Bacterial Vaginosis.pptx
- 2. OUTLINE 1. Introduction 2. Epidemiology 3. Risk Factors 4. Protective Factors 5. Etiology 6. Pathophysiology 7. Clinical Presentation 8. Differential diagnosis 9. Investigations 10. Treatment 11. Complication 12. Prevention 13. References
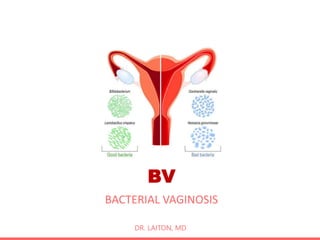
- 3. 1. INTRODUCTION Bacterial Vaginosis (BV) is a clinical condition characterized by a shift in vaginal flora away from lactobacillus species toward more diverse bacterial species including facultative anaerobes. Bacterial Vaginosis (BV) is not a sexual transmitted infection (STI). Other names of BV includes: Anaerobic Vaginositis, Non- specific Vaginitis, Vaginal Bacteriosis, and Gardnerella Vaginitis This condition was called Bacterial Vaginosis (not bacterial vaginitis) because it is caused by bacteria and inflammatory response is lacking. However, BV is the most common causes of vaginal infection.
- 4. 1. INTRODUCTION CONT. BV is the most common infection encountered in the outpatient gynaecological settings. Typical symptoms of Bacterial Vaginosis is thin, grey, homogenous vaginal discharge and fishy vaginal odour. Other symptoms which may be present are vulvar irritation, dysuria and dyspareunia. Wet Mount Microscopy showing clue cells on a saline smear is most specific criterion for diagnosis of Bacterial Vaginosis. Asymptomatic BV often resolve with treatment, however symptomatic BV is treatment using antibiotic therapy. Antibiotics which are mainly used are Metronidazole or Clindamycin.
- 5. 2. EPIDEMIOLOGY General population prevalence of BV is high globally ranging from 23% to 29% across regions. Black and Hispanic women have significantly higher prevalence compared to other racial groups. The estimated annual global economic burden treating symptomatic BV is US $4.8 billion. Economic burden of BV is increasing when including costs of BV-associated preterm births and HIV cases. BV Cases (26%) Non BV Cases (74%)
- 6. 3. RISK FACTORS Risk factors of BV are listed below: 1. Recent antibiotic use 2. Decreased estrogen production of the host 3. Wearing an IUCD 4. Douching, Tub baths, and Bubble baths 5. Intravaginal hygiene products 6. Liquid soaps and body washes 7. Sexual activity High frequency of sexual activity Multiple sexual partners Having new sexual partners Early Initiation of sexual intercourse
- 7. 3. RISK FACTORS Risk factors of BV are listed below (cont.): 8. Presence of other STIs 9. Prior Trichomoniasis 10. Cigarette smoking 11. Obesity 12. Being single/not married 13. Prior pregnancy 14. History of induced labour 15. Frequency use of sex toys 16. Frequency digital-vaginal sex 17. Frequency use of scented soap 18. Lesbians
- 8. 4. PROTECTIVE FACTORS Protective factors of BV are listed below: 1. Abstinence 2. Use of condoms 3. Hormonal contraception (combined and progestin only) 4. Cleaning sex toys between use 5. Use of gloves during digital-vaginal sex 6. Use of probiotics These protective factors play very minor role in reducing the risk of BV. Few studies have been conducted, there is no enough data to be conclusive.
- 9. 5. ETIOLOGY • BV is known to be synergistic polymicrobial infection. • Gardnerella vaginalis is thought to have a leading role in the infection, although the correct aetiology is unknown. • Other associated bacteria includes: 1. Prevotella 2. Anaerobes Mobiluncus Bacteroides Peptostreptococcus Fusobacterium Veillonella Eubacterium 3. Mycoplasma hominis 4. Ureaplasma urealyticum 5. Streptococcus viridans 6. Atopobium vaginae
- 10. 6. PATHOPHYSIOLOGY The exact pathogenesis of BV is not fully understood. BV is thought to be result of a shift in vaginal flora from lactobacillus species towards more diverse of bacterial species including facultative anaerobes. The shift of vaginal flora causes a reduction in the hydrogen peroxide-producing lactobacilli, this leads to an increase in the vaginal pH and overgrowth of Gardnerella vaginalis and anaerobes. Decrease in pH facilitates: – Adherence of Gardnerella vaginalis to the exfoliating epitheal cells making clue cells and – Formation of Gardnerella vaginalis biofilms which can survive hydrogen peroxide, lactic acid, and high level of antibiotics.
