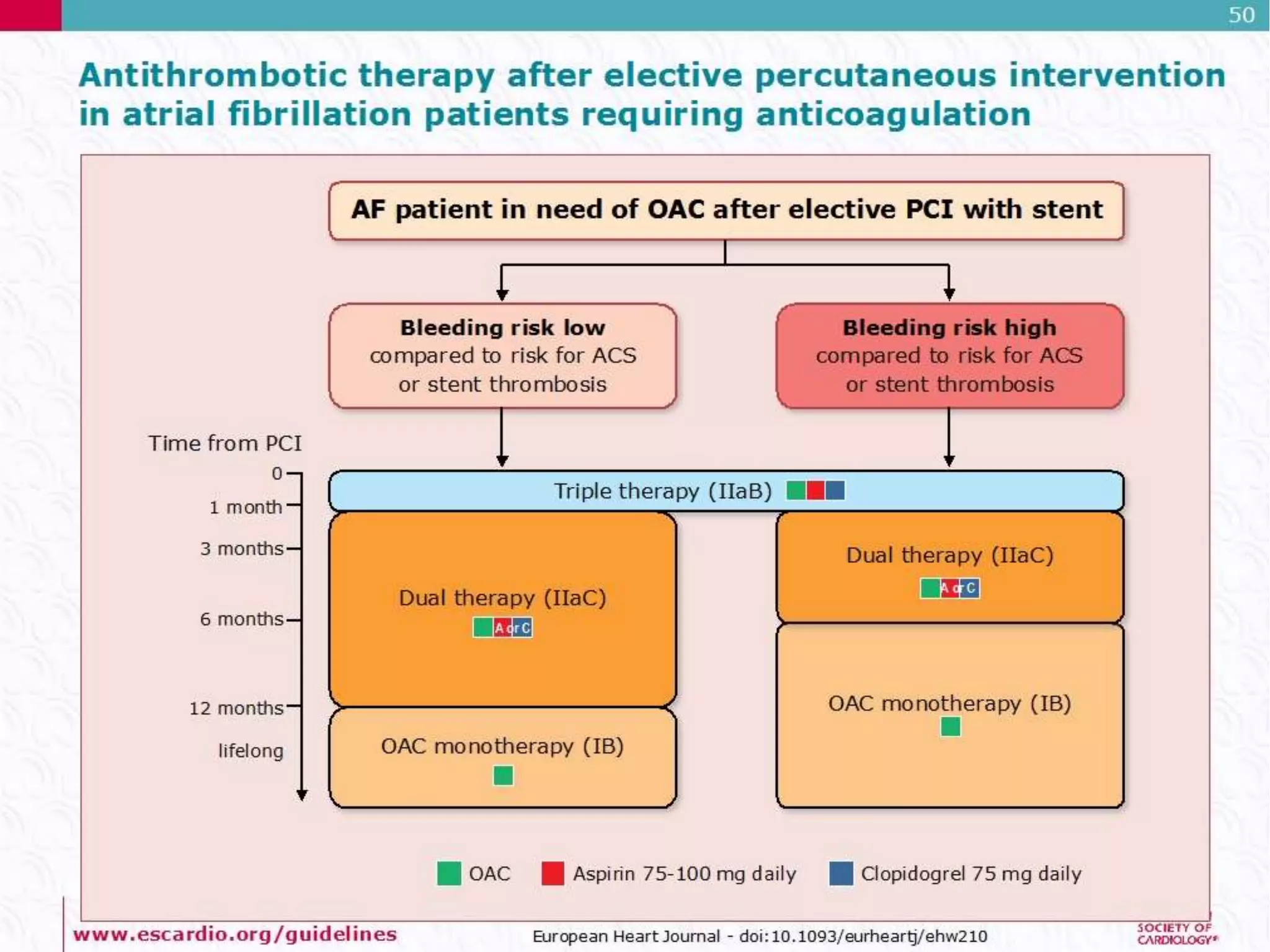
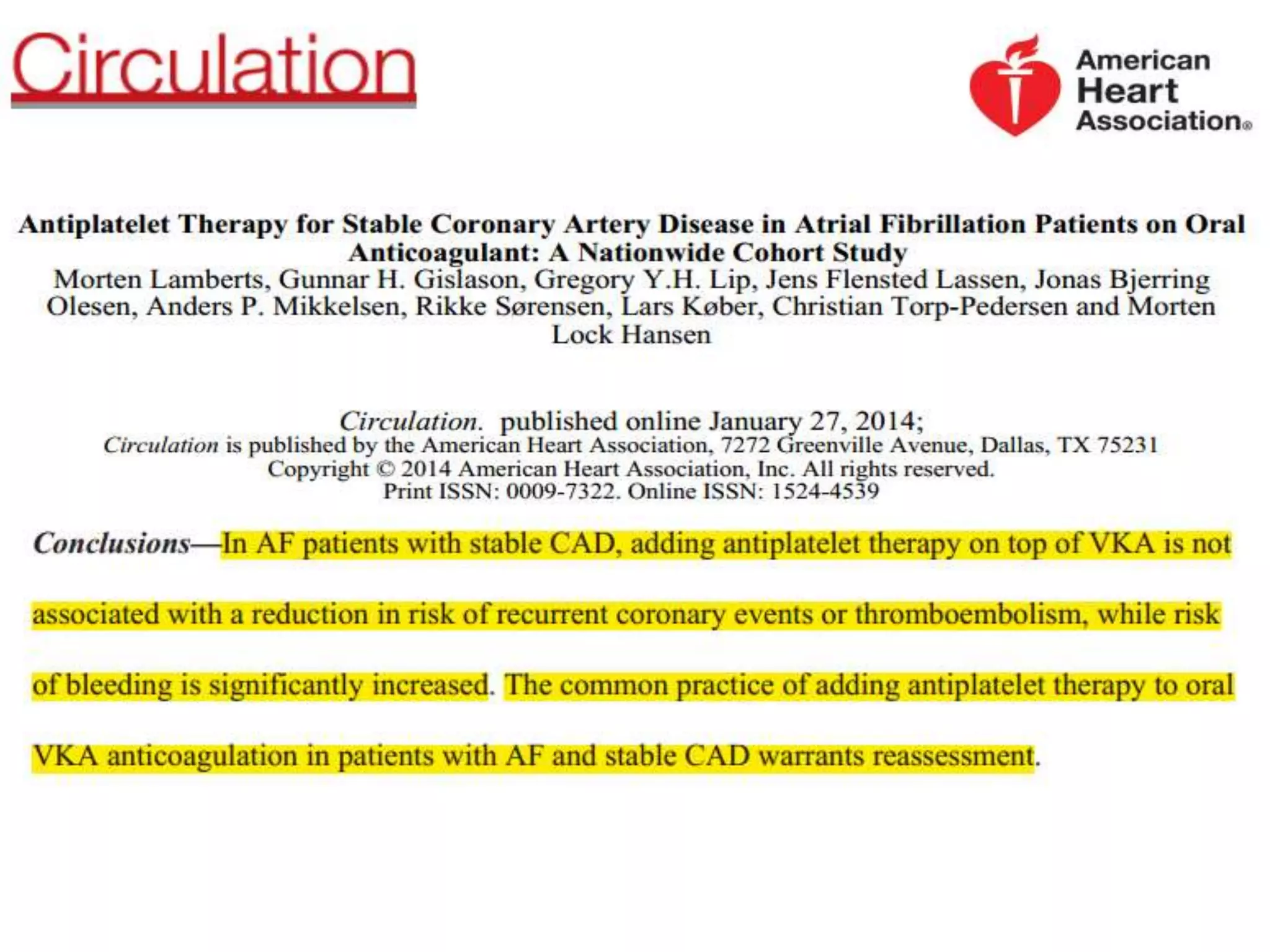
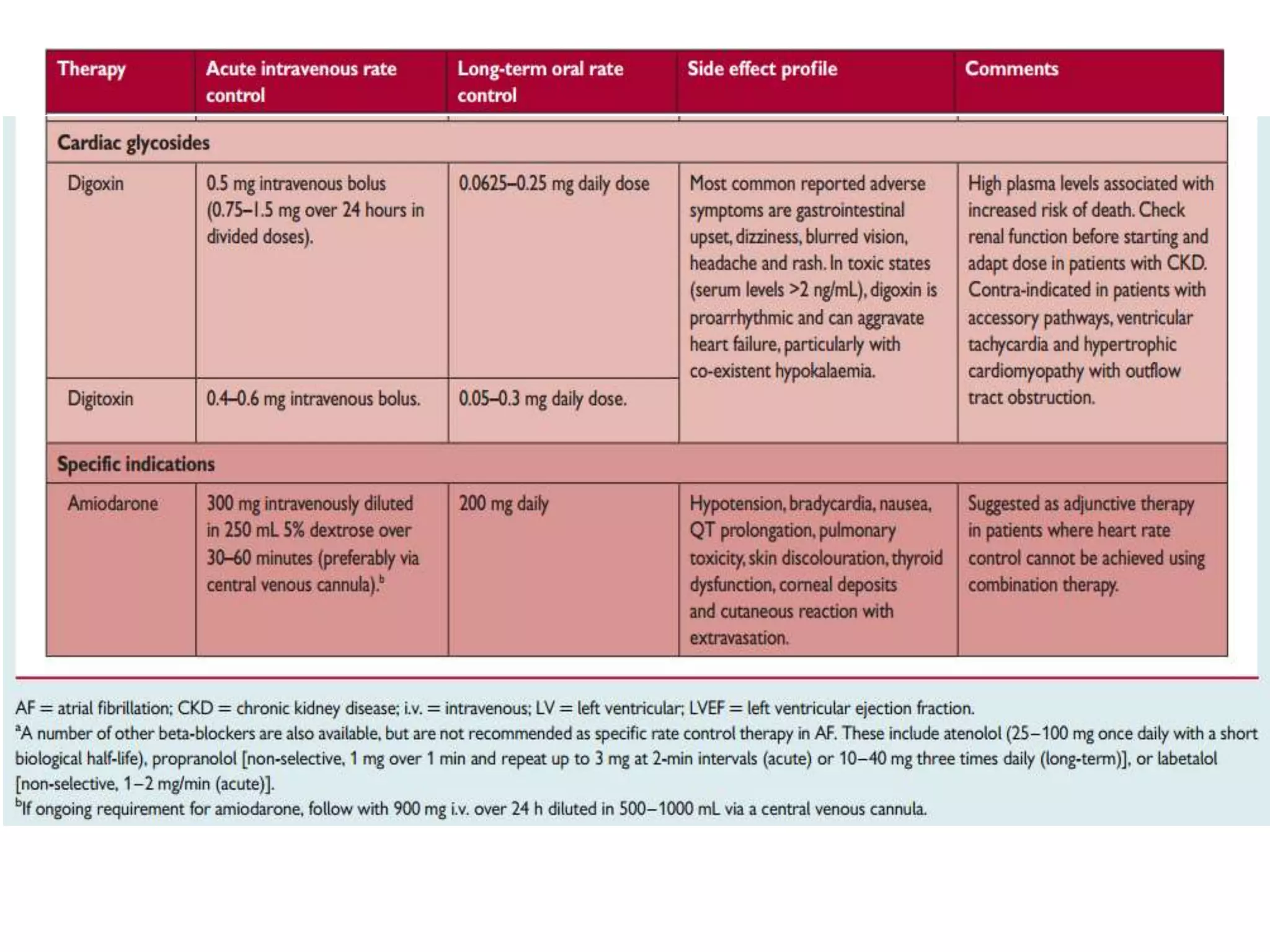
