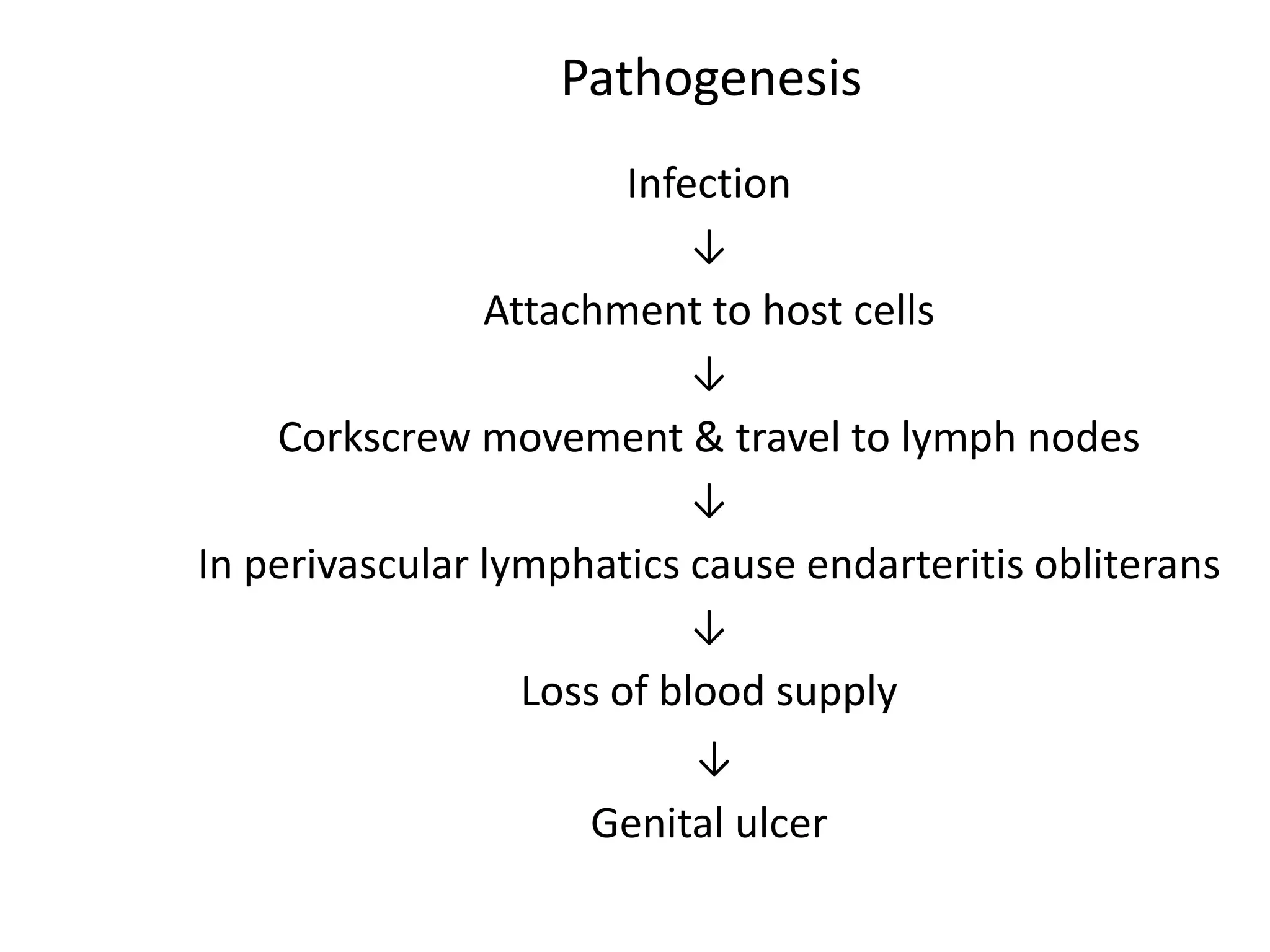
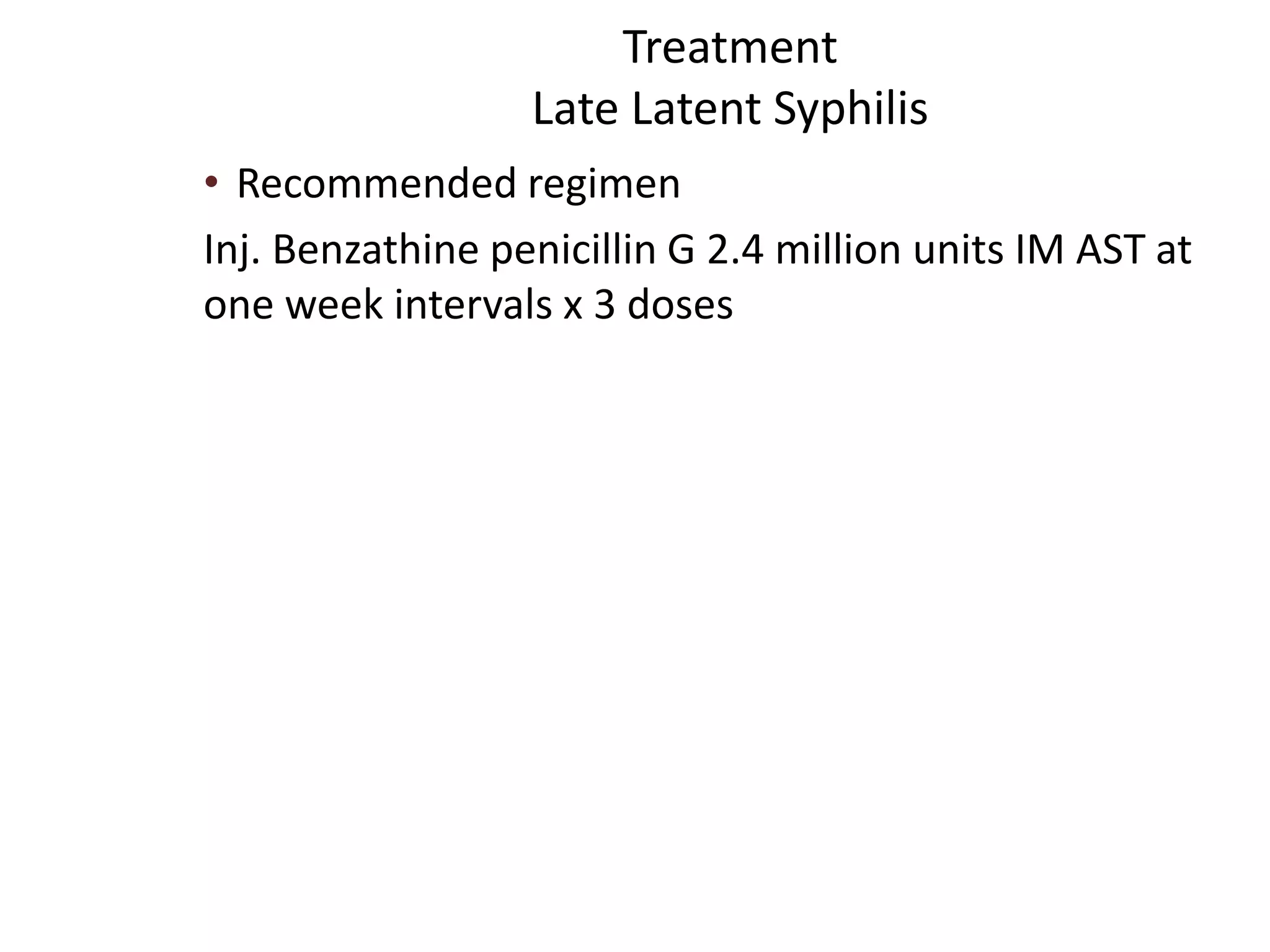
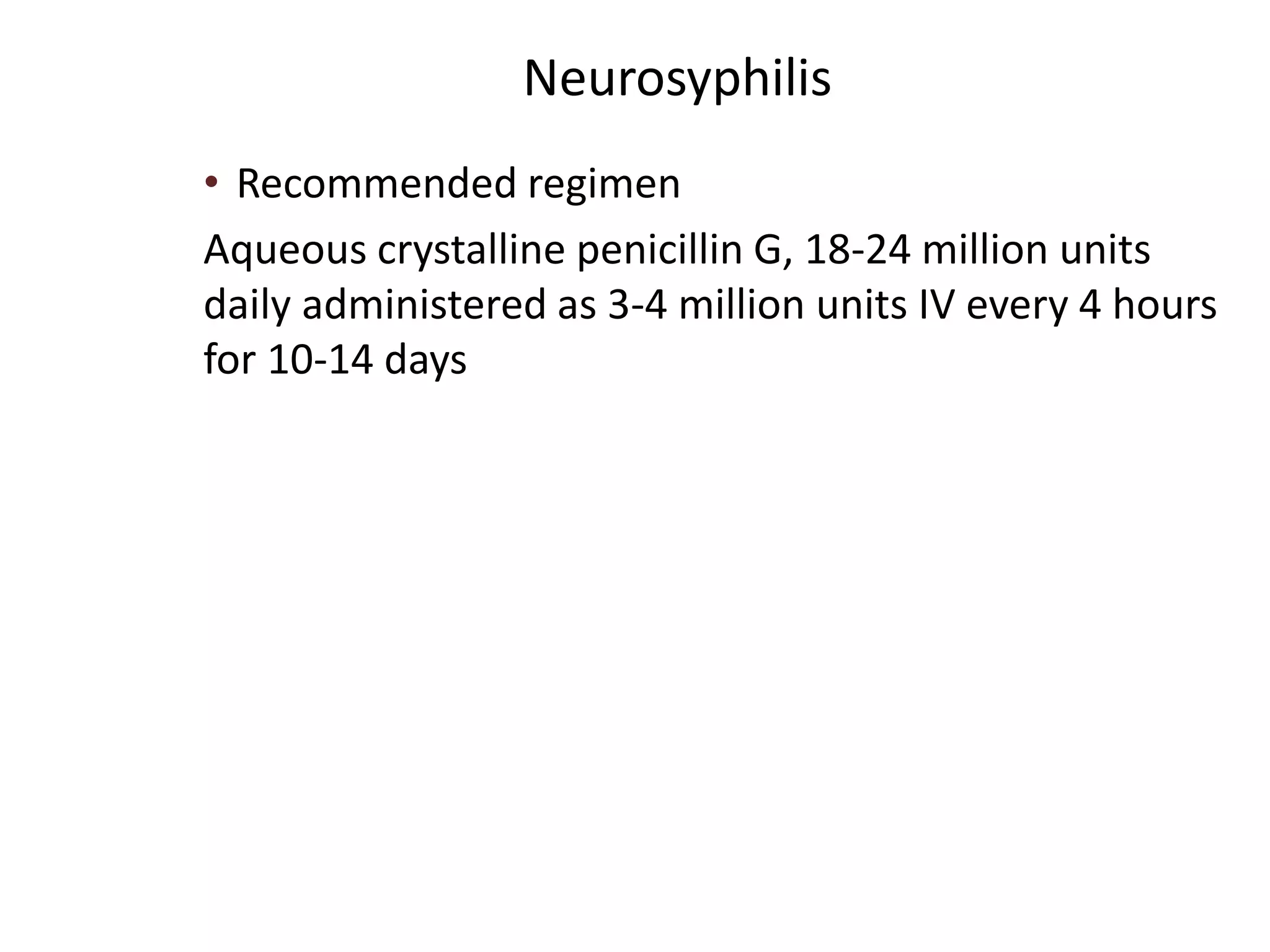
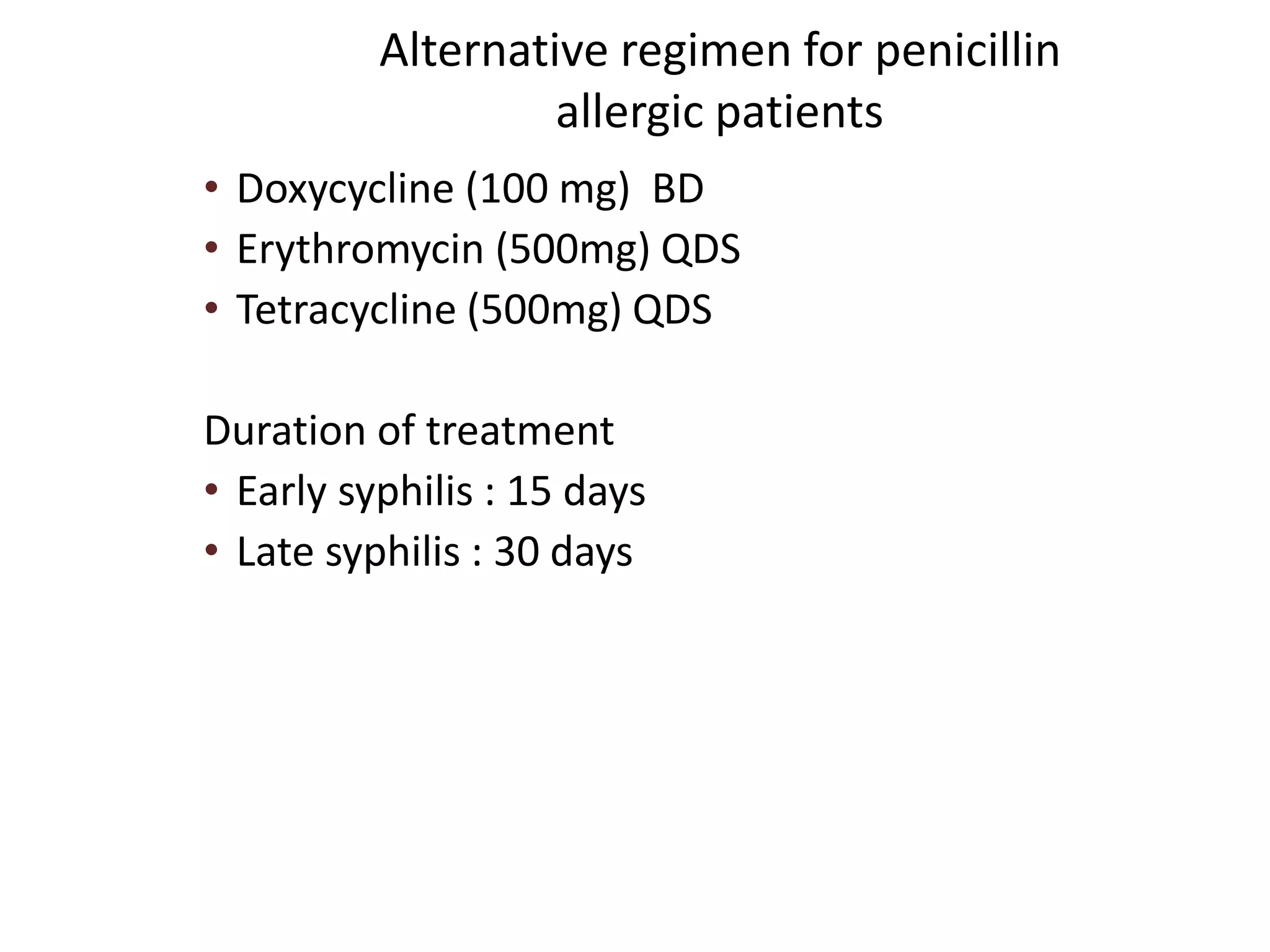
