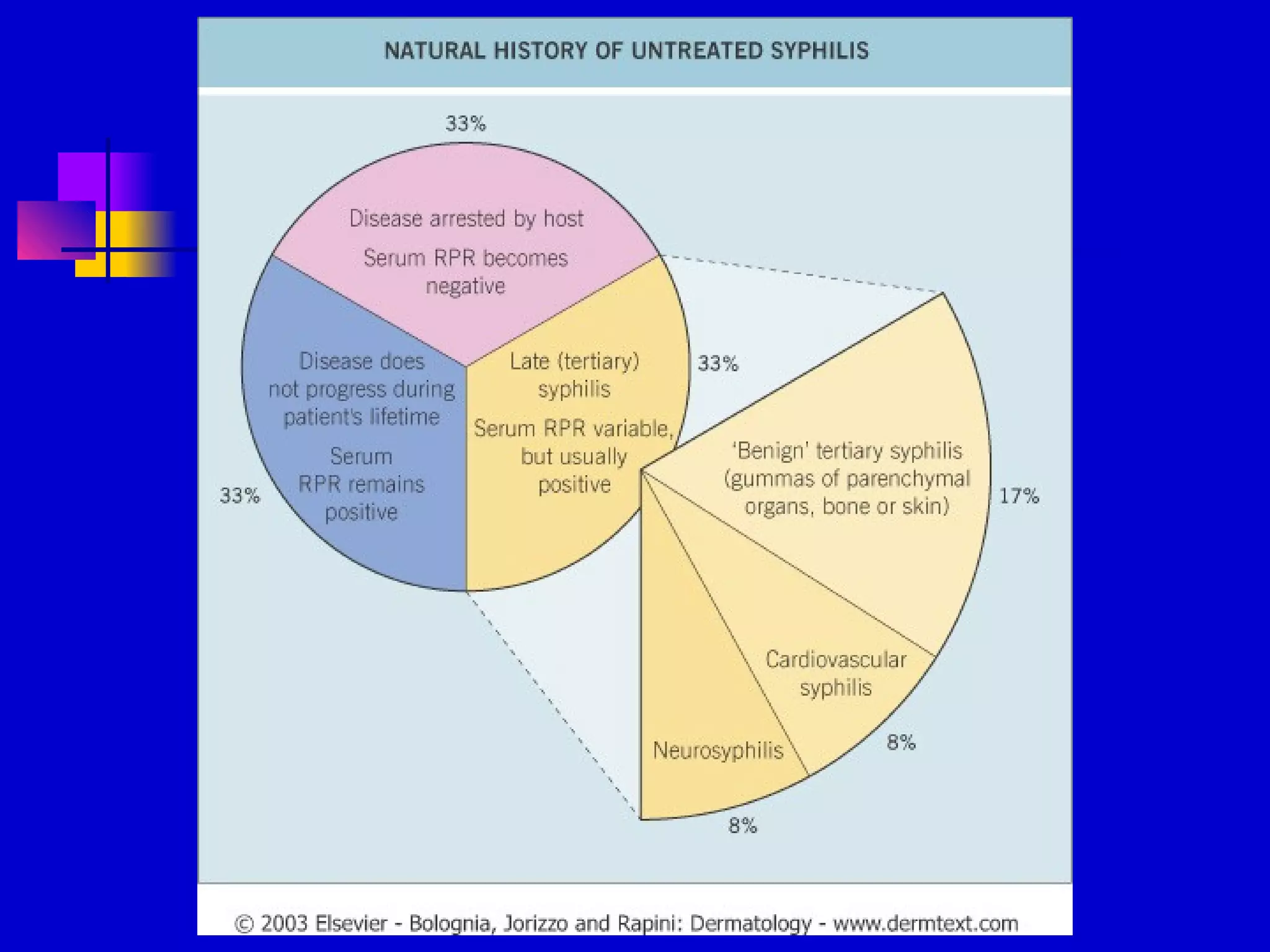
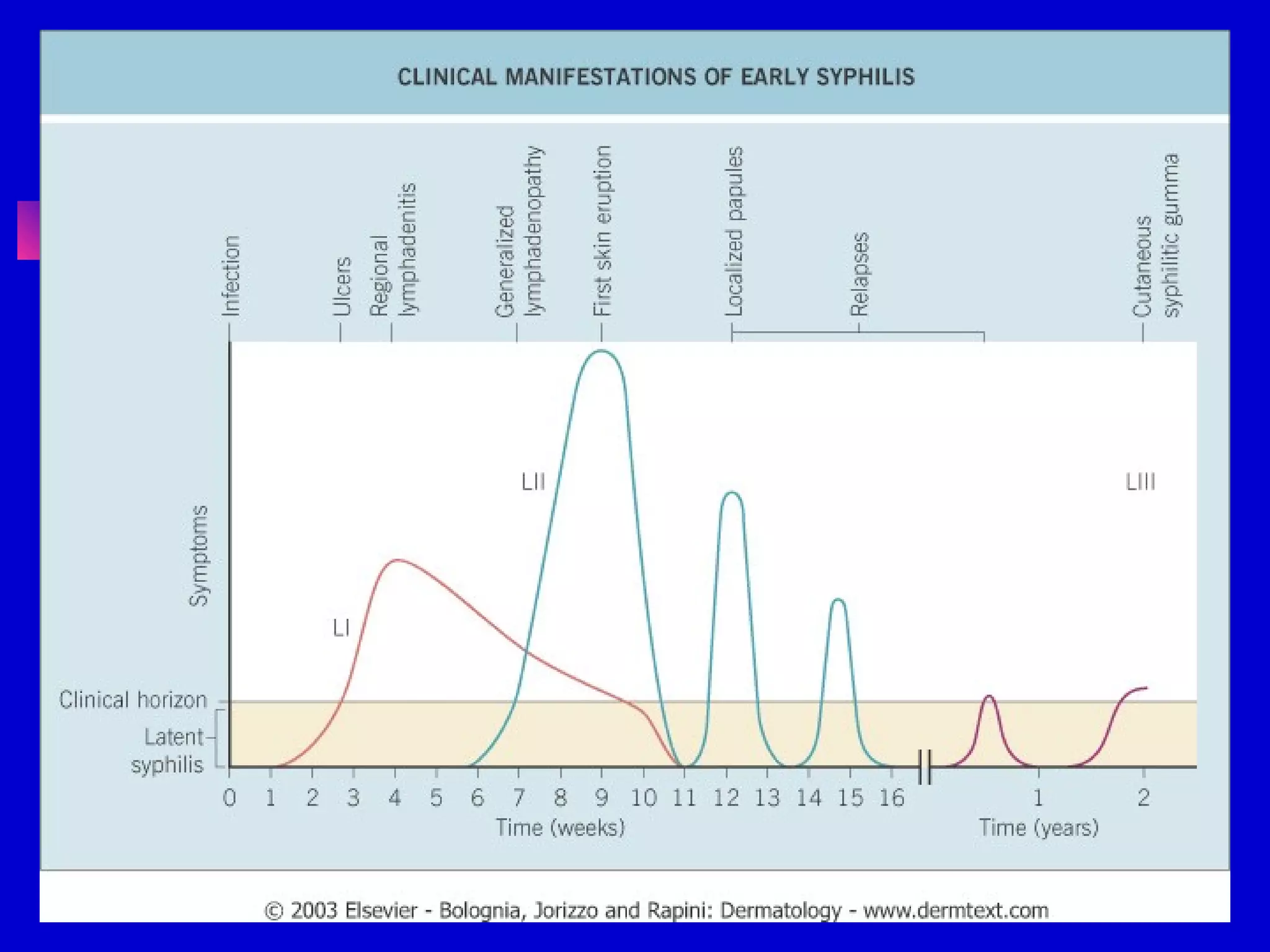
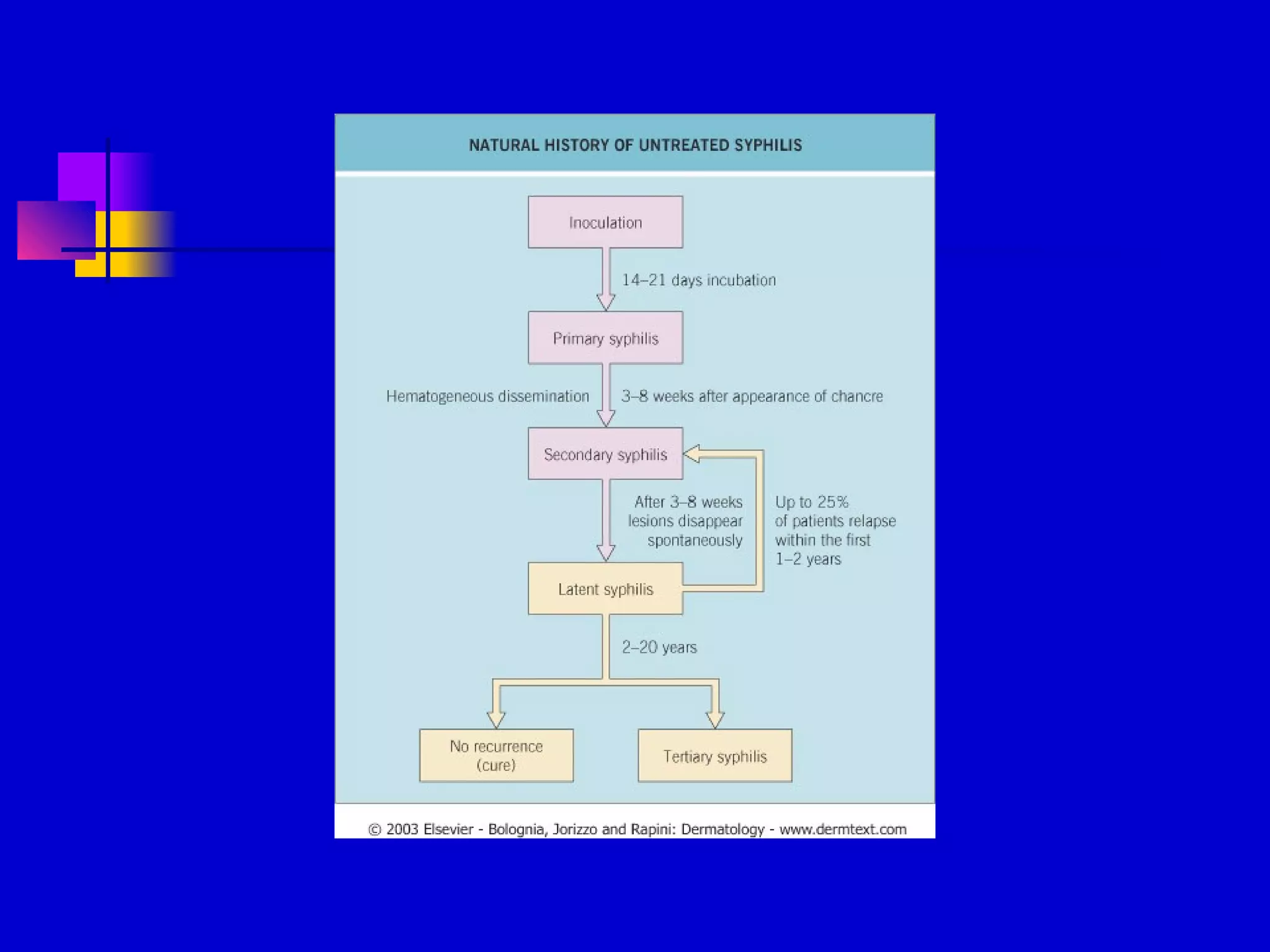
