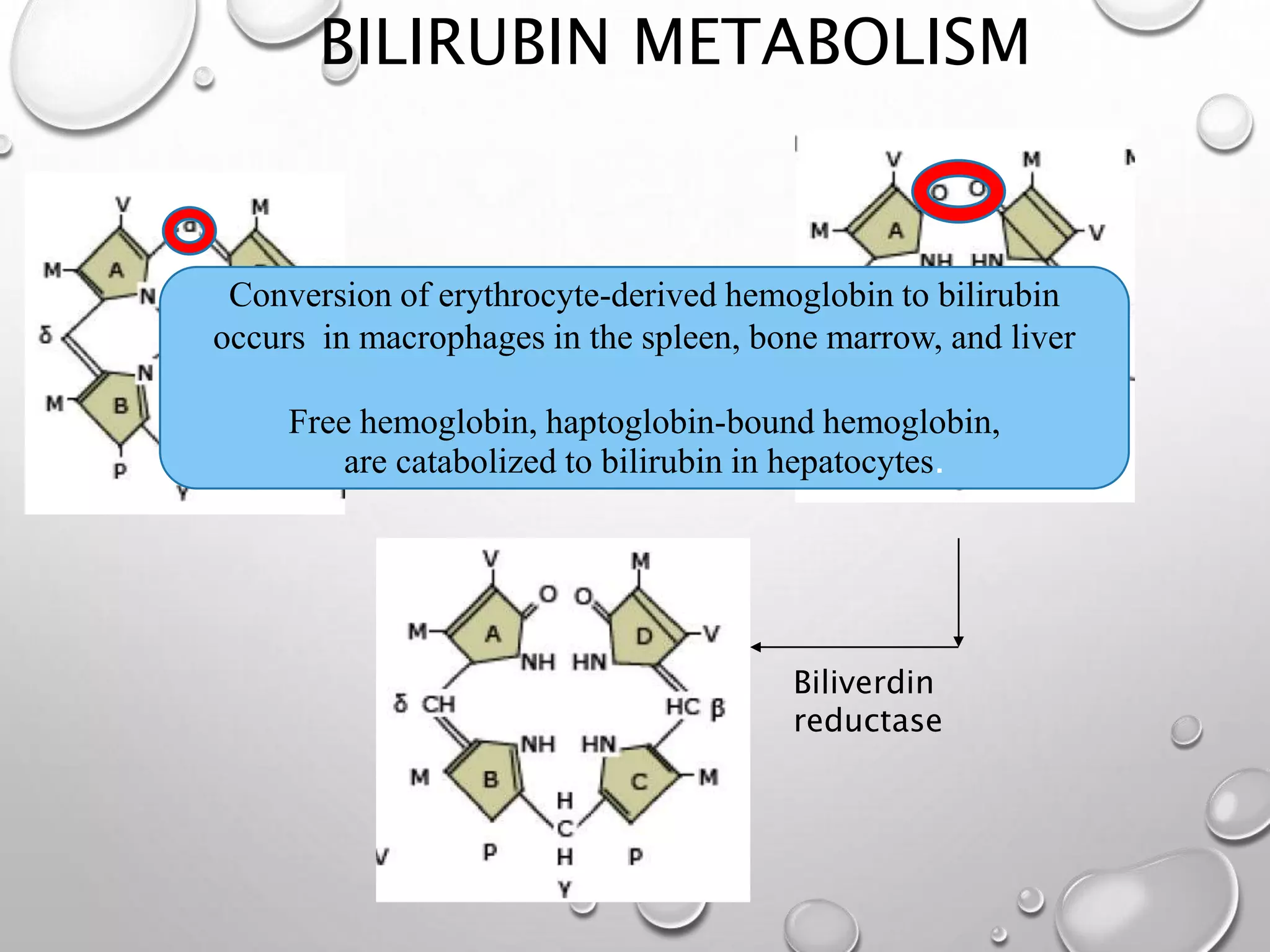
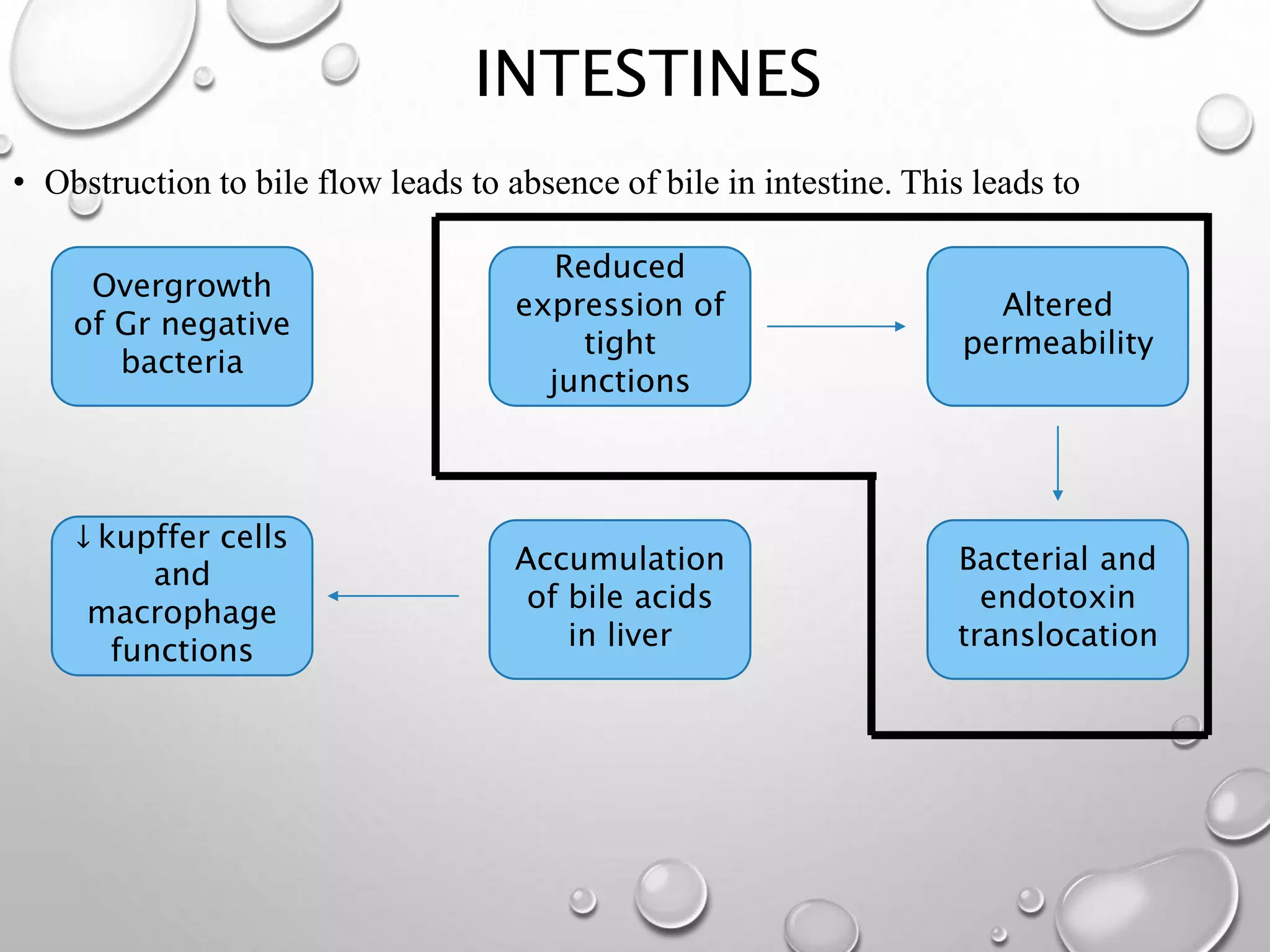