- 11. 6. PATHOPHYSIOLOGY CONT. • Anaerobes produce large amount of proteolytic carboxylase enzymes which break down vaginal peptides into variety of amines that are volatile, malodorous, and associated with increased vaginal transudation. • Production of amines causes further reduction of lactobacilli which leads to more increase of vaginal pH. • Anaerobes (mobiluncus) produce amine called trimethylamine giving the smell of rotting fish. • Anaerobes also produce succinate (keto-acid). Production of succinate and absence of lactic acid blunt the chemotactic response of polymorphinuclear leucocytes reducing their killing ability. • This explains absence of cellular inflammatory response.
- 13. 7. CLINICAL PRESENTATION - HISTORY More than 50% of women diagnosed with BV are asymptomatic. Symptoms of BV include the following: 1. Vaginal odour Most common and often initial symptom of BV. Odour may be recognized only after sexual intercourse. The alkalinity of semen may cause a release of volatile amines from the vaginal discharge and cause a fishy odour. 2. Increased vaginal discharge Vaginal discharge are usually thin, homogenous, whitish-grey. 3. Vulvar irritation is less common 4. Dysuria and dyspareunia occur rarely
- 14. 7. CLINICAL PRESENTATION – P.E. • Physical Examination is mainly done by Inspection and Speculum Examination. • Physical Examination findings include: 1. Vaginal discharge features include the following: Most often gray, thin, and homogeneous Adherent to the vaginal mucosa Small bubbles in the discharge fluid () No pooling of discharge in the posterior fornix () 2. An increased light reflex of the vaginal walls may be observed, indicating very wet appearance. 3. No or little evidence of inflammation of vaginal walls. 4. The labia, introitus, cervix, and cervical discharge appear normal. 5. Any evidence of Cervicitis, check for STIs.
- 15. COLOR OF VAGINAL DISCHARGE COLOR INTERPRETATION WHITE Healthy Yeast Infection YELLOW TO GREEN Sexual Transmitted Infection Trichomoniasis PINK TO RED Menstruation or Implant bleeding Cervical Infection or Cervical Polyp Endometrial or cervical cancer Vaginal irritation GRAY Bacterial Vaginosis CLEAR Healthy Ovulation Pregnancy Hormonal Imbalance
- 16. 8. DIFFERENTIAL DIAGNOSIS For atypical clinical features of BV, the possibility of a coinfection is high, such as Vaginal Candidiasis, Trichomoniasis, Chlamydia infection, Gonorrhoeae, HSV infection, or an alternative diagnosis. Differential diagnosis are as follows: 1. Candidiasis 2. Cervicitis 3. Chlamydial Genitourinary Infections 4. Gonorrhoea 5. HSV Infection 6. Trichomoniasis 7. Vaginal Candidiasis 8. Vaginitis
- 17. 8. DIFFERENTIAL DIAGNOSIS Vaginitis Normal pH Infectious - Vulvovaginal Candidiasis - HSV infection Non-infectious - Vulvodynia - Dermatosis - Dermatitis - Physiologic leucorrhoea Abnormal pH Infectious - Bacterial Vaginosis - Trichomoniasis - Cervicitis Non-infectious - Blood - Semen - Cervical mucus - Amniotic fluid - Vaginal atrophy - Lichen Planus - Desquamative Inflammatory vaginitis
- 18. 9. INVESTIGATIONS Specimen of choice is vaginal discharge. The collection of specimen for diagnosis is ideally performed during a comprehensive pelvic examination using a speculum. During speculum examination, an evaluation of the discharge is made by clinician. Specimen is collected from the lateral vaginal wall and posterior fornix with a sterile swab. There are two main categories of diagnostic tests for BV: 1. Clinical Criteria (Amsel’s criteria) 2. Laboratory-based testing (Nugent scoring)
- 19. 9. INVESTIGATIONS CONT. The following are investigations done in BV: 1. Macroscopic Examination 2. Vaginal pH 3. Whiff Test 4. Microscopic Examination Saline Wet Mount (Clue Cells Test) Gram stain Evaluation of bacteria flora 5. Vaginal Culture 6. Diagnostic Tools 7. Quantitative PCR
- 20. 9. INVESTIGATIONS CONT. 1. Macroscopic Examination This is done during speculum examination, an evaluation of the discharge is made by clinician. Typical features of BV vaginal discharge will be seen (as mentioned on Physical Examination). 2. Vaginal pH Test The use of pH sticks placed on the vaginal wall or The use of a swap which is touched on pH paper. Vaginal pH > 4.5 in 90% of BV cases. 3. Whiff Test A drop of 10% potassium hydroxide is placed on a glass slide. The swab is then stirred in the 10% KOH and immediate evaluate for a fishy odour. Fishy odour means positive result. It is usually positive in 70% of BV cases.