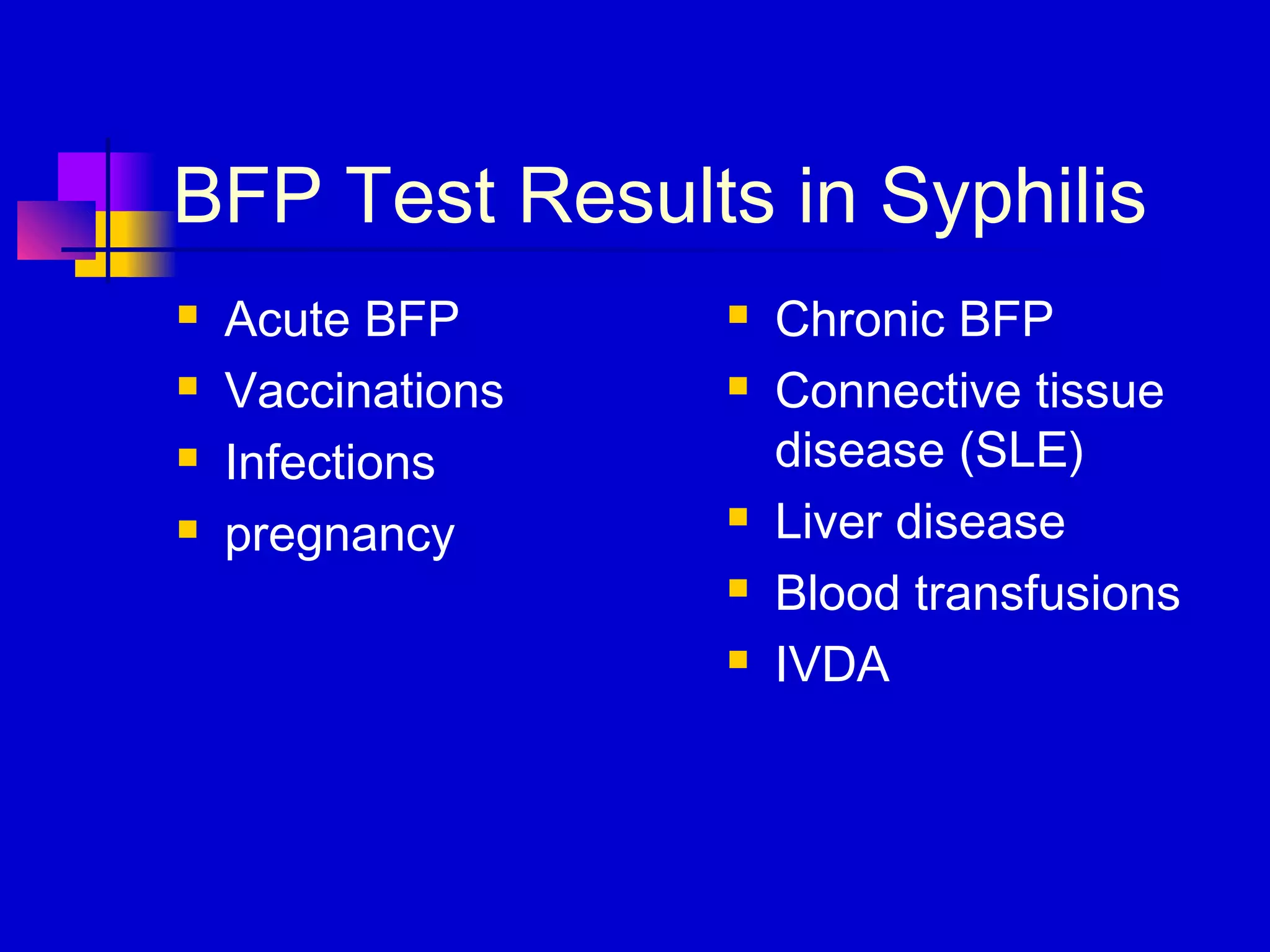
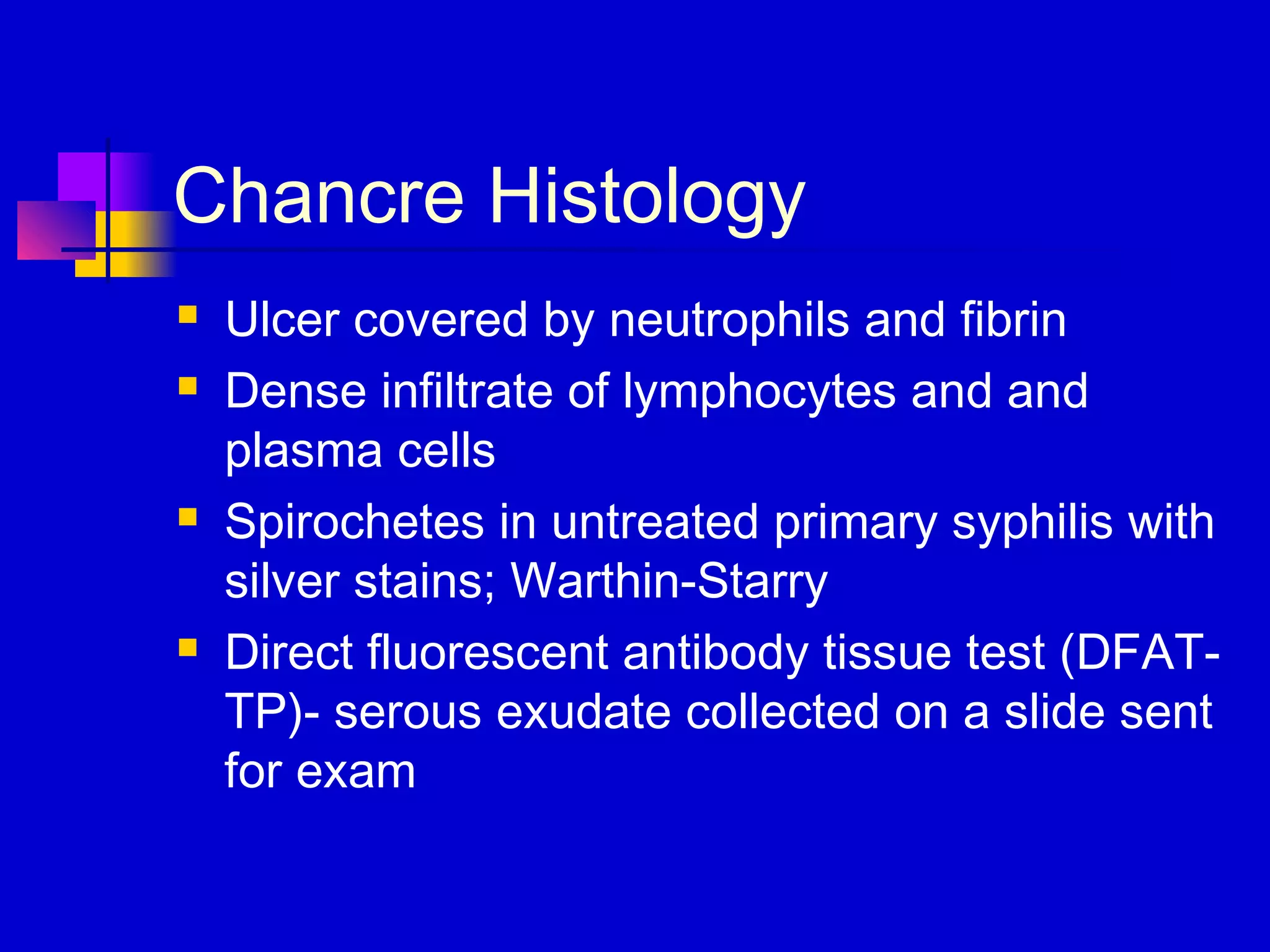
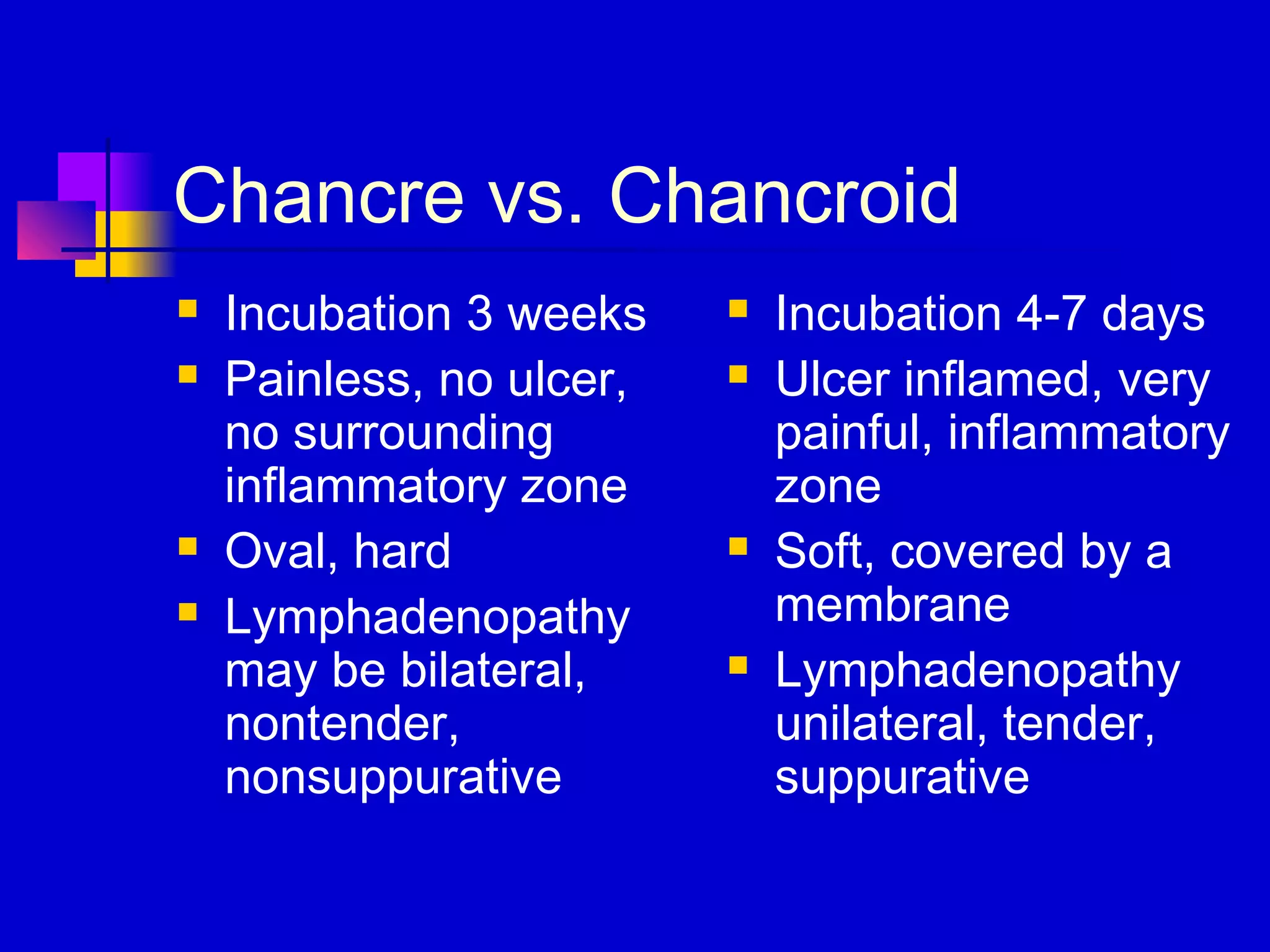
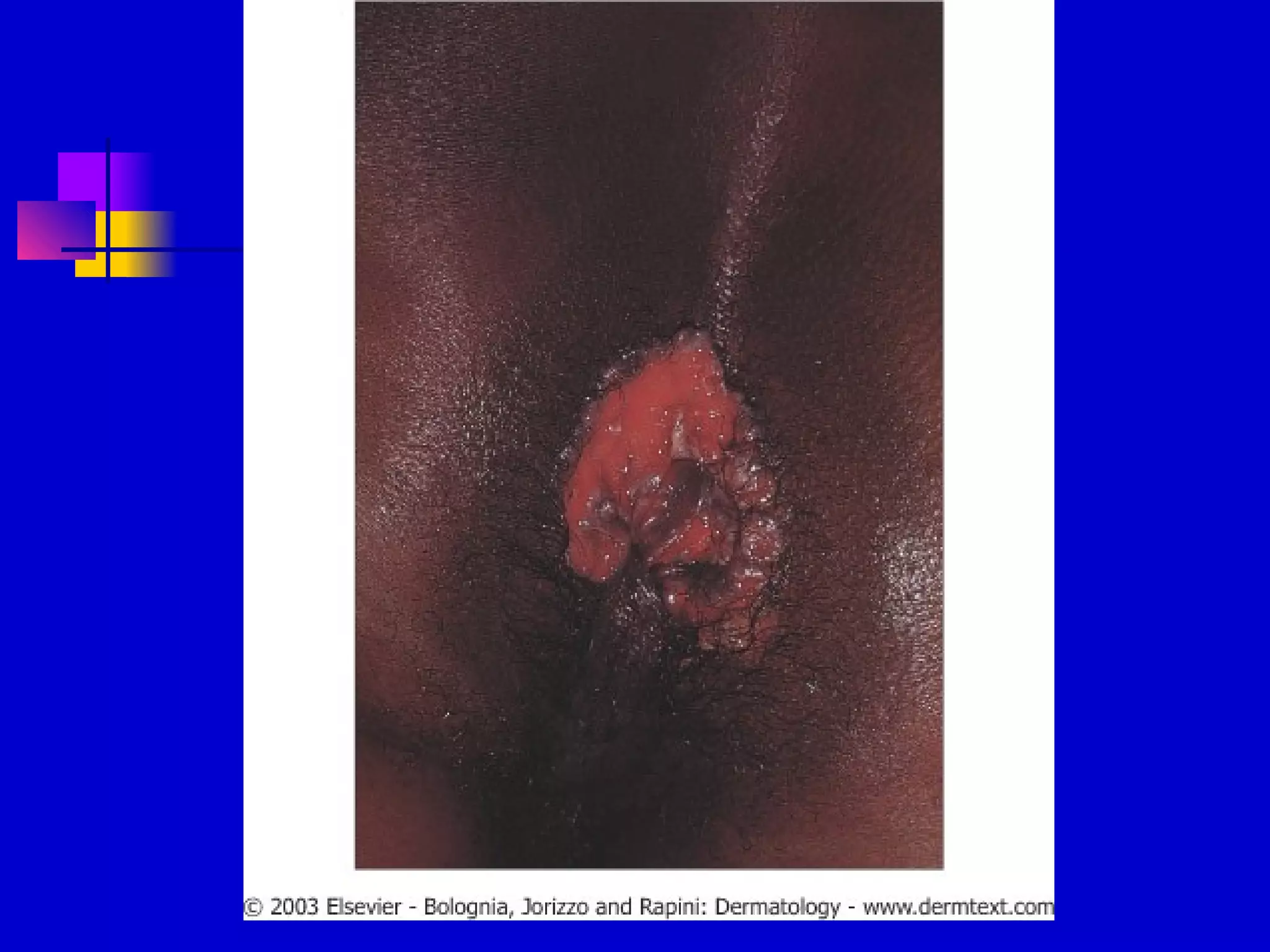