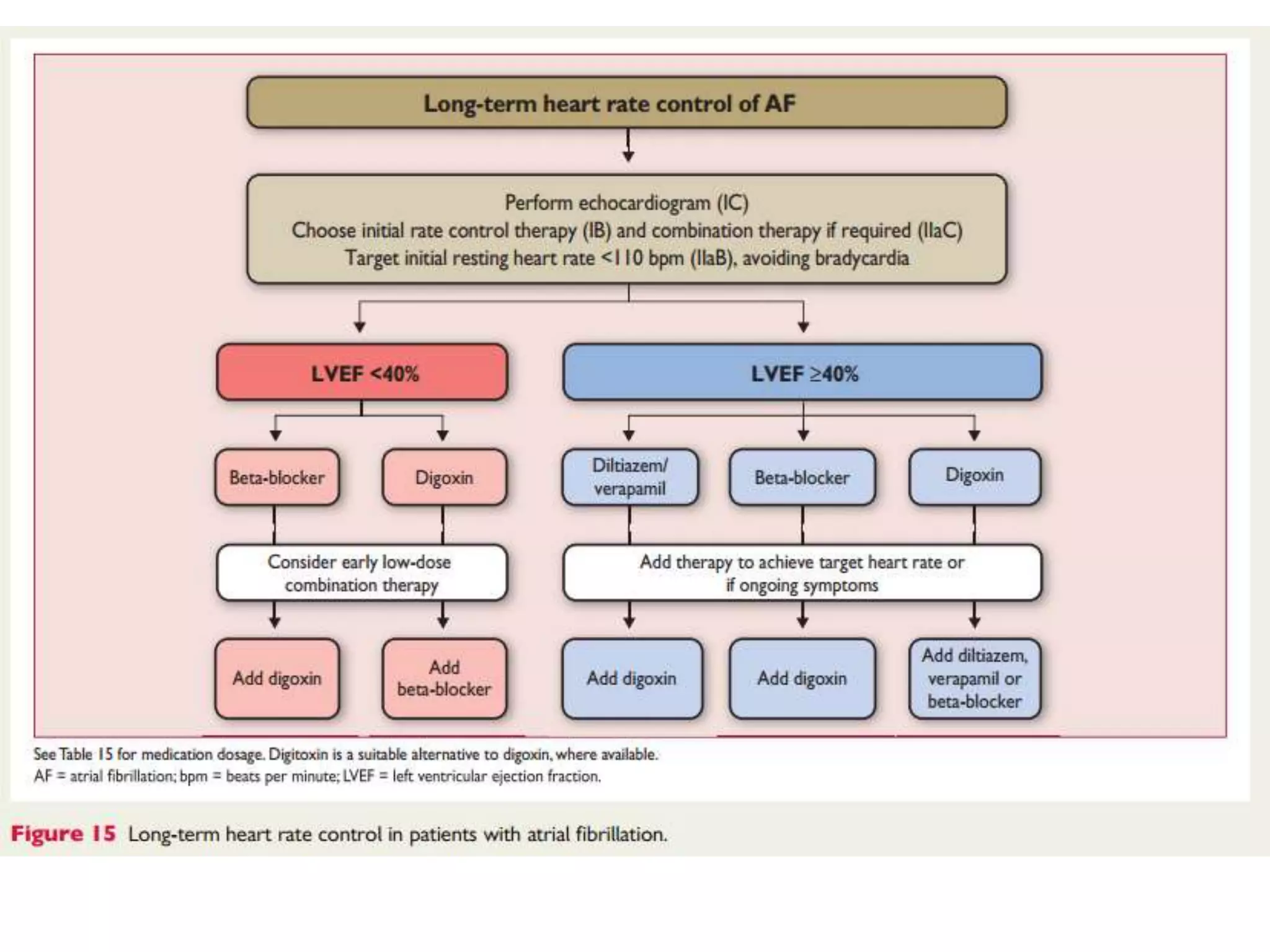
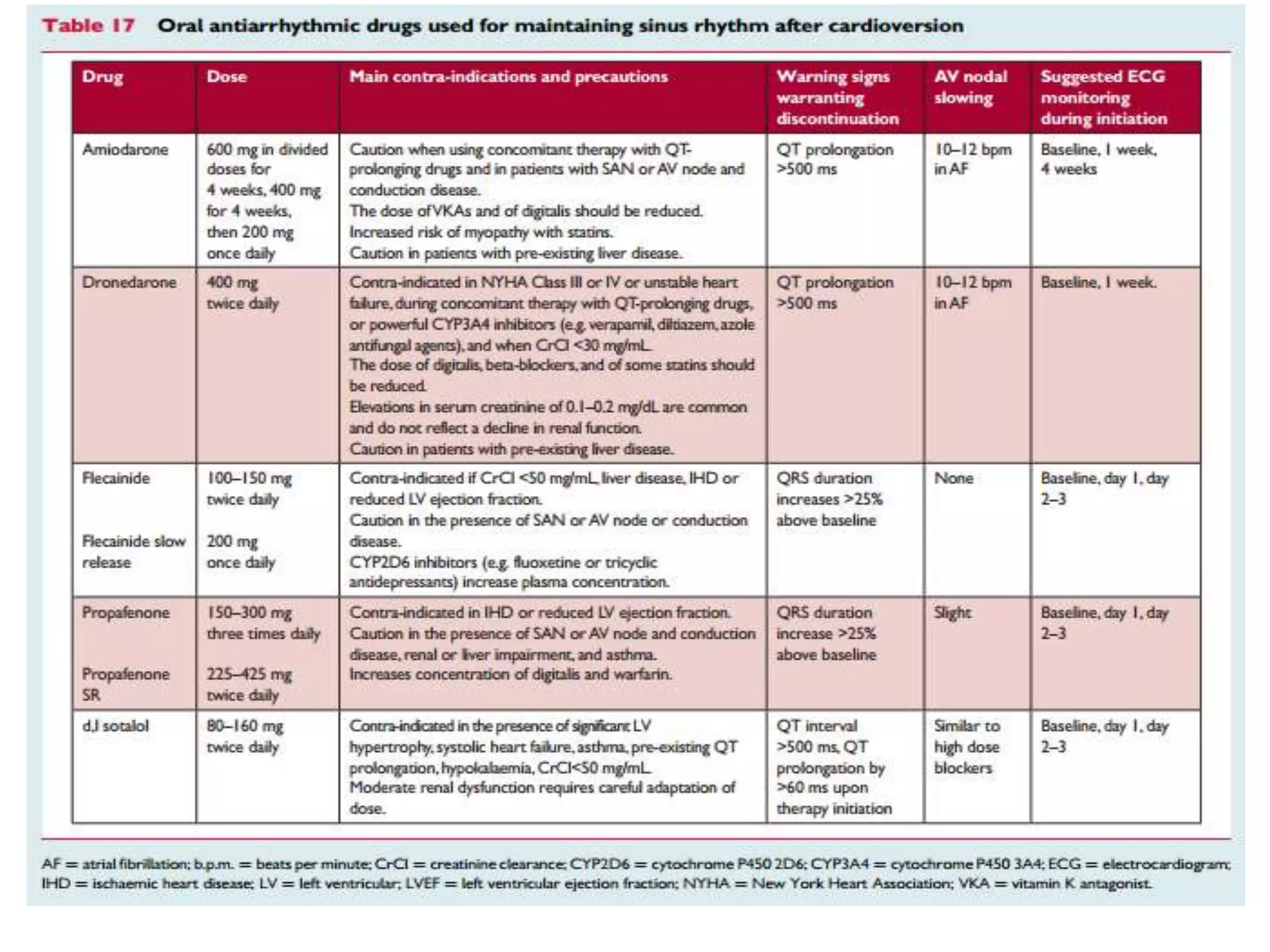
