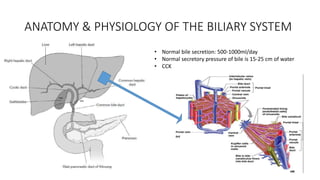
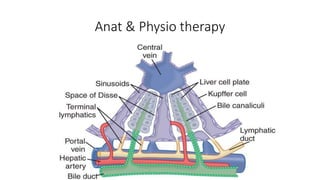
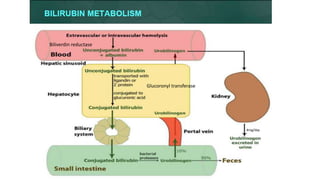
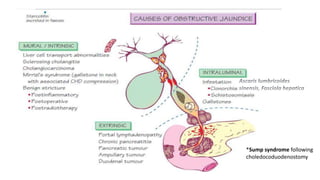
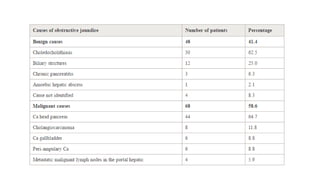
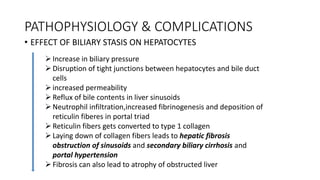
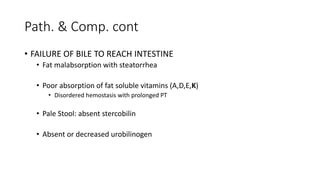
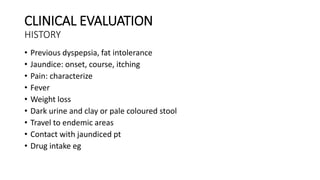
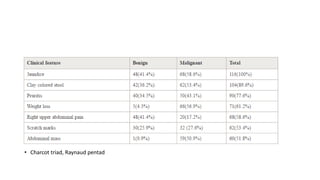
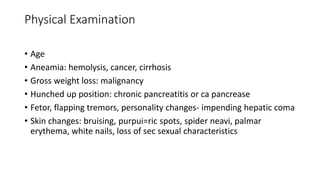
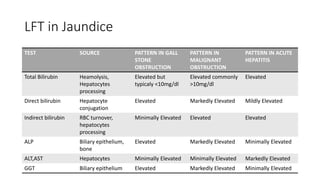
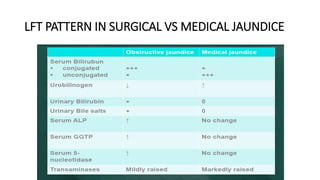
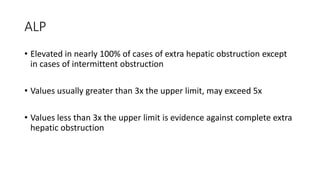
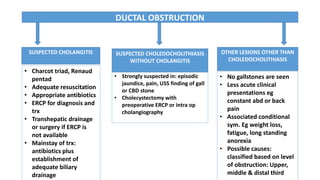
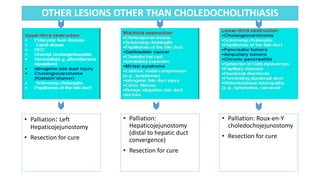
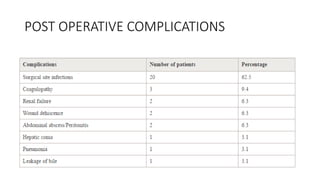
Surgical jaundice refers to jaundice that is caused by a mechanical obstruction in the extrahepatic biliary tree or within the porta hepatis, and is amenable to surgical treatment. It results from the failure of the normal amount of bile to reach the intestine. Causes include gallstones, tumors, strictures. Complications arise from bile stasis in the liver and lack of bile in the intestine, and can include hepatic fibrosis and cirrhosis, fat malabsorption, coagulopathies, and renal failure. Evaluation involves history, exam, liver function tests and imaging like ultrasound or MRCP to identify the level and cause of obstruction. Management depends on the specific cause but may include antibiotics, st