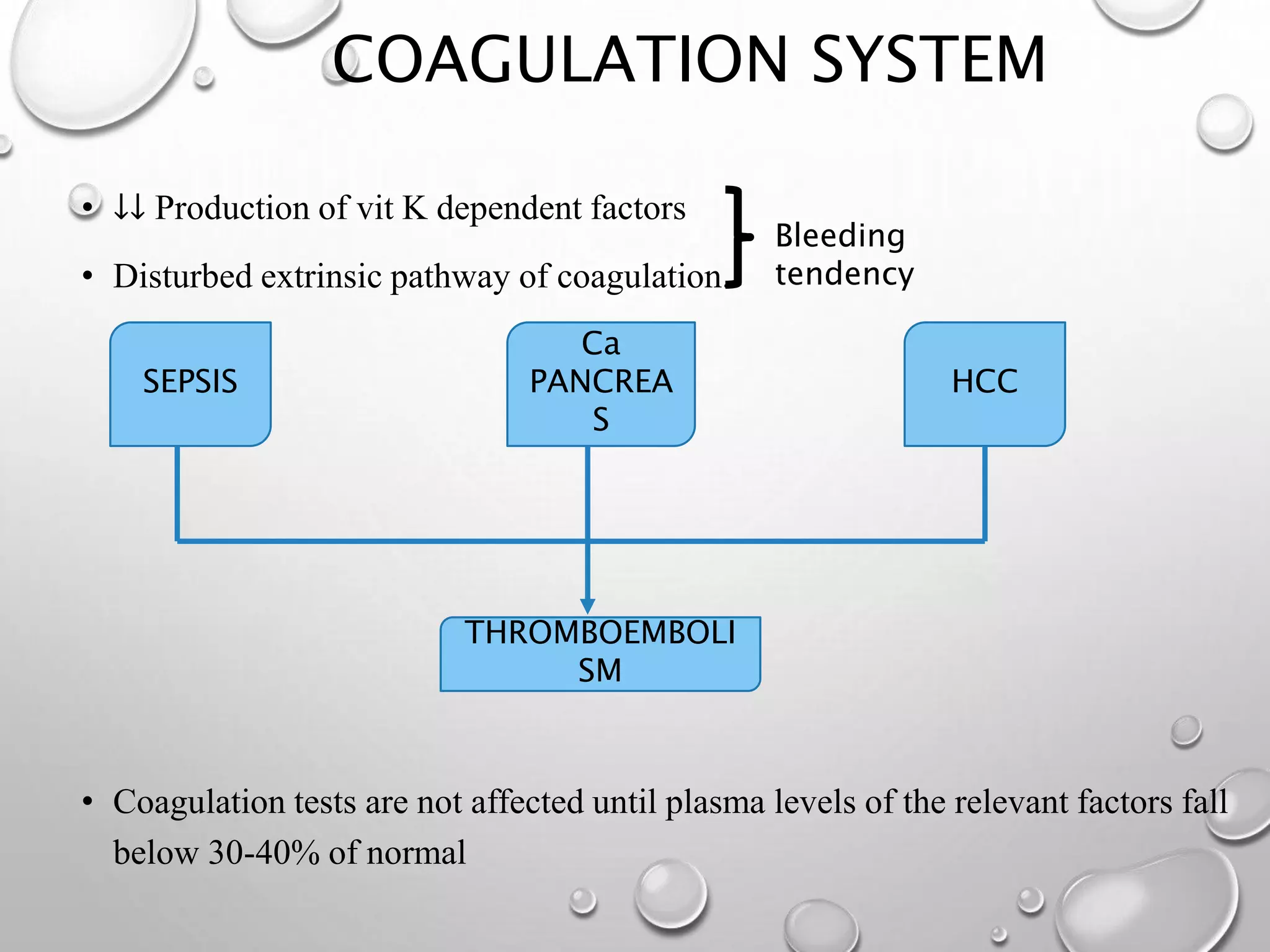
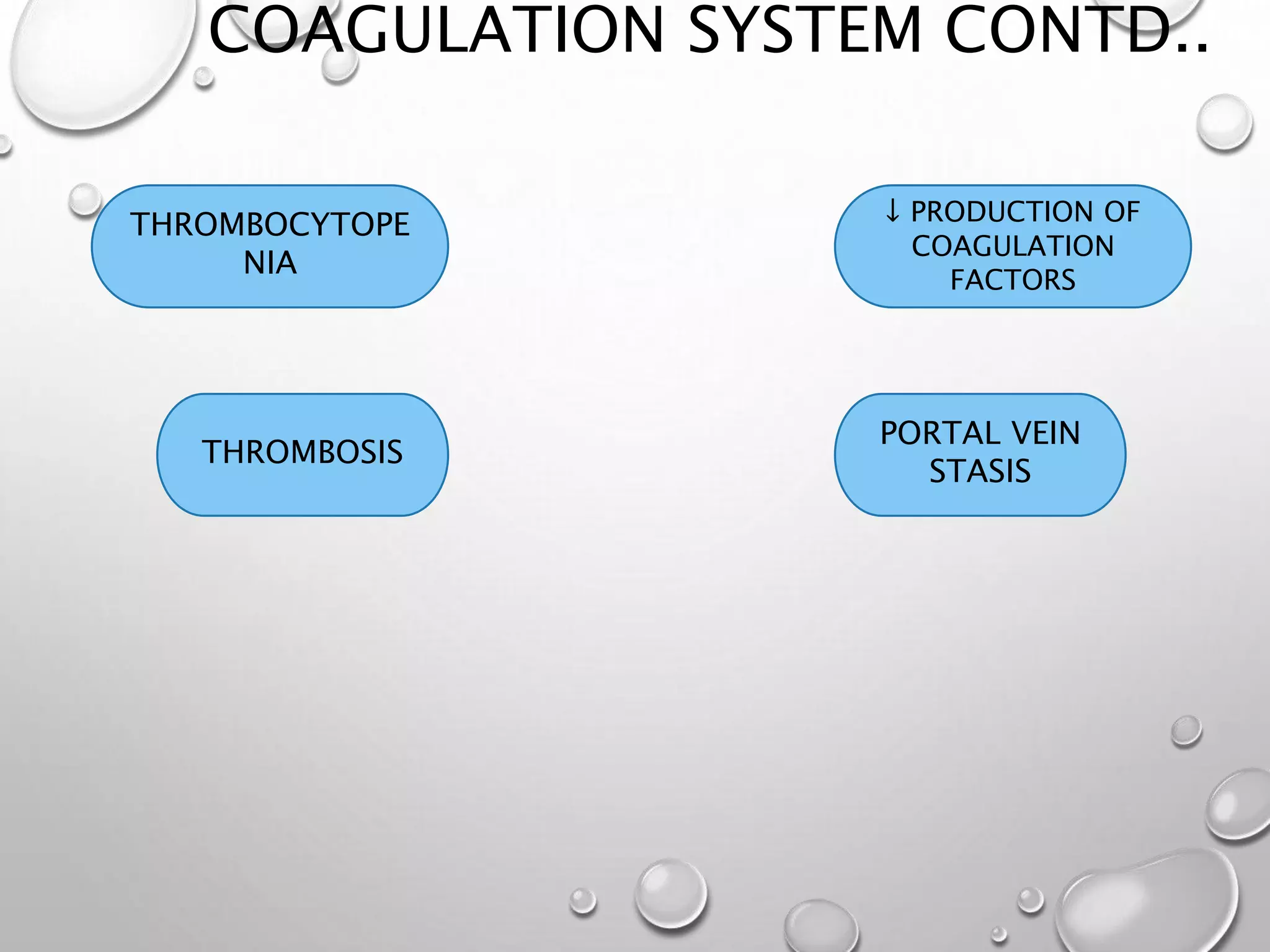
