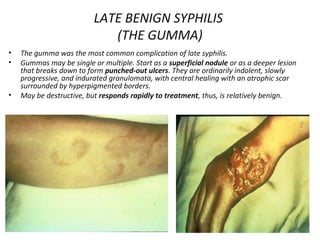
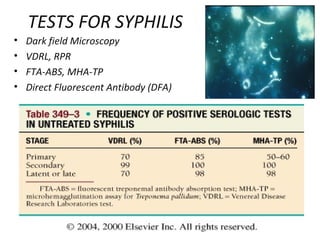
Syphilis is caused by the bacterium Treponema pallidum and is transmitted sexually, from mother to fetus, or rarely through other means. It progresses through primary, secondary, latent, and tertiary stages if left untreated. Primary syphilis presents as a painless chancre at the infection site while secondary syphilis causes a rash, fever, and mucous patches. Latent syphilis involves positive blood tests without symptoms. Tertiary syphilis can damage internal organs. Treatment involves penicillin or alternatives like doxycycline for non-pregnant patients and higher dose penicillin for pregnant patients and congenital cases.