- 21. 9. INVESTIGATIONS CONT. 4. Microscopic Examination A. Saline Wet Mount The swab is immersed into 0.2mL of physiological saline and put on a glass slide. Glass slide is covered with a coverslip and examined at 400 magnification with a light microscope. Clue cells are identified, that is positive result. Clue cells are vaginal epitheal cells covered with bacteria (coccobacilli) that the peripheral borders are obscured.
- 22. 9. INVESTIGATIONS CONT. AMSEL CRITERIA FOR DIAGNOSIS OF BV: Amsel Criteria is the most widely accepted clinical criteria used in diagnosis of BV. This clinical diagnosis requires that at least three of the following four criteria to be met: 1. Homogenous, thin, greyish-white discharge 2. Vaginal pH > 4.5 3. Positive whiff-amine test 4. Presence of clue cells in the vaginal fluid
- 23. 9. INVESTIGATIONS CONT. 4. Microscopic Examination B. Gram stain Specimen on the slide is stained by standard methods, the stained slide is read, and number of morphotypes are evaluated based on a standardized scoring method. The current standard scoring method used is Nugent scoring of gram stained smear for bacterial vaginosis.
- 24. 9. INVESTIGATIONS CONT. SCORE Lactobacillus morphotype per field Gardnerella morphotype per field Curved Bacteria (mobiluncus) per field 0 >30 0 0 1 5 – 30 <1 1 – 5 2 1 – 4 1 – 4 >5 3 <1 5 – 30 4 0 >30 NUGENT SCORING OF GRAM STAINED SMEAR FOR BACTERIAL VAGINOSIS: INTERPRETATION OF NUGENT SCORE: 0 – 3: Normal 4 – 6: Intermediate, repeat test later 7 – 10: Bacterial Vaginosis
- 26. 9. INVESTIGATIONS CONT. 4. Microscopic Examination C. Microscopic Evaluation of the bacteria flora This is done to examine the evidence of changes in overall bacterial predominance. The healthy vagina has a predominance of lactobacilli (large gram-positive rods). The flora of a patient with BV changes to become dominated by coccobacilli, reflecting an increase in growth of Gardnerella vaginalis and other anaerobes. No PMNs are observed.
- 27. 9. INVESTIGATIONS CONT. 4. Vaginal Culture Vaginal culture is not done routinely and has no utility. G vaginalis is 100% of vaginal culture of symptomatic BV and 70% of vaginal cultures of asymptomatic BV. Vaginal cultures helps to exclude other infectious aetiologies such as Trichomonas spp, C trachomatis, and N gonorrhoea. In recurrent BV cases that have not resolved with standard regimens, cultures may be appropriate. 5. Diagnostic tools FemExam is one of diagnostic tool, not used a lot due to variable in sensitivity (38 - 90%) and specificity (12.5 – 97%). There are other female self-test cards in the market. 6. Quantitative PCR It is useful in the evaluation of BV treatment response and the risk of preterm birth in pregnant women.