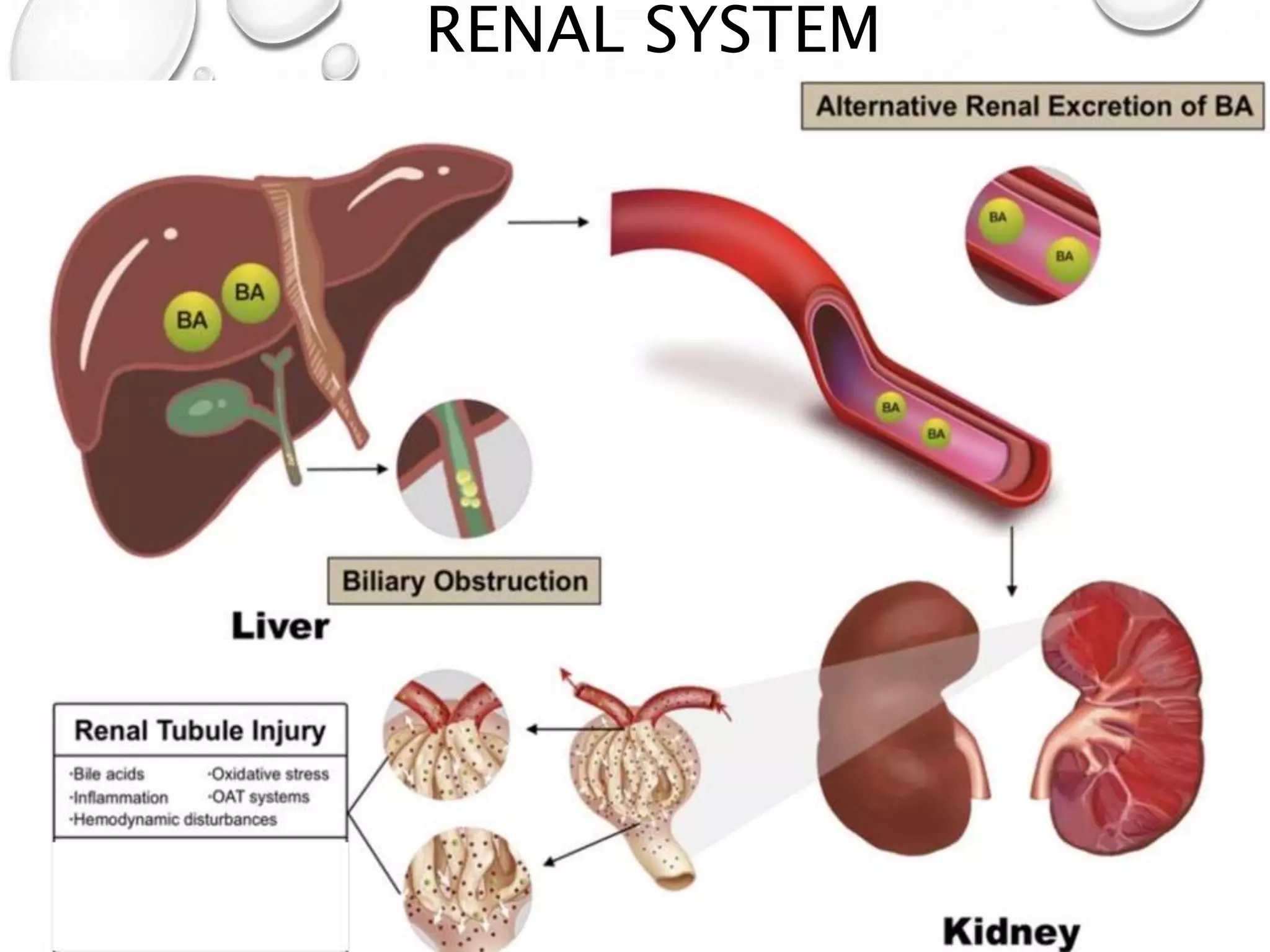
