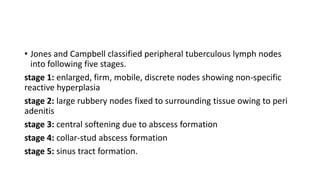
Tuberculosis of peripheral lymph nodes, also known as tuberculous lymphadenitis, is the most common extrapulmonary manifestation of tuberculosis. It typically involves the cervical lymph nodes. The infection can spread hematogenously from a primary lung infection or directly from a contiguous focus. Diagnosis involves physical examination, tuberculin testing, staining of aspirated lymph node samples for acid-fast bacilli, and radiological or PCR analysis. Treatment primarily consists of a standard course of antituberculosis drugs according to WHO guidelines.