- 28. 9. INVESTIGATIONS CONT. Examples of Vaginitis Self-Test Kit in the market
- 29. Clinical Elements Bacterial Vaginosis Trichomoniasis Vaginal Candiasis Symptoms Vaginal odour + +/- - Vaginal discharge Thin, gray, homogenous Green-yellow White curdlike Vulvar irritation +/- + + Dyspareunia - + - Signs Vulvar erythema - +/- +/- bubbles in vaginal fluid + +/- - Strawberry cervix - +/- - Microscopy Saline wet mount Clue cells + - - Motile protozoa - + - KOH test Pseudohyphae - - + Whiff test + +/- - pH > 4.5 > 4.5 < 4.5 Differences between Infectious Vaginitis:
- 30. 10. TREATMENT Benefits of Treatment includes: 1. Relief of symptoms 2. Reduction of postoperative infection 3. Reduction of the risk of acquiring STIs Inpatient care is not necessary for patient with BV. Surgery is not indicated for BV. Antibiotics are the mainstay of therapy for BV, mainly Metronidazole and Clindamycin. Alternative antibiotics are Tinidazole and Secnidazole. Asymptomatic women with confirmed BV do not need treatment. Uncomplicated cases typically resolve after standard antibiotic treatment .
- 31. 10. TREATMENT CONT. Treat BV occurring in pregnant women to reduce the risk of pregnancy-associated complications related to infection. Treatment before transvaginal procedures, caesarean delivery, total abdominal hysterectomy, or insertion of an IUD is also recommended. Studies of topically applied and orally administered yogurt or lactobacilli preparations and probiotics, which are used to help re-establish the lactobacilli population in the vagina, have demonstrated inconsistent results. BV that does not resolve after one course of treatment may be cured by giving a second course of the same agent or by switching to another agent.
- 32. 10. TREATMENT CONT. Some women with recurrent BV may benefit from evaluation or treatment of G vaginalis colonization in their sexual partner (controversial). Testing for other infections (e.g., N gonorrhoeae, C trachomatis, or herpes simplex virus infection) may be appropriate . Therapy with metronidazole or clindamycin may alter the vaginal flora and predispose the patient to development of vaginal candidiasis . ON THE NEXT PAGES IS THE ALGORITHM OF THE INITIAL TREATMENT OF BV
- 33. 10. INITIAL TREATMENT OF BV Has the diagnosis been confirmed based on any of the following: 1. Amsel Criteria 2. Gram stain 3. Commercial Test Does the patient have symptoms? OR Is the patient about to have a transvaginal surgery or procedure? Test before treating YES NO
- 34. 10. INITIAL TREATMENT OF BV Does the patient have symptoms? (vaginal discharge + vaginal odour) OR Is the patient about to have a vaginal surgery or procedure? Is the individual pregnant or lactating? Observe and do not treat: BV often resolves without treatment Treatment with antibiotics can result in vaginal yeast infections YES NO
- 35. 10. INITIAL TREATMENT OF BV • Oral Metronidazole 500 mg BID for 7 days OR • Vaginal metronidazole 0.75% gel 5 g OD for 5 days OR • Vaginal Clindamycin 2% cream 5 g OD for 7 days Neither • Oral Metronidazole 500 mg BID for 7 days OR • Oral Metronidazole 250 mg TID for 7 days OR • Oral Clindamycin 300 mg BID for 7 days Pregnant • Oral Metronidazole 500 mg BID for 7 days OR • Oral Clindamycin 300 mg BID for 7 days Lactating
- 36. 10. TREATMENT CONT. For further understanding, treatment session is further divided into the following: A. Nonpregnant symptomatic patients B. Nonpregnant asymptomatic patients C. Pregnant symptomatic patients D. Pregnant asymptomatic patients E. Lactating patients F. Patients undergoing gynaecologic procedures G. Sexual partner of patient with confirmed BV H. Recurrent BV patients
- 37. 10. TREATMENT CONT. A. NONPREGNANT SYMPTOMATIC PATIENTS: Nonpregnant symptomatic patient are treated by oral or vaginal formulations of Metronidazole and Clindamycin. Many patients consider oral medication to be more convenient than vaginal dosing, but oral medication causes more systemic side effects, such as headache, nausea, abdominal pain, and Clostridioides. Oral metronidazole is commonly used, and metronidazole is less commonly associated with Clostridioides difficile infection compared with clindamycin. Alternative medications includes Tinidazole and Secnidazole.
