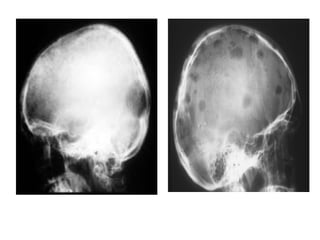
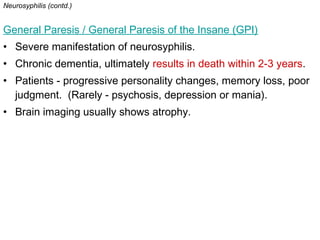
Syphilis is a sexually transmitted disease caused by the bacterium Treponema pallidum. It has four stages: primary, secondary, latent, and tertiary. The primary stage involves a chancre at the infection site. Secondary syphilis causes a rash and mucous patches. Latent syphilis has no symptoms. Tertiary syphilis can cause gummas, neurological issues, and cardiovascular complications if left untreated. Syphilis is diagnosed through fluid microscopy, serological tests like RPR and FTA-ABS, and clinical history. It is treated with penicillin, doxycycline, or ceftriaxone depending on the stage. Prevention involves abstinence, condoms,

![SYPHILIS INFECTION
4 stages
1] Primary syphilis
via direct sexual contact (exposure to the infectious lesions of a person
with syphilis).
Primary chancre of syphilis is seen at the site of infection 10-90 days
post-initial exposure (average 21 days)
Chancre:
1° skin lesion at site of contact (usually genitalia, but can be anywhere on
the body).
firm, painless skin ulceration localized at the point of initial exposure to the
spirochete (often on penis / vagina / rectum).
Multiple lesions (rarely); typically only one lesion is seen.
Persists for 4 - 6 weeks, then heals; local lymph node swelling can
occur.
Asymptomatic during initial incubation period (many patients do not seek
medical care immediately).
Cannot be contracted through toilet seats, daily activities, hot tubs, or
sharing eating utensils or clothing](https://image.slidesharecdn.com/syphilisinanutshell-151002070250-lva1-app6892/85/Syphilis-in-a-nutshell-3-320.jpg)

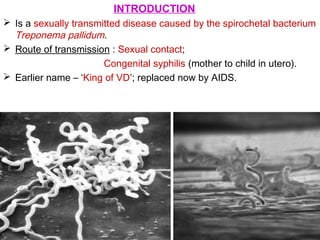
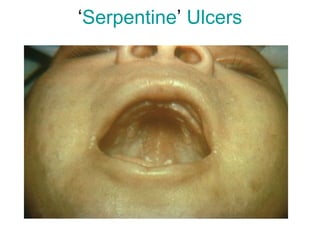
![2] Secondary syphilis
Approximately 1-6 months post-primary infection (commonly 6 - 8
weeks).
Many different manifestations.
Patient is most contagious in this stage.
Symmetrical reddish-pink non-itchy rash on trunk and extremities.
Rash – usually on palms of the hands and the soles of the feet.
Moist areas of body - the rash becomes flat, broad, whitish lesions
known as ‘Condylomata lata’.
‘Serpentine Ulcers’ – in mouth.
Mucous patches on the genitals or in the mouth.
Genital warts, ulcers and chancres.
All of these lesions are infectious and contain active treponema
organisms.
Fever, sore throat, malaise, wt. loss, headache, meningismus.
Enlarged lymph nodes
Rare manifestations :
• acute meningitis, hepatitis, renal disease, hypertrophic gastritis, patchy
proctitis, ulcerative colitis, rectosigmoid mass, arthritis, periostitis, optic
neuritis, intersitial keratitis, iritis, and uveitis.](https://image.slidesharecdn.com/syphilisinanutshell-151002070250-lva1-app6892/85/Syphilis-in-a-nutshell-5-320.jpg)

![3] Latent syphilis
Defined as having ‘serologic proof of infection without signs or
symptoms of disease.’
Can be either early or late.
Early latent syphilis: having syphilis for two years or less from the
time of initial infection without signs or symptoms of disease.
Late latent syphilis: infection for more than two years but without
clinical evidence of disease.
Distinction is important for both therapy and risk for transmission.
* Early latent syphilis : single I.M. injection of long-acting penicillin;
* Late latent syphilis : three injections each week.
50% of latent syphilis cases progress into late stage syphilis;
25% stay in the latent stage, and rest 25% make a full recovery.](https://image.slidesharecdn.com/syphilisinanutshell-151002070250-lva1-app6892/85/Syphilis-in-a-nutshell-9-320.jpg)
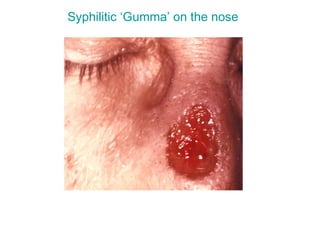
![4] Tertiary syphilis
Occurs 1-10 years after initial infection, (can take up
to 50 years also).
‘Gummas’ or granulomas…
soft, tumor-like balls of inflammation;
are chronic; immune system is unable to completely clear
the organism.
appear almost anywhere in the body (including the
skeleton).
Gummas: indicate chronic inflammatory state in body;
mass-effects upon the local anatomy.](https://image.slidesharecdn.com/syphilisinanutshell-151002070250-lva1-app6892/85/Syphilis-in-a-nutshell-10-320.jpg)

![TREATMENT
1] Penicillin G
• First choice of treatment.
• For Early syphilis – one dose is sufficient.
• For Latent Syphilis – weekly dose for 3 weeks.
• Parenteral penicillin G can be used during pregnancy.
2] Oral Tetracycline and Doxycycline
• For penicillin-sensitive patients.
3] Ceftriaxone, Azithromycin](https://image.slidesharecdn.com/syphilisinanutshell-151002070250-lva1-app6892/85/Syphilis-in-a-nutshell-23-320.jpg)