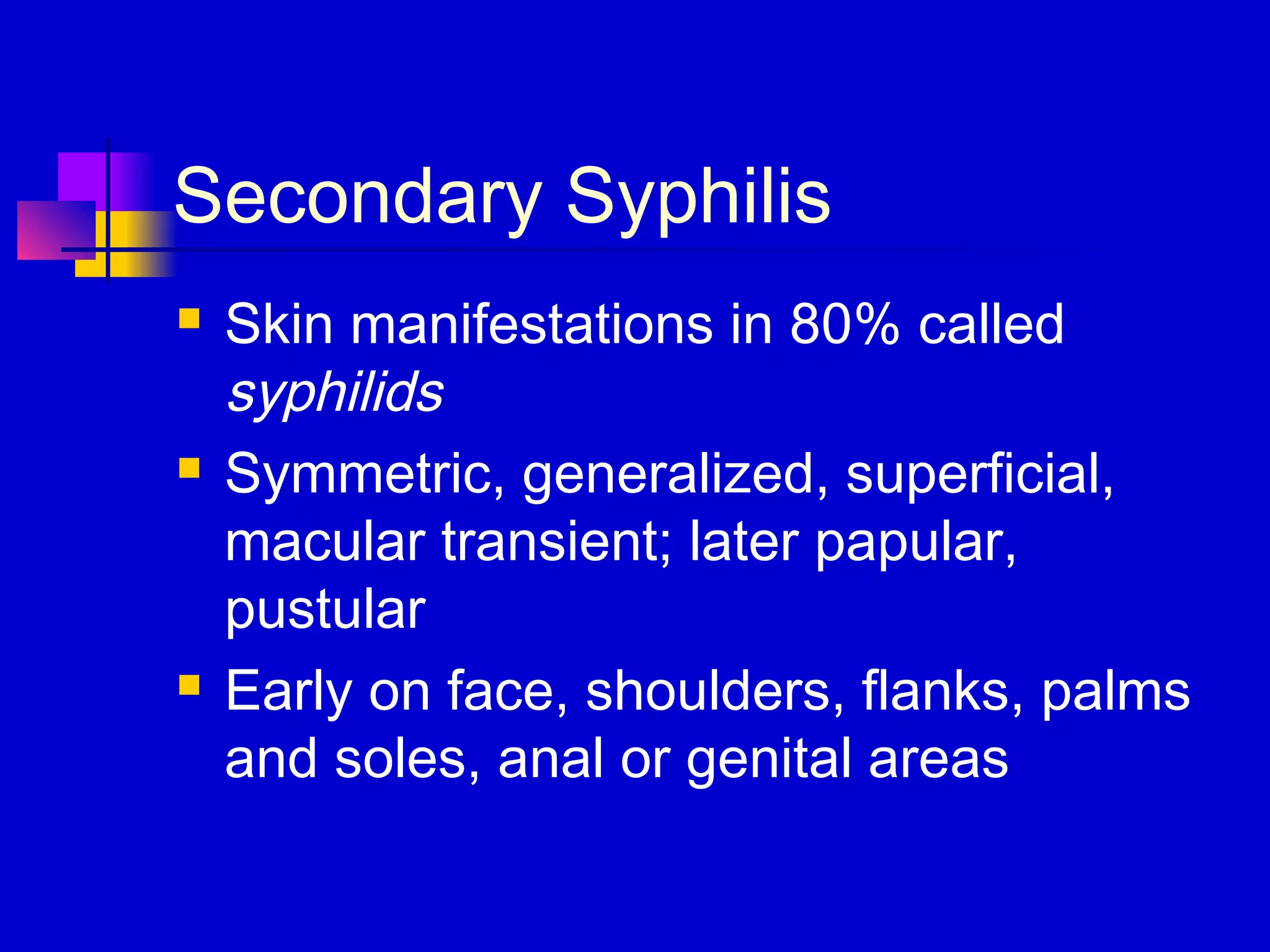
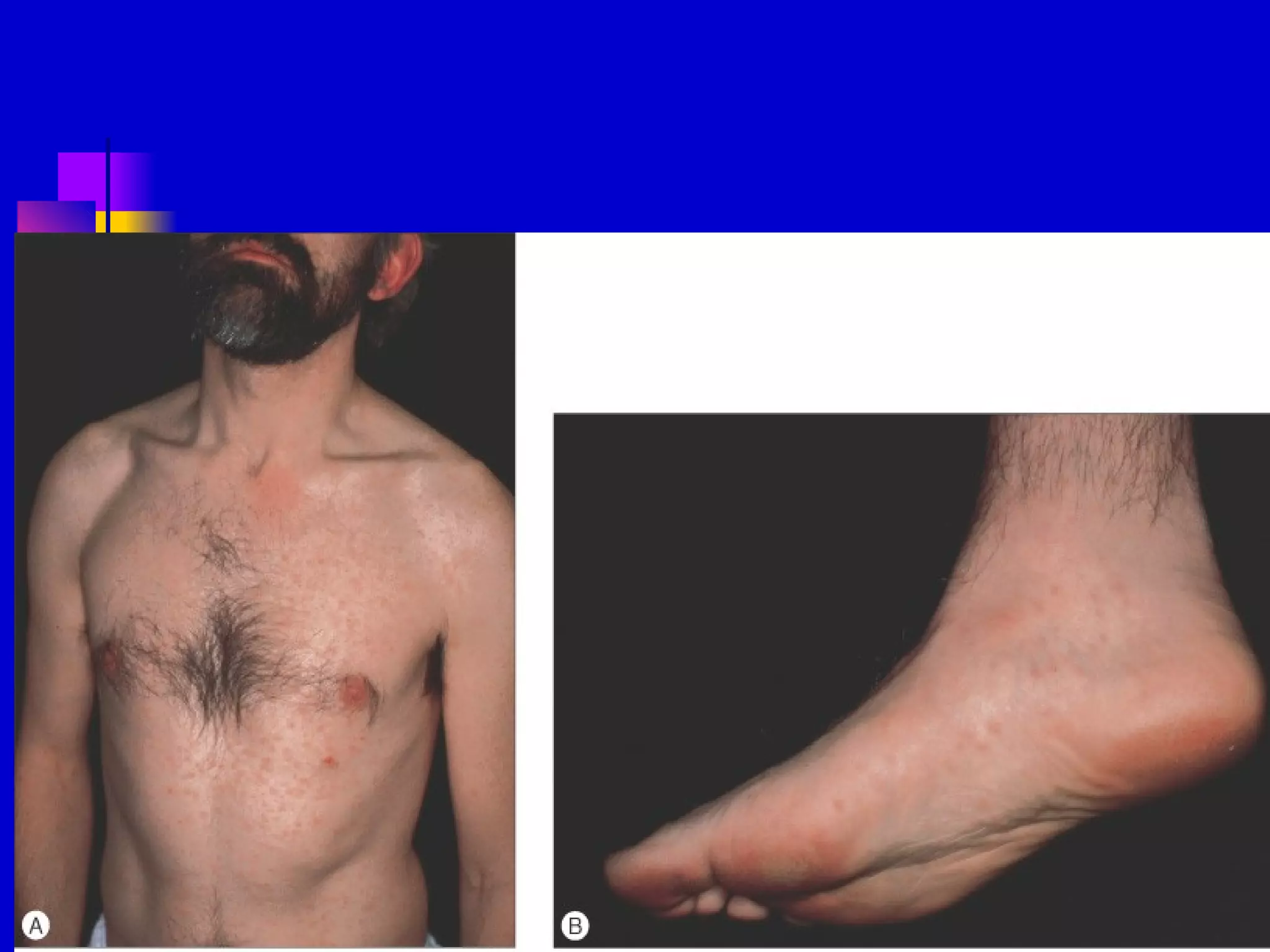
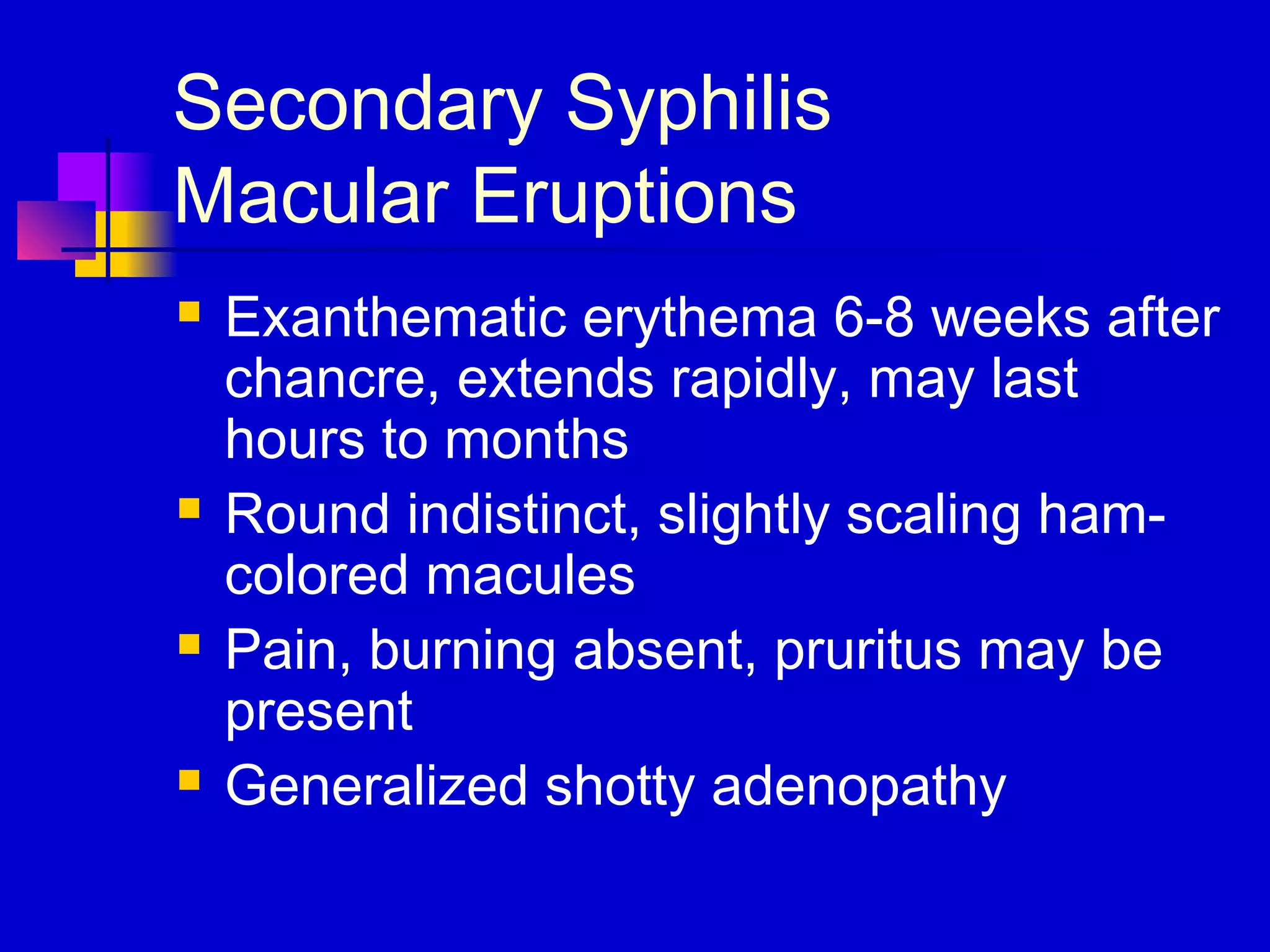