- 38. 10. TREATMENT CONT. A. NONPREGNANT SYMPTOMATIC PATIENTS: DRUG OF CHOICE Metronidazole 500 mg PO BID for 7 days OR Metronidazole 0.75% gel 5 g PV OD for 5 days OR Clindamycin 2% cream 5 g PV OD (at bedtime) for 7 days ALTERNATIVE THERAPY Clindamycin 300mg PO BID for 7 days OR Clindamycin ovule 100mg PO OD for 3 days OR Tinidazole 2 g PO 0D for 2 days OR Tinidazole 1 g PO 0D for 5 days OR Secnidazole 2 g packet PO single dose
- 39. 10. TREATMENT CONT. B. NONPREGNANT ASYMPTOMATIC PATIENTS: Nonpregnant asymptomatic patients do not require antibiotic treatment. Treatment is typically avoided since patients often spontaneously improve over a period of time and any antibacterial therapy can be followed by symptomatic vaginal yeast infection. Exception: 1. Patients undergoing gynaecologic procedures or surgery that involved the vagina. 2. Patients more susceptible to acquiring STIs including HIV and HSV infection (controversial).
- 40. 10. TREATMENT CONT. C. PREGNANT SYMPTOMATIC PATIENTS: Pregnant individuals with symptomatic BV are treated to relieve bothersome symptoms. Oral therapy is preferred because some data indicate oral treatment is more effective against potential subclinical upper genital tract infection. Some guidelines allow the use of oral and vaginal formulations same as nonpregnant symptomatic patients. Example: CDC Guideline. Metronidazole should be avoided during the first trimester because it can cross the placenta and become tetratogenic (controversial).
- 41. 10. TREATMENT CONT. C. PREGNANT SYMPTOMATIC PATIENTS: DRUG OF CHOICE Metronidazole 500 mg PO BID for 7 days OR Metronidazole 250 mg PO TID for 7 days OR Clindamycin 300mg PO BID for 7 days TOPICAL THERAPY Metronidazole 0.75% gel 5 g PV OD for 5 days OR Clindamycin 2% cream 5 g PV OD (at bedtime) for 7 days
- 42. 10. TREATMENT CONT. D. PREGNANT ASYMPTOMATIC PATIENTS: Asymptomatic pregnant individuals are recommended to be treated to reduce the risk of pregnancy-associated complications related to infection (controversial). Asymptomatic pregnant individuals with previous preterm births may benefit from treatment. When treatment is indicated, oral therapy is used. Trials suggest that oral clindamycin given early in pregnancy is an effective therapy. Topical clindamycin given in the second half of pregnancy is less effective and even associated with an increase in low birth weight and neonatal infection.
- 43. 10. TREATMENT CONT. D. PREGNANT ASYMPTOMATIC PATIENTS: DRUG OF CHOICE Metronidazole 500 mg PO BID for 7 days OR Metronidazole 250 mg PO TID for 7 days OR Clindamycin 300mg PO BID for 7 days Metronidazole should be avoided during the first trimester because it can cross the placenta and become tetratogenic (controversial). Topical clindamycin given in the second half of pregnancy is less effective and even associated with an increase in low birth weight and neonatal infection.
- 44. 10. TREATMENT CONT. E. LACTATING PATIENTS: Lactating individuals with confirmed BV and symptoms are offered treatment while asymptomatic individuals do not require treatment as asymptomatic BV can resolve, just like in nonpregnant individuals. The preferred treatment for lactating individuals is: Metronidazole 500 mg PO BID for 7 days Oral clindamycin is a reasonable therapeutic choice, however clindamycin has the potential to cause adverse effects on the breastfed infant's gastrointestinal flora. Infants of patients treated with oral clindamycin should be monitored for diarrhoea, candidiasis (thrush, diaper rash) or rarely blood in the stool indicating possible antibiotic-associated colitis.
- 45. 10. TREATMENT CONT. E. LACTATING PATIENTS: Maternal metronidazole use is linked to more loose stools and more candidal colonization in metronidazole- exposed infants. It is recommended that maternal receiving the 2-gram one-time dose, should interrupt breastfeeding, express and discard their milk for 12 to24 hours. For lactating individuals who are administered Tinidazole or Secnidazole, interruption of breastfeeding is recommended during treatment and for three days after the last dose.
