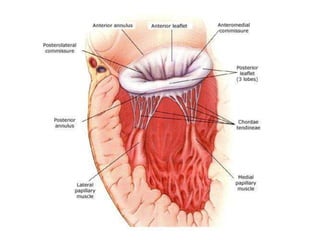
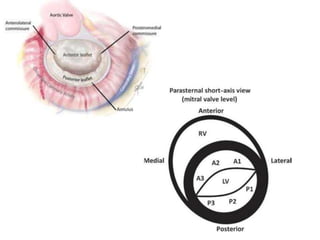
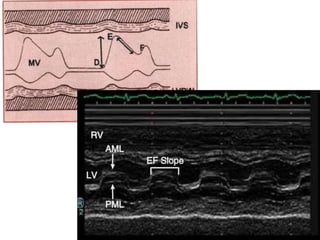
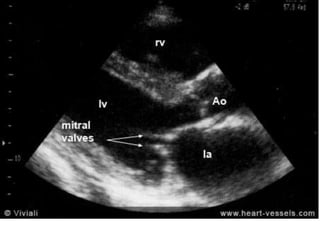
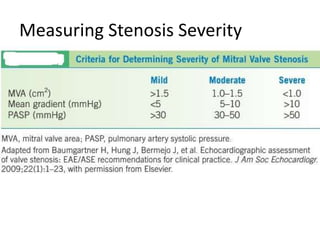
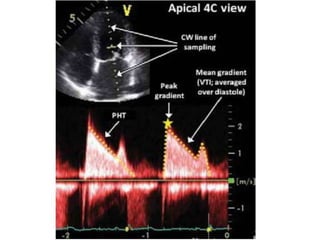
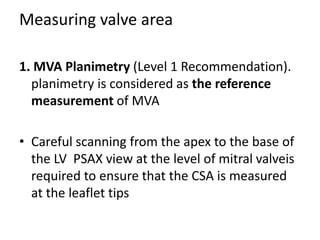
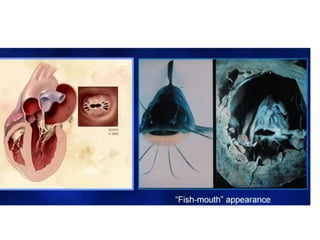
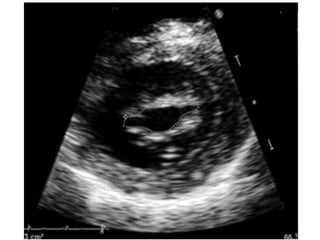
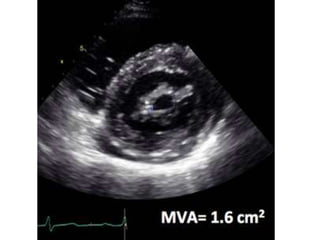
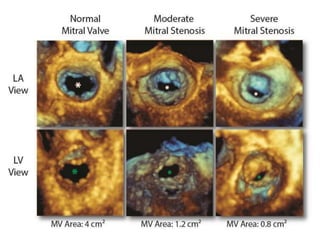
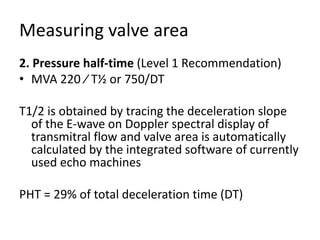
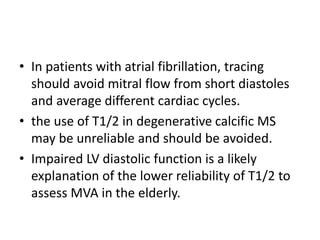
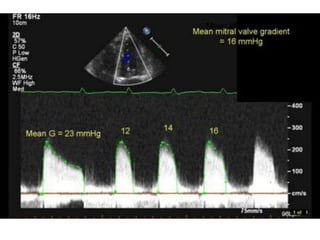
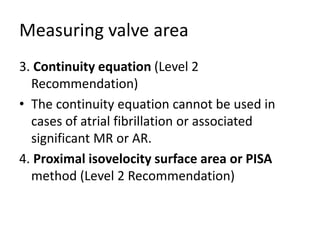
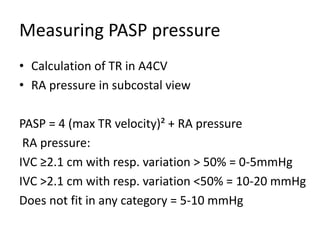
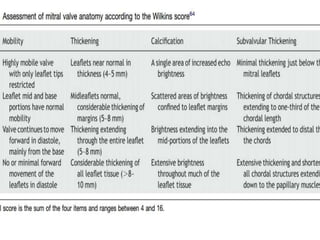
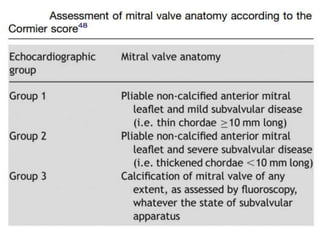
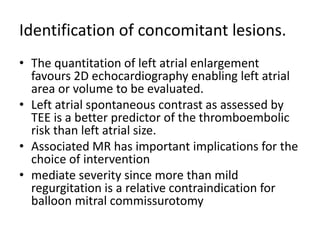
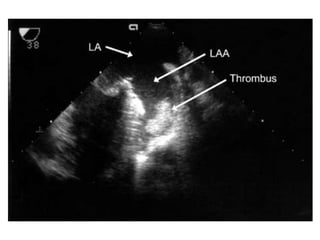
This document summarizes the echocardiographic assessment of mitral stenosis (MS). It describes the anatomy of the mitral valve and causes of MS. Methods for assessing MS severity include measuring the pressure gradient, mitral valve area using planimetry and pressure half-time, and pulmonary artery pressure. Suitability for percutaneous transvenous mitral commissurotomy is evaluated. Concomitant valve lesions are also identified. Stress echocardiography may be used when symptoms are equivocal. Transesophageal echocardiography is recommended in some cases.