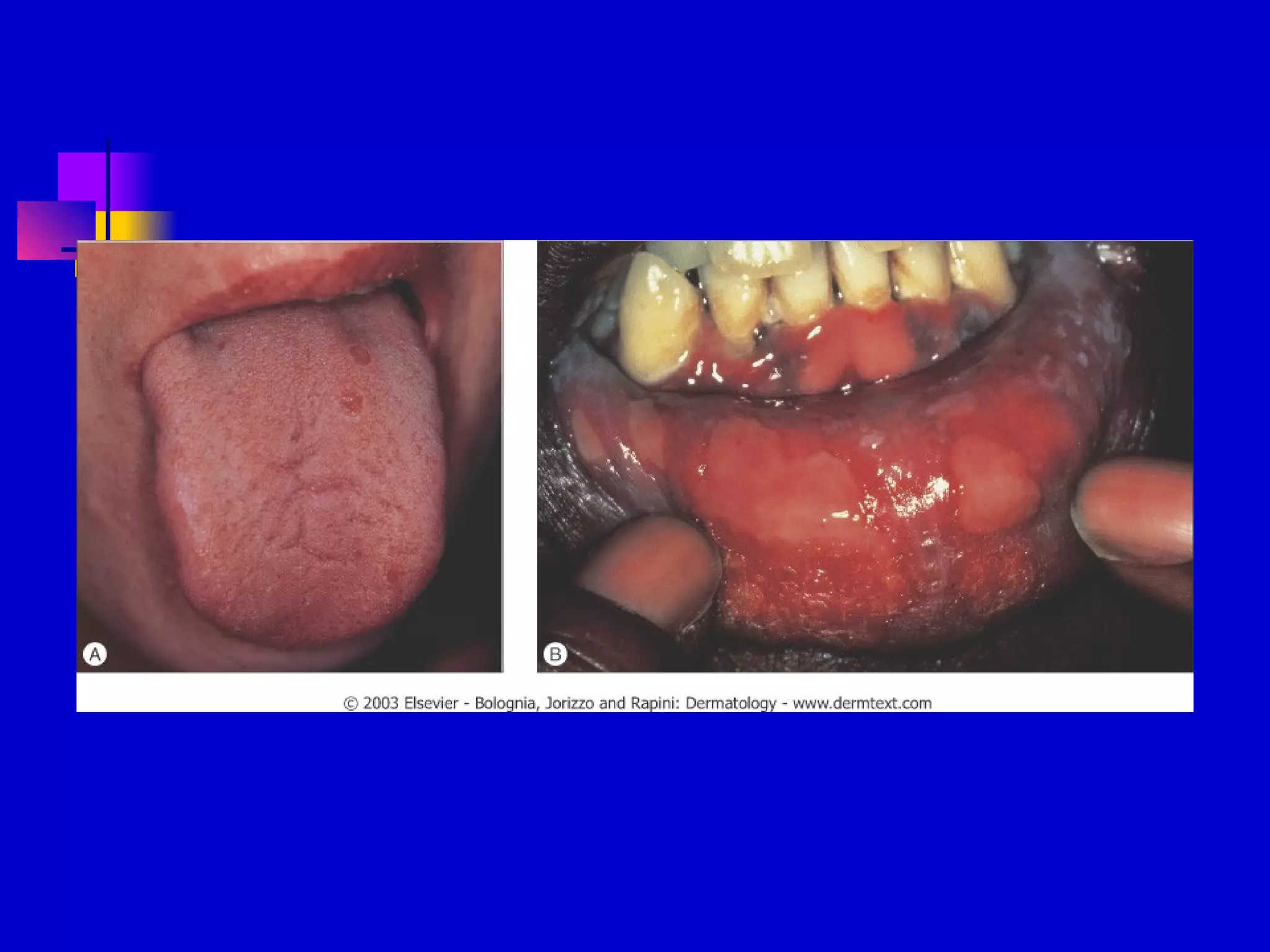
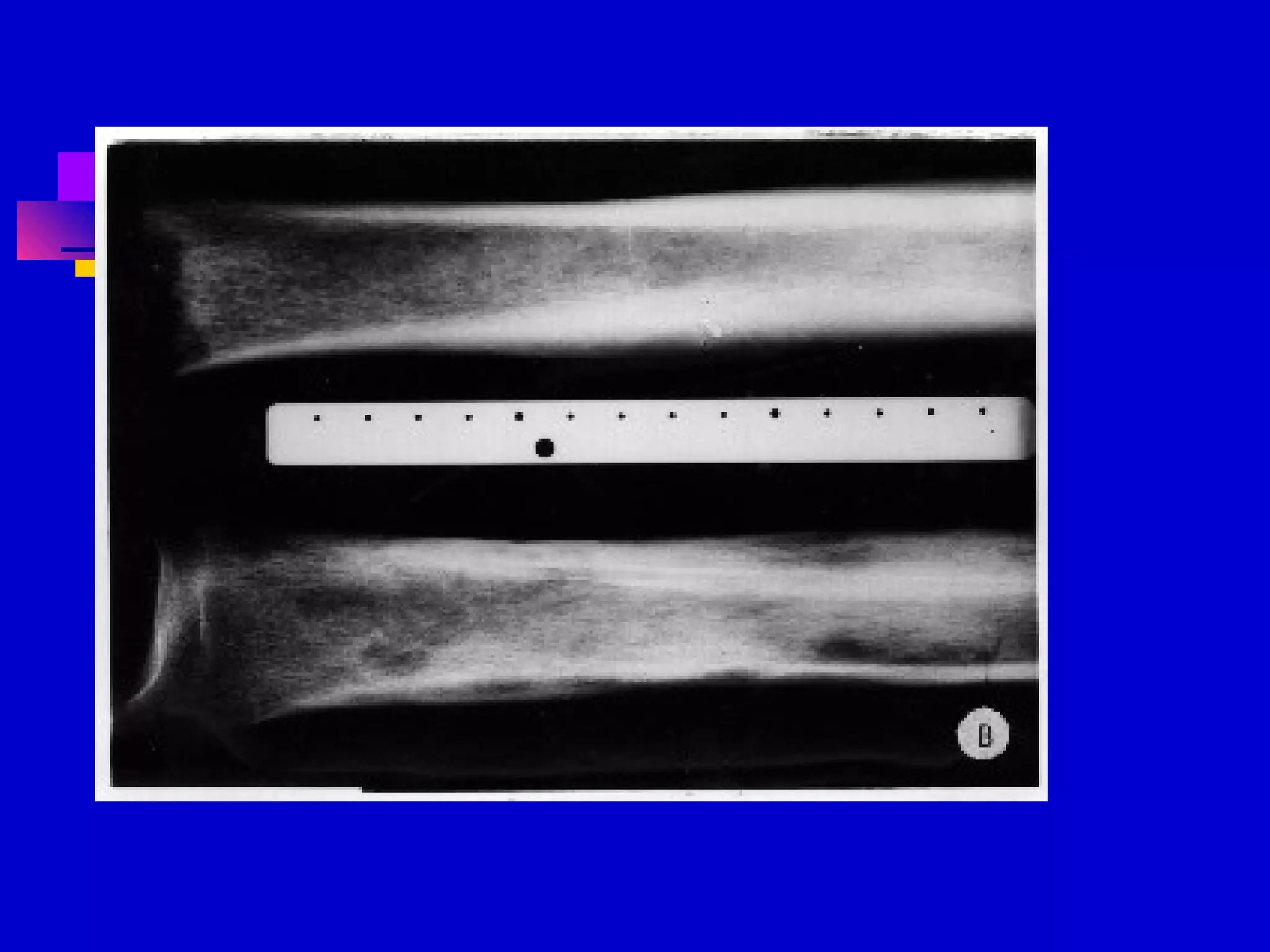
This document provides information on syphilis, caused by the spirochete Treponema pallidum. It is a contagious sexually transmitted disease with four stages: primary, secondary, latent, and tertiary. The primary stage involves a chancre at the infection site. Secondary syphilis presents with rashes and mucous membrane lesions. Latent syphilis involves no symptoms. Late stage syphilis can involve skin gummas, bone and neurological involvement like tabes dorsalis or general paresis. Syphilis screening involves nontreponemal and treponemal tests and darkfield microscopy of lesions.