- 46. 10. TREATMENT CONT. E. LACTATING PATIENTS: DRUG OF CHOICE Metronidazole 500 mg PO BID for 7 days OR Clindamycin 300mg PO BID for 7 days TOPICAL THERAPY Metronidazole 0.75% gel 5 g PV OD for 5 days OR Clindamycin 2% cream 5 g PV OD (at bedtime) for 7 days ALTERNATIVE THERAPY (INTERRUPT BF) Tinidazole 2 g PO 0D for 2 days OR Tinidazole 1 g PO 0D for 5 days OR Secnidazole 2 g packet PO single dose
- 47. 10. TREATMENT CONT. F. GYNAECOLOGIC PROCEDURE OR SURGERY: For individuals with confirmed BV (with or without symptoms), antibiotic treatment is given prior to transvaginal procedures or surgery to prevent postprocedure infection (cuff infection after hysterectomy, endometritis after termination). The medication treatment options are the same as for symptomatic nonpregnant females. Transvaginal procedures or surgery includes pregnancy termination, dilation and curettage, hysterectomy, insertion of an IUD. Treatment before caesarean delivery or total abdominal hysterectomy is also recommended.
- 48. 10. TREATMENT CONT. F. SEXUAL PARTNER OF CONFIRMED BV PATIENT: Sexual activity is a risk factor for transmission. The data do not support treatment of asymptomatic sexual partners of individuals with confirmed BV. Antibiotic treatment of the sexual partners does not increase the rate of clinical or symptomatic improvement for the index patients nor did it reduce the rate of recurrence during a four-week study period. Individuals with documented BV infection should encourage sexual partners who have a vagina to be aware of the signs and symptoms of BV given the high risk of concordant infection (25 to 50 percent).
- 49. 10. TREATMENT CONT. G. RECURRENT BACTERIAL VAGINOSIS: Approximately 30% of patients with initial responses to therapy have a recurrence of symptoms within 3 months, and more than 50% experience a recurrence within 12 months. The explanation for this high rate of recurrence is unclear. Recurrence more likely reflects a 1. Failure to eradicate the offending organisms 2. Failure to re-establish the normal vaginal flora 3. Formation of biofilms which are more difficult to eradicate 4. Treatment failure due antimicrobial resistance 5. Nonadherence to medications
- 50. 10. TREATMENT CONT. G. RECURRENT BACTERIAL VAGINOSIS: The only interventions proven to reduce development or recurrence of BV are chronic suppressive therapy and circumcision of male partner. Symptomatic recurrent BV should be treated initially with a seven-day course of oral or vaginal metronidazole or clindamycin (alternate between the two antibiotics). Alternative treatment: vaginal boric acid suppositories for 30 days can be used as an induction regimen simultaneously or to follow seven-day oral antibiotic treatment. The treatment regimen may be the same or different from the initial or previous treatment regimen.
- 51. 10. TREATMENT CONT. G. RECURRENT BACTERIAL VAGINOSIS: FIRST CHOICE Oral or Vaginal Metronidazole or Clindamycin for 7 days as in treatment of symptomatic nonpregnant patients. ALTERNATIVE THERAPY Oral Metronidazole or Clindamycin for 7 days PLUS Vaginal boric acid 600 mg PV OD (at bedtime) for 30 days. Oral Metronidazole or Clindamycin for 7 days FOLLOWED BY Vaginal boric acid 600 mg PV OD (at bedtime) for 30 days N.B: Vaginal boric acid alone is ineffective. Boric acid can cause death if taken orally. Boric acid should not be used by individuals who are pregnant or attempting conception. Sexual partners of patients treated with vaginal boric acid have reported skin irritation after exposure.
- 52. 10. TREATMENT CONT. G. RECURRENT BV – LONG-TERM SUPPRESIVE REGIMEN: After initial induction therapy, most individuals with a history of recurrent infection benefit from suppressive therapy to maintain an asymptomatic state. Patient with more than 3 documented episodes of BV in the previous 12 months should be offered a long-term suppressive regimen consisting of maintenance metronidazole vaginal gel. Long-term clindamycin regimens, oral or topical, are not advised because of toxicity (oral) and lack of documented efficacy (topical).
- 53. 10. TREATMENT CONT. G. RECURRENT BV – LONG-TERM SUPPRESIVE REGIMEN: Metronidazole Monotherapy: – Metronidazole gel 0.75% or an oral nitroimidazole for 7 to 10 days followed by twice-weekly dosing of metronidazole gel for more than three months (treat for four to six months). – In Metronidazole Monotherapy, secondary vaginal candidiasis was a common side effect. Combination Therapy followed by suppression therapy: – Oral nitroimidazole for 7 days and vaginal boric acid 600 mg once daily at bedtime is begun at the same time and continued for 21 days. – Follow-up a day or two after their last vaginal boric acid dose; if they are in remission, immediately begin metronidazole gel twice weekly for four to six months as suppressive therapy.