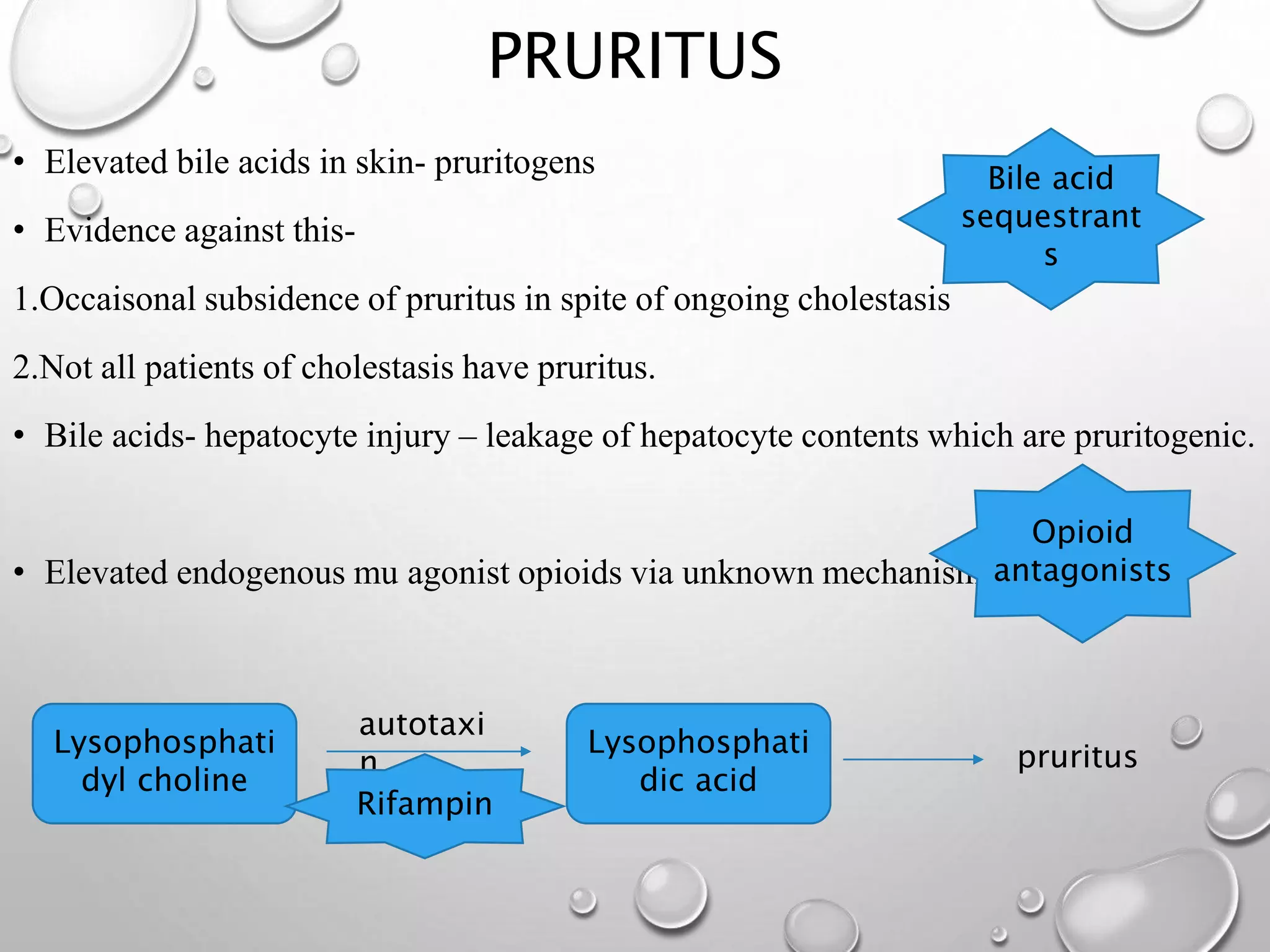
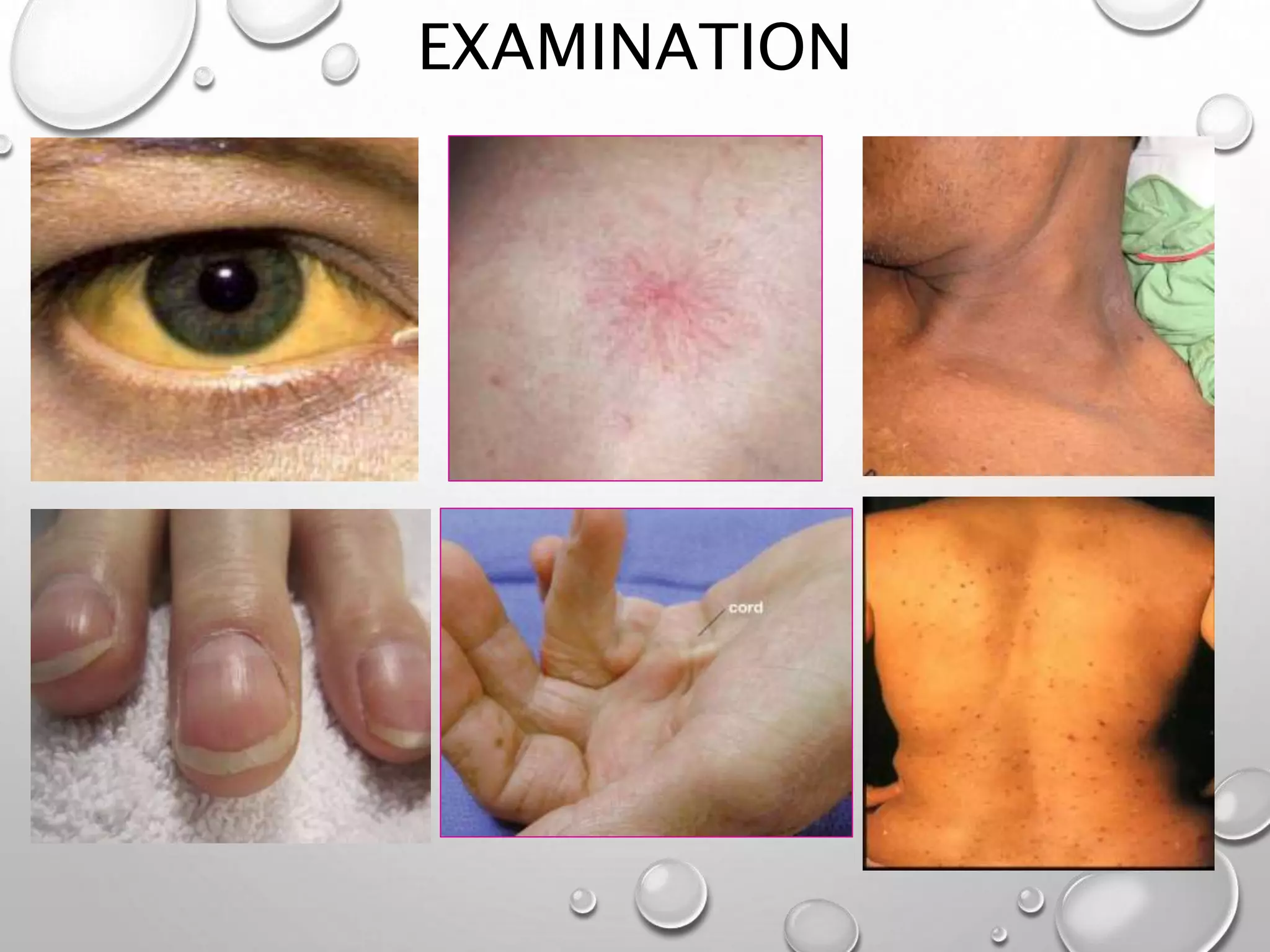
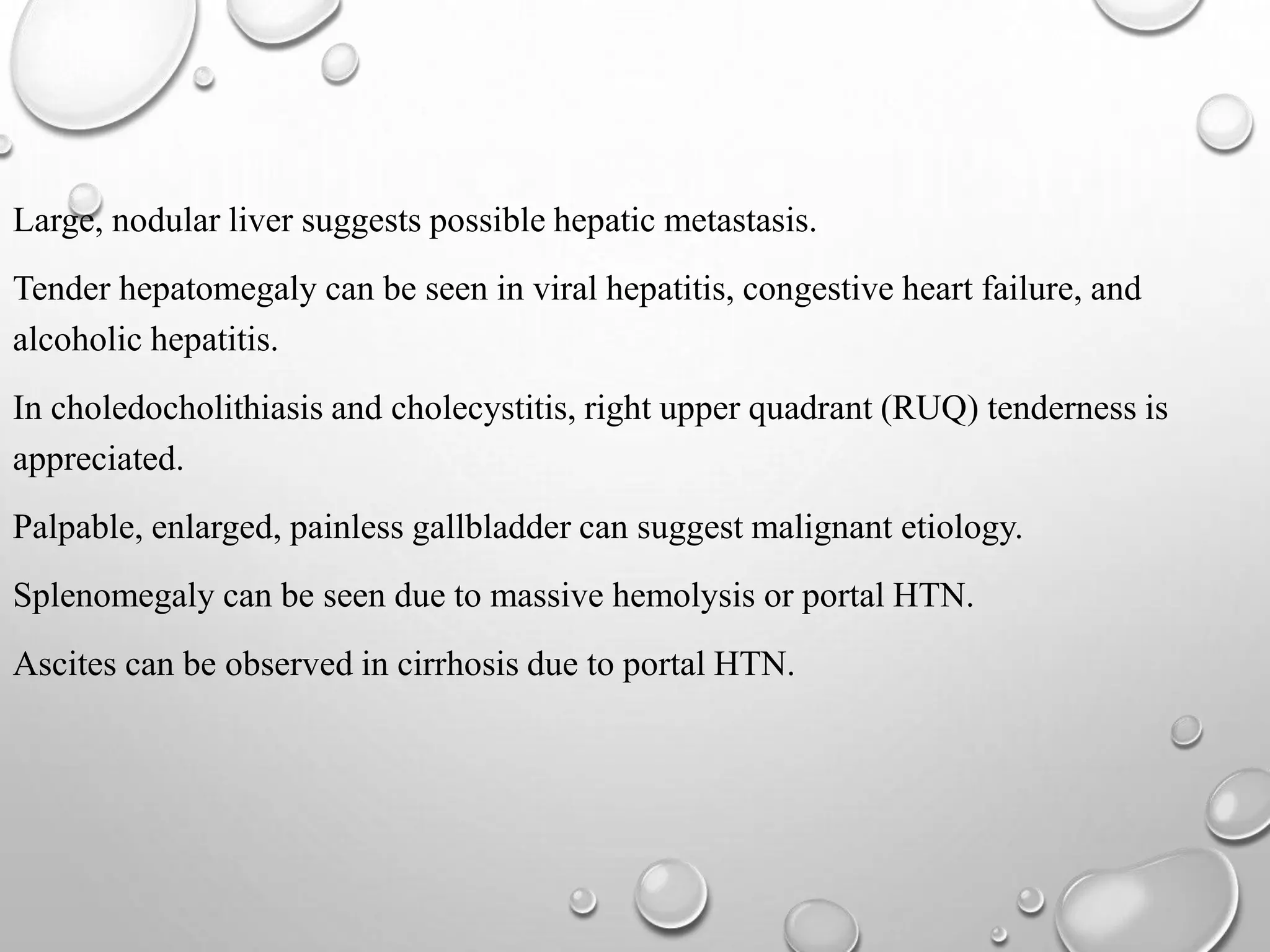
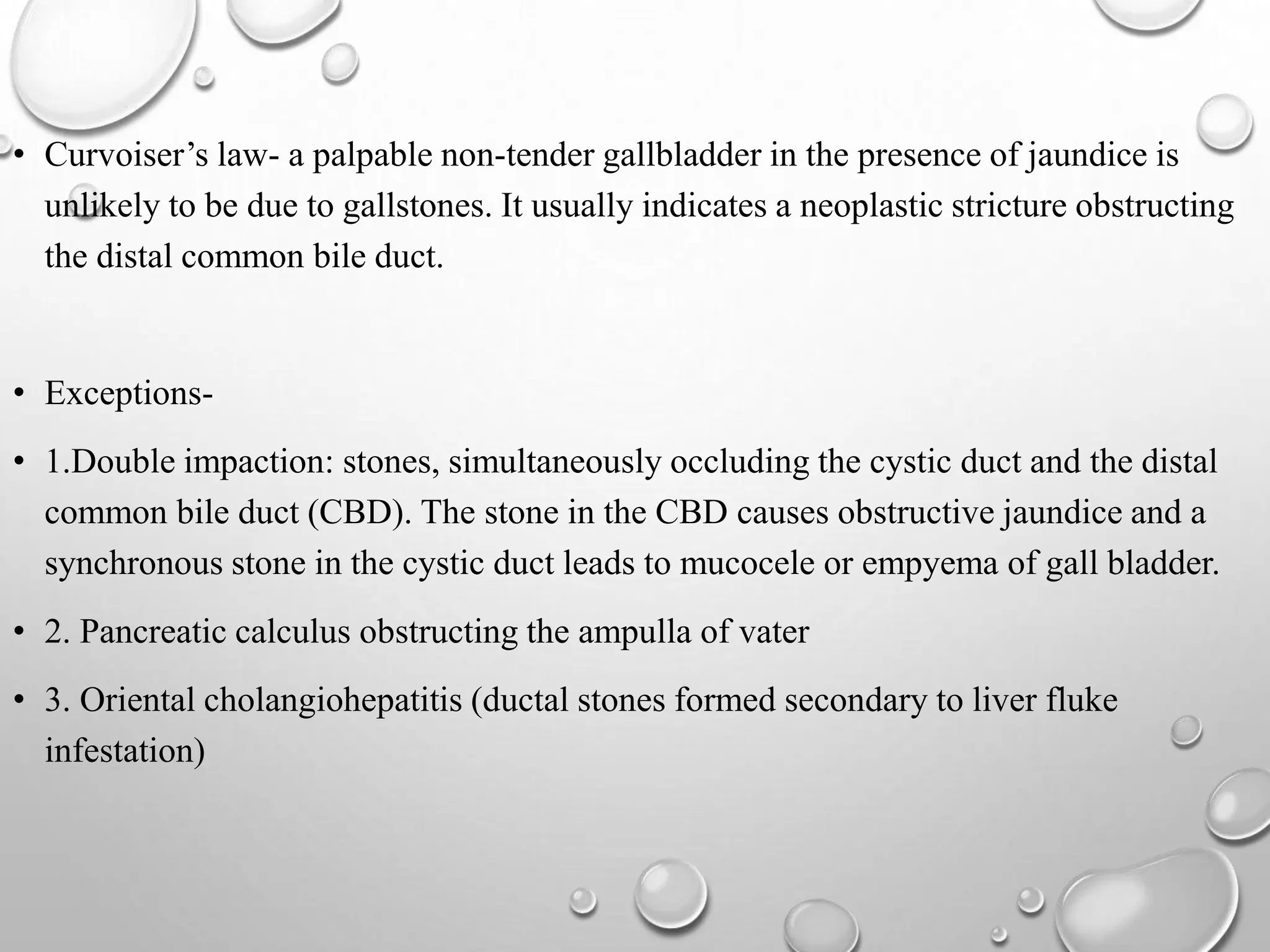
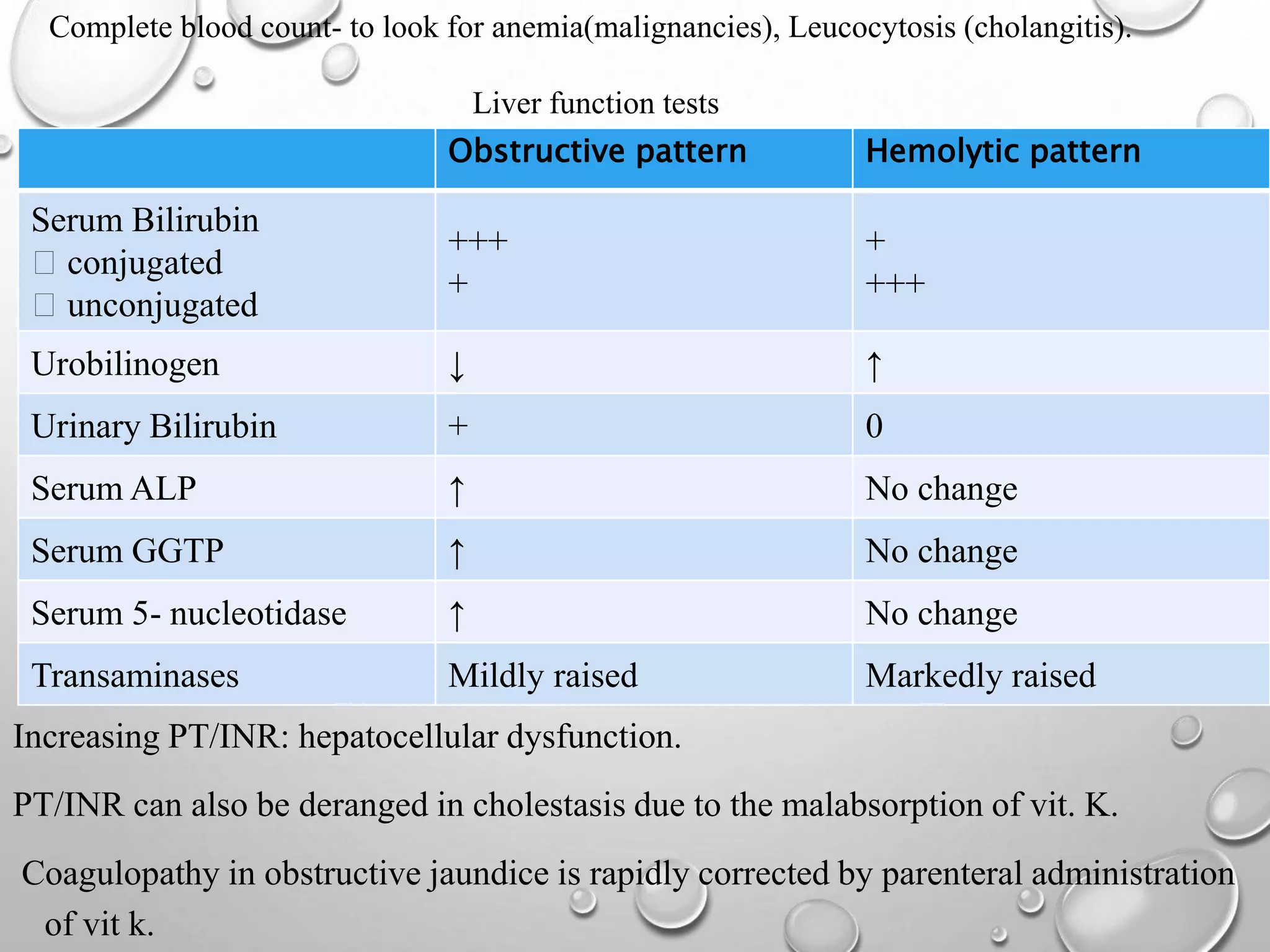
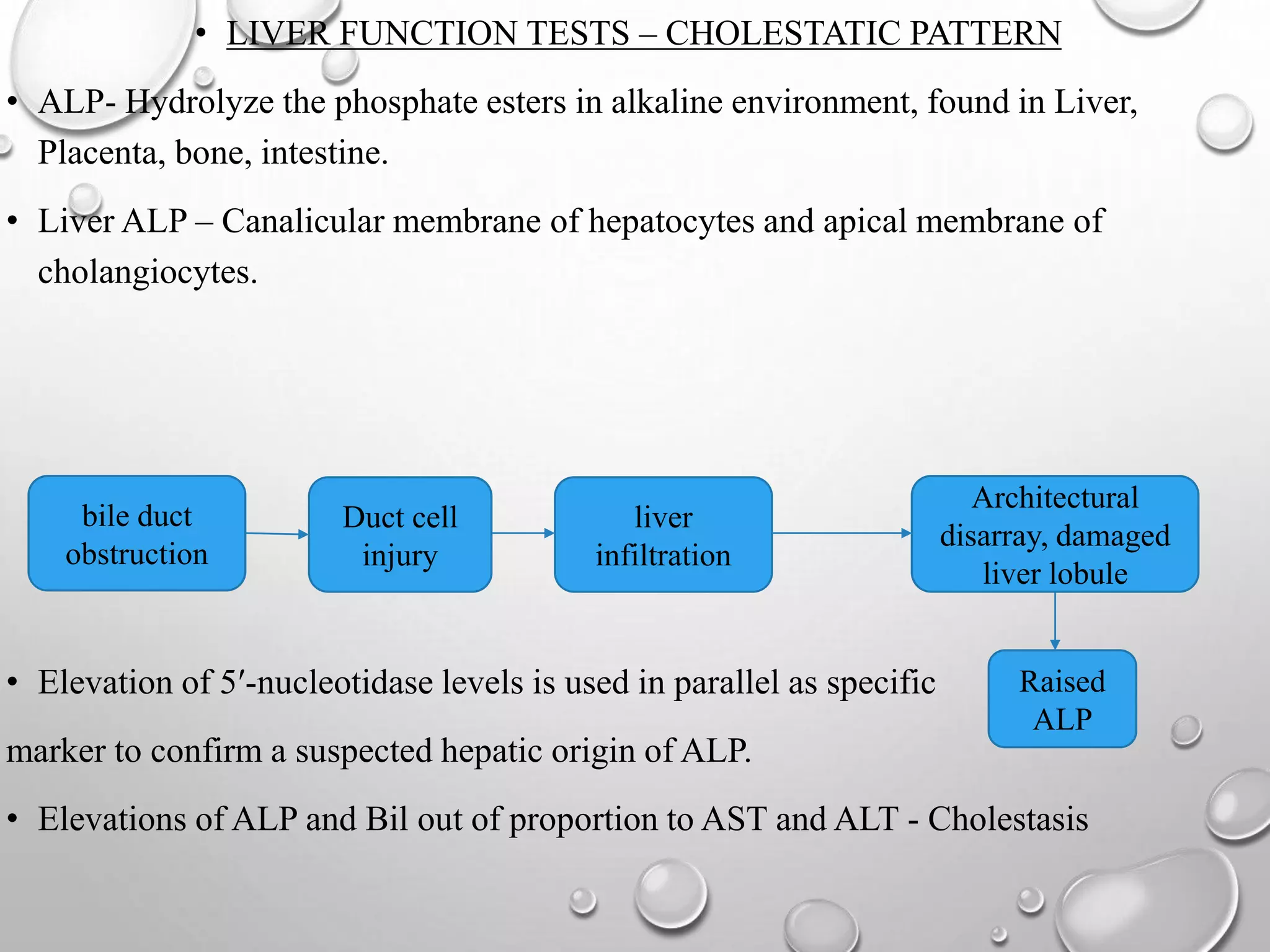
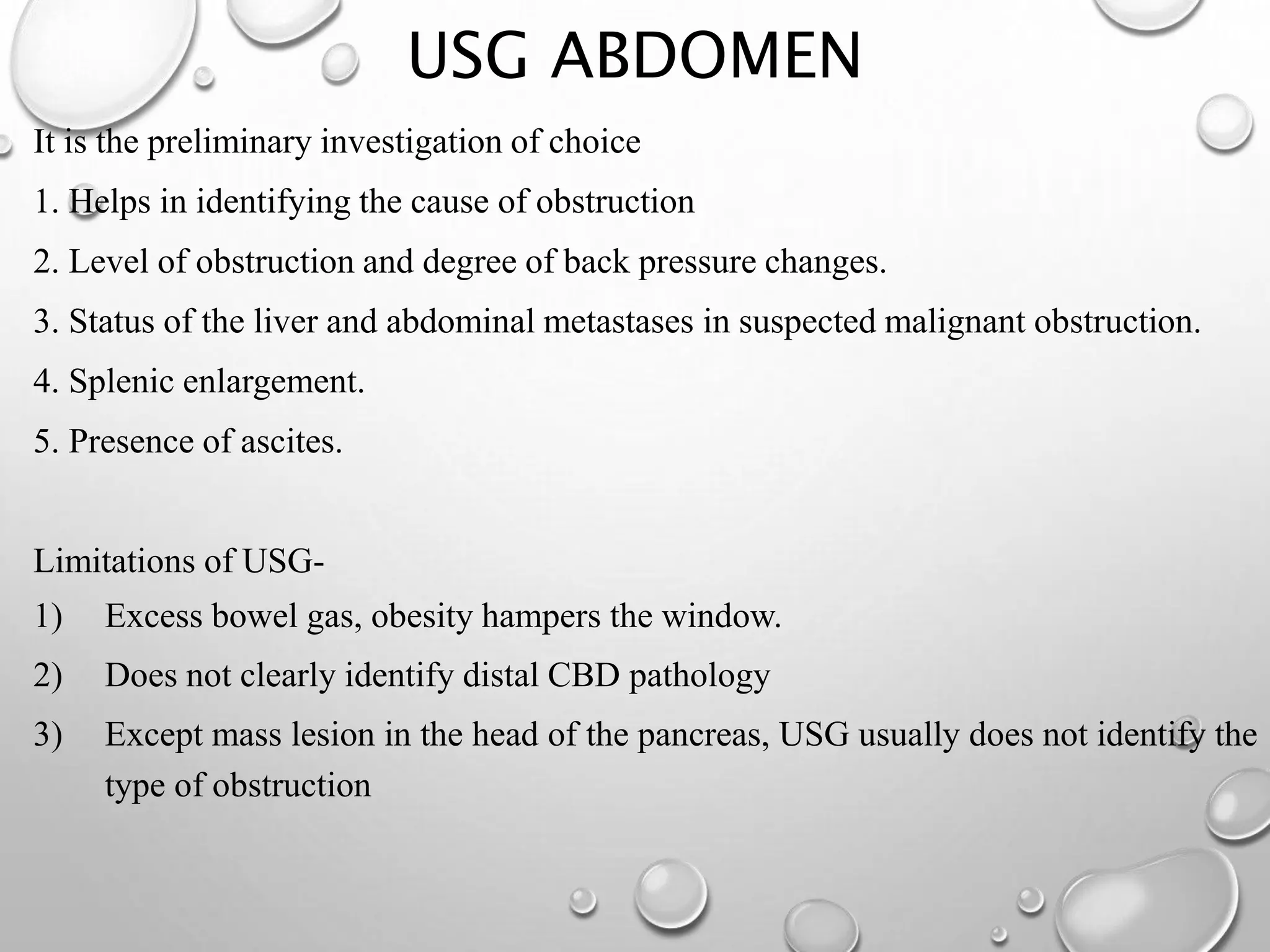
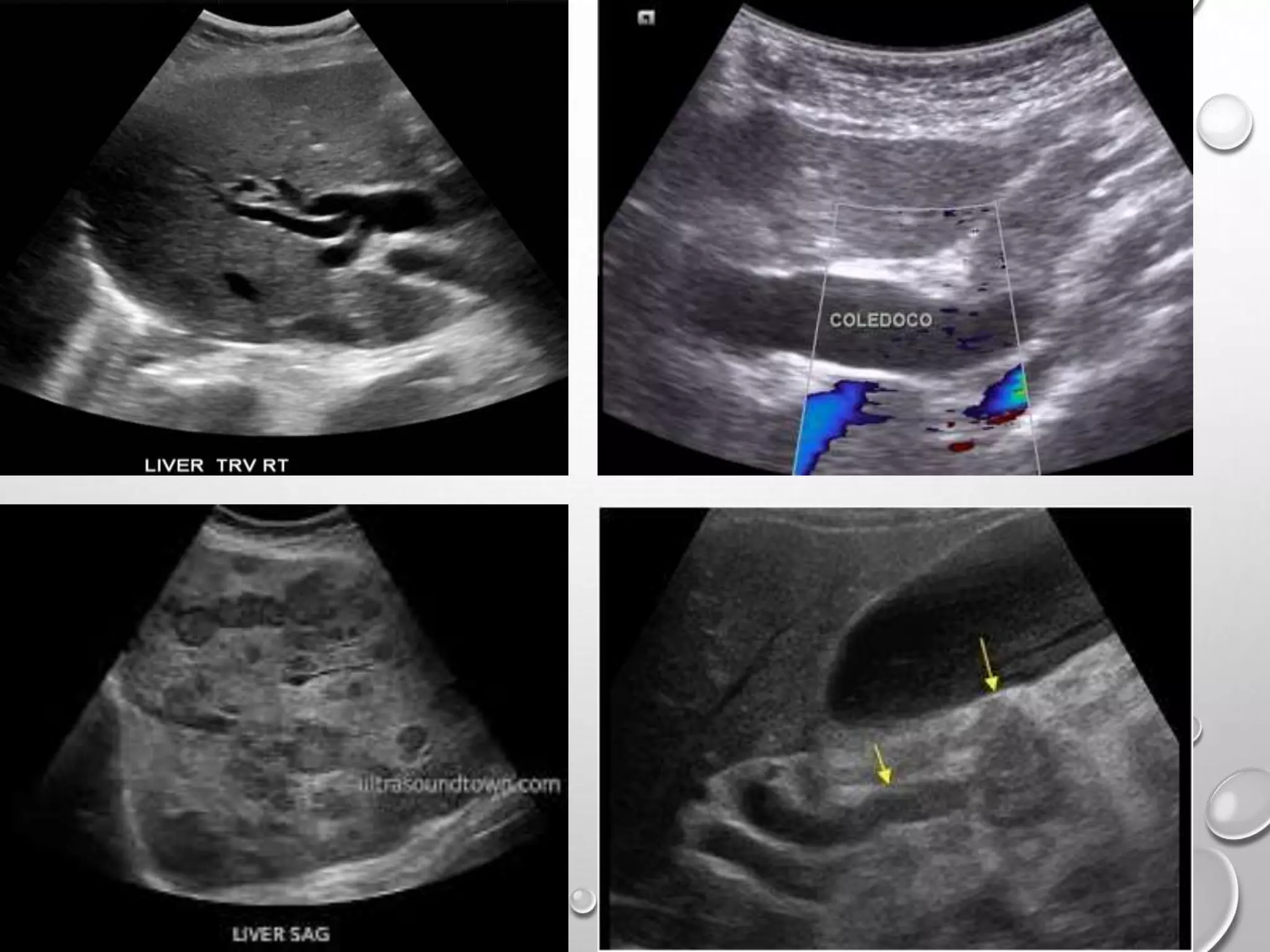
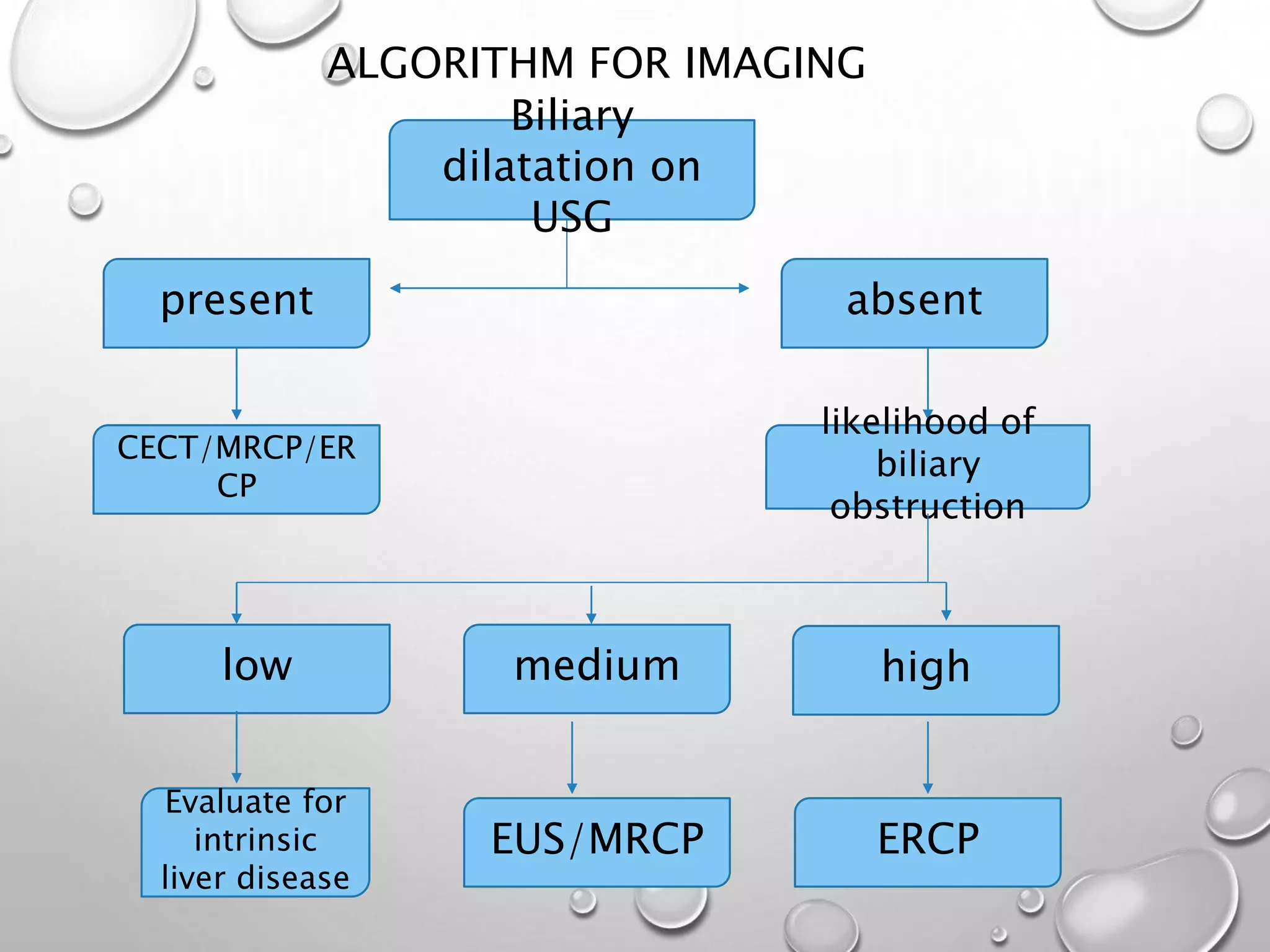
