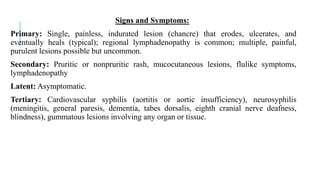
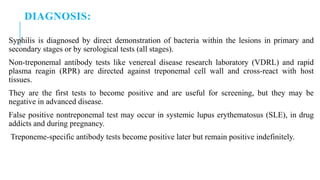
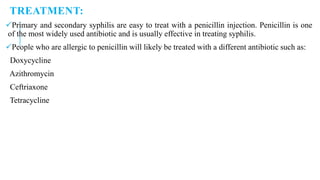
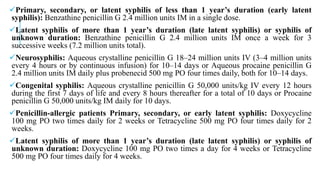
Syphilis is a sexually transmitted disease caused by the spirochete Treponema pallidum. It has four stages - primary, secondary, latent, and tertiary - and can cause lesions, rashes, and long-term damage if untreated. It is diagnosed through direct visualization of spirochetes or serological tests. Treatment involves penicillin, doxycycline, or tetracycline depending on the stage of disease. Syphilis can also be transmitted from mother to child during pregnancy or childbirth, potentially causing fetal death or lifelong infections.