- 54. 10. TREATMENT CONT. G. RECURRENT BV – LONG-TERM SUPPRESIVE REGIMEN: METRONIDAZOLE MONOTHERAPY Oral or Vaginal Metronidazole for 7 to 10 days FOLLOWED BY Twice-weekly dosing of Metronidazole gel for more than three months (four to six months). COMBINATION FOLLOWED BY SUPPRESSION THERAPY Oral Metronidazole or Tinidazole for 7 days AND Vaginal boric acid 600 mg once daily at bedtime for 21 days. If patient is in remission, begin: Twice-weekly dosing of Metronidazole gel for more than three months (four to six months).
- 55. 10. TREATMENT CONT. G. RECURRENT BV – LONG-TERM SUPPRESIVE REGIMEN: Intravaginal L. Crispatus (LACTIN-V) – Intravaginal treatment with Lactobacillus crispatus is a promising therapy to follow the initial course of metronidazole. – This approach is promising both: 1. For eliminating Bacterial Vaginosis and 2. For restoring Lactobacillus colonization – In addition, the product is not commercially available, and study results should not be extrapolated to other probiotic remedies. Treatment: Vaginal metronidazole for 7 days followed by Intravaginal LACTIN-V once daily for 11 weeks.
- 56. 10. TREATMENT CONT. OTHER LESS STUDIES TREATMENT: 1. Combination of metronidazole and fluconazole 2. Treatment with lactobacillus - Exogenous lactobacillus recolonization with 30 days of oral probiotic Lactobacillus rhamnosus and Lactobacillus reuteri in addition to seven days of metronidazole therapy. 3. Vaginal microbiome transplant 4. Vaginal boric acid with EDTA (ethylenediaminetetraacetic acid) for bacteria that forms biofilms.
- 57. 11. COMPLICSCATIONS • GYNAECOLOGICAL COMPLICATIONS 1. Psychological Disturbances 2. Increase risk of STIs including HIV and HSV 3. Bacteraemia 4. PID and UTI • OBSTETRIC COMPLICATIONS 1. Preterm delivery and LBW 2. Premature labour due to choriamnionitis 3. Late term miscarriage 4. Postpartum fever, endometritis and salpingitis • POSTOPERATIVE COMPLICATIONS 1. Wound infection 2. Vaginal cuff infection
- 58. 12. PREVENTION 1. Use of condoms 2. Hormonal contraceptives 3. Avoid douching, tub baths, and bubble baths 4. Avoid the use of feminine hygiene products ( vulvovaginal products) 5. Avoid the use of liquid soaps and body washes 6. Cleaning sex toys between use 7. Use of gloves during digital-vaginal sex 8. Use of probiotics 9. Limiting number of sex partners 10. Avoid thongs and tight nylon tights
- 59. 13. CONCLUSION • The BV prevalence is high globally, with concomitant high economic burden and marked racial disparities in prevalence. • Research to determine aetiology, prevention, and treatment strategies are urgently needed to reduce the burden of BV among women. • Women with recurrent BV reported psychological and social impacts on their self-esteem, sexual relationship, and quality of life. • Support and acknowledgement of impacts of BV on women life are required when managing women with recurrent BV.
- 60. 14. REFERENCES 1. Williams Gynaecology Third Edition 2. Dutta’s Textbook of Gynaecology Eighth Edition 3. Bacterial Vaginosis. eMedicine: https://emedicine.medscape.com/article/254342-overview 4. Bacterial Vaginosis. Uptodate (2021): https://www.uptodate.com/contents/bacterial-vaginosis- treatment/print 5. Bacterial vaginosis. CDC (2021): https://www.cdc.gov/std/treatment-guidelines/bv.htm 6. Bacterial vaginosis, Wikipedia (2021): https://en.wikipedia.org/wiki/Bacterial_vaginosis 7. Bactrial Vaginosis – Global burden. Stdjournal (2019): https://journals.lww.com/stdjournal/Fulltext/2019/05000/High_G lobal_Burden_and_Costs_of_Bacterial.5.aspx
- 61. “Do not cry over spilled milk. By this time tomorrow, it will be free yoghurt. Compliments to Lactobacillus bulgaricus” TAHNK FOR LISTENING. ANY QUESTION?