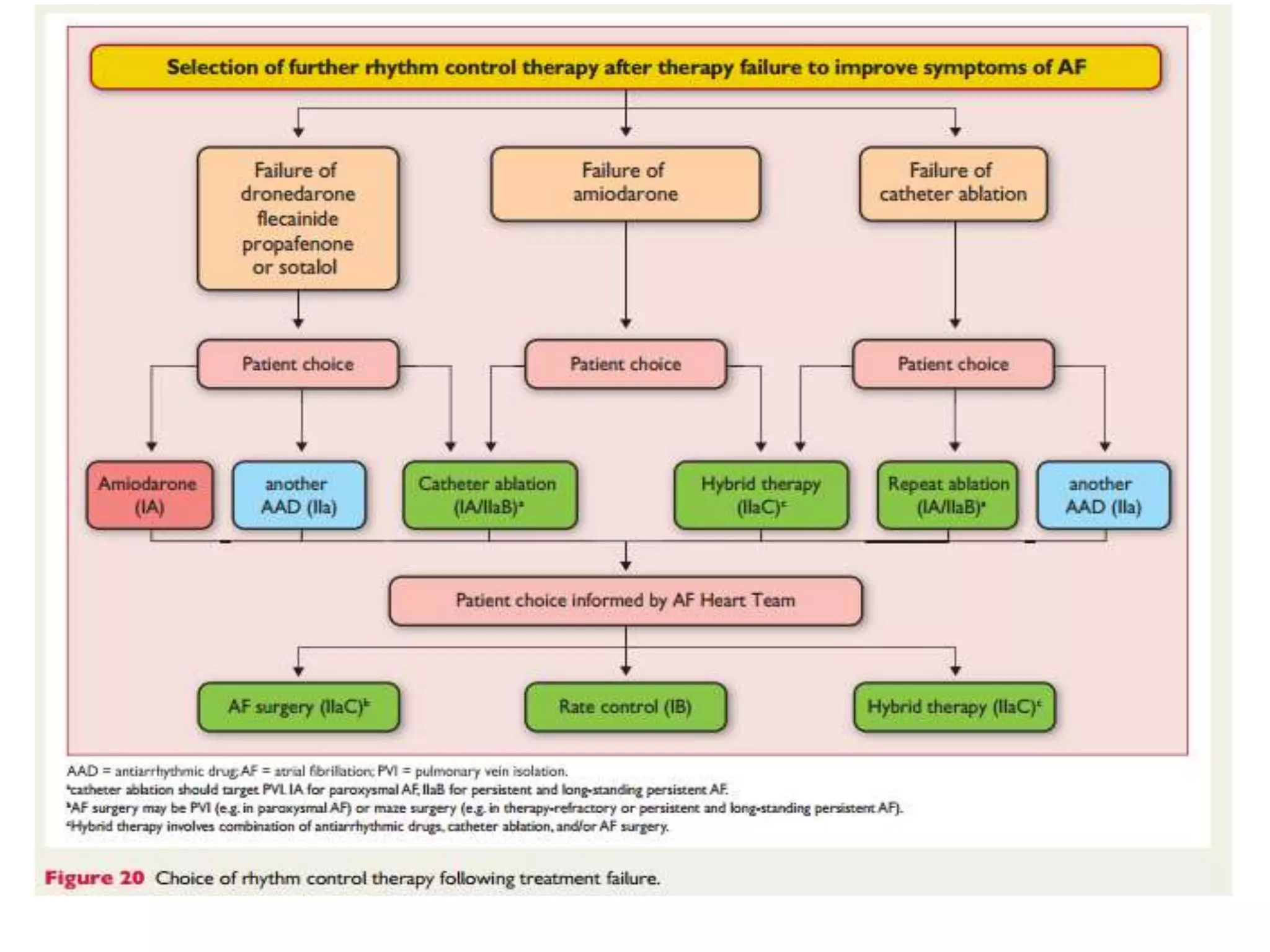
The document summarizes guidelines for managing atrial fibrillation. It discusses recommendations for stroke prevention using anticoagulants, rate control therapy, and rhythm control therapy. It also recommends catheter ablation of accessory pathways in Wolff-Parkinson-White syndrome patients with atrial fibrillation to prevent rapid conduction across pathways leading to dangerous arrhythmias.