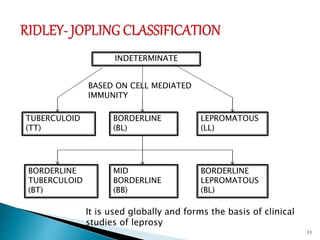
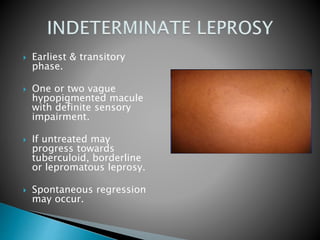
Leprosy is a chronic infectious disease caused by Mycobacterium leprae. It is characterized by lesions of the peripheral nerves, skin, and nasal mucosa. There are different clinical classifications of leprosy based on immune response and bacterial load, ranging from tuberculoid leprosy with few bacteria and strong immune response to lepromatous leprosy with many bacteria and weak immune response. Without treatment, leprosy can cause permanent damage, especially to the hands, feet, and face.