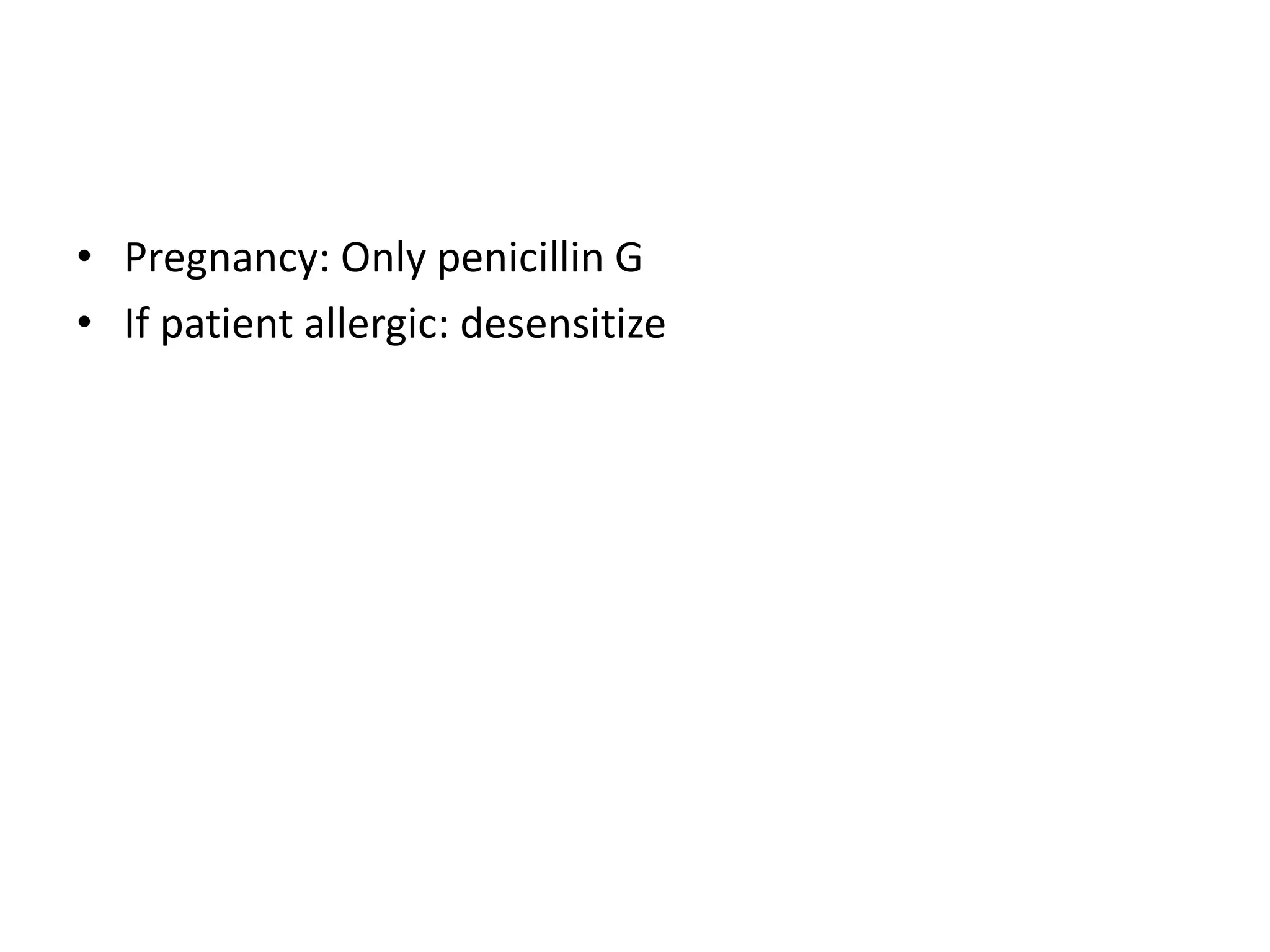
This document provides an overview of sexually transmitted infections (STIs), with a focus on syphilis. It defines STIs and notes that the number of causative agents has expanded beyond the original "five classical venereal diseases." STIs are classified into bacterial, viral, protozoal, fungal and ectoparasitic agents. The document then describes the epidemiology, transmission, pathogenesis, signs/symptoms, diagnosis and treatment recommendations for syphilis in primary, secondary, latent and tertiary stages according to CDC guidelines. Penicillin is the recommended treatment, with alternatives for penicillin-allergic patients. The potential Jarisch-Herxheimer reaction is also mentioned.