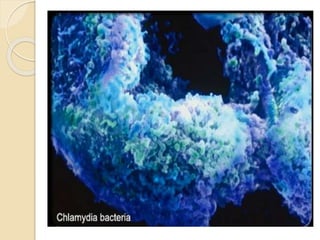
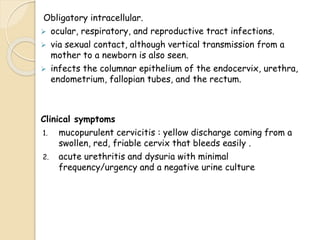
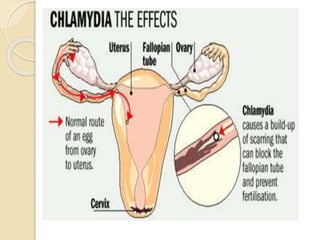
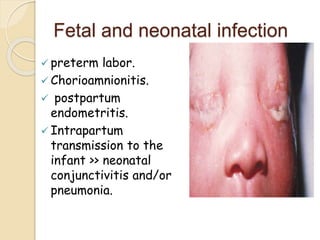
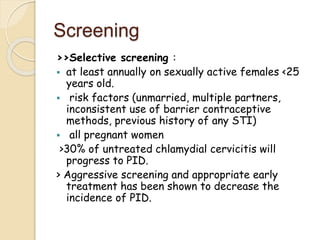
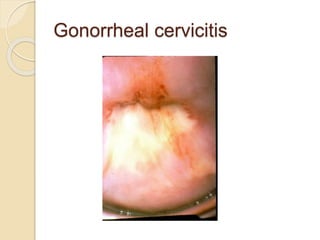
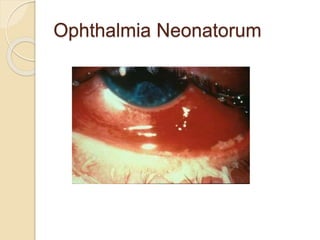
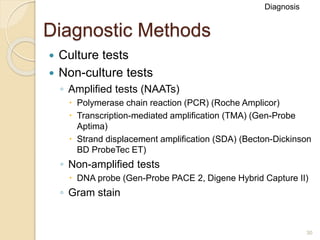
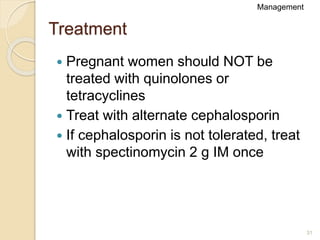
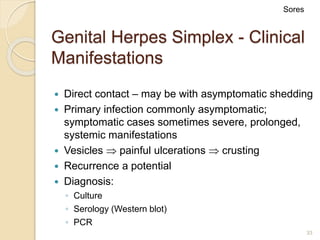
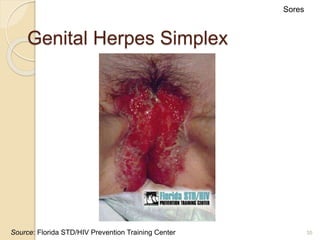
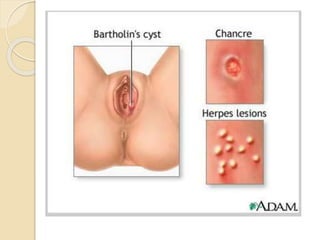
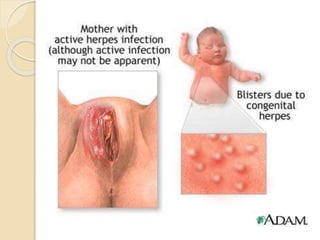
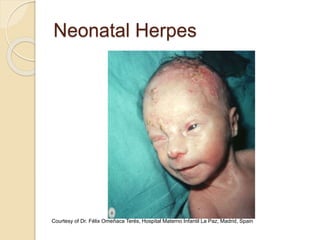
Sexually transmitted diseases (STDs) can be passed from person to person during sexual contact and from mother to baby during pregnancy or childbirth. Common STDs discussed include chlamydia, gonorrhea, herpes, syphilis, HIV, and how each can affect both sexual partners and newborns. STDs are diagnosed through tests and examinations and treated with antibiotics or antiviral medications to cure the infection and prevent transmission. Untreated STDs can lead to long-term health issues like infertility, stillbirth, or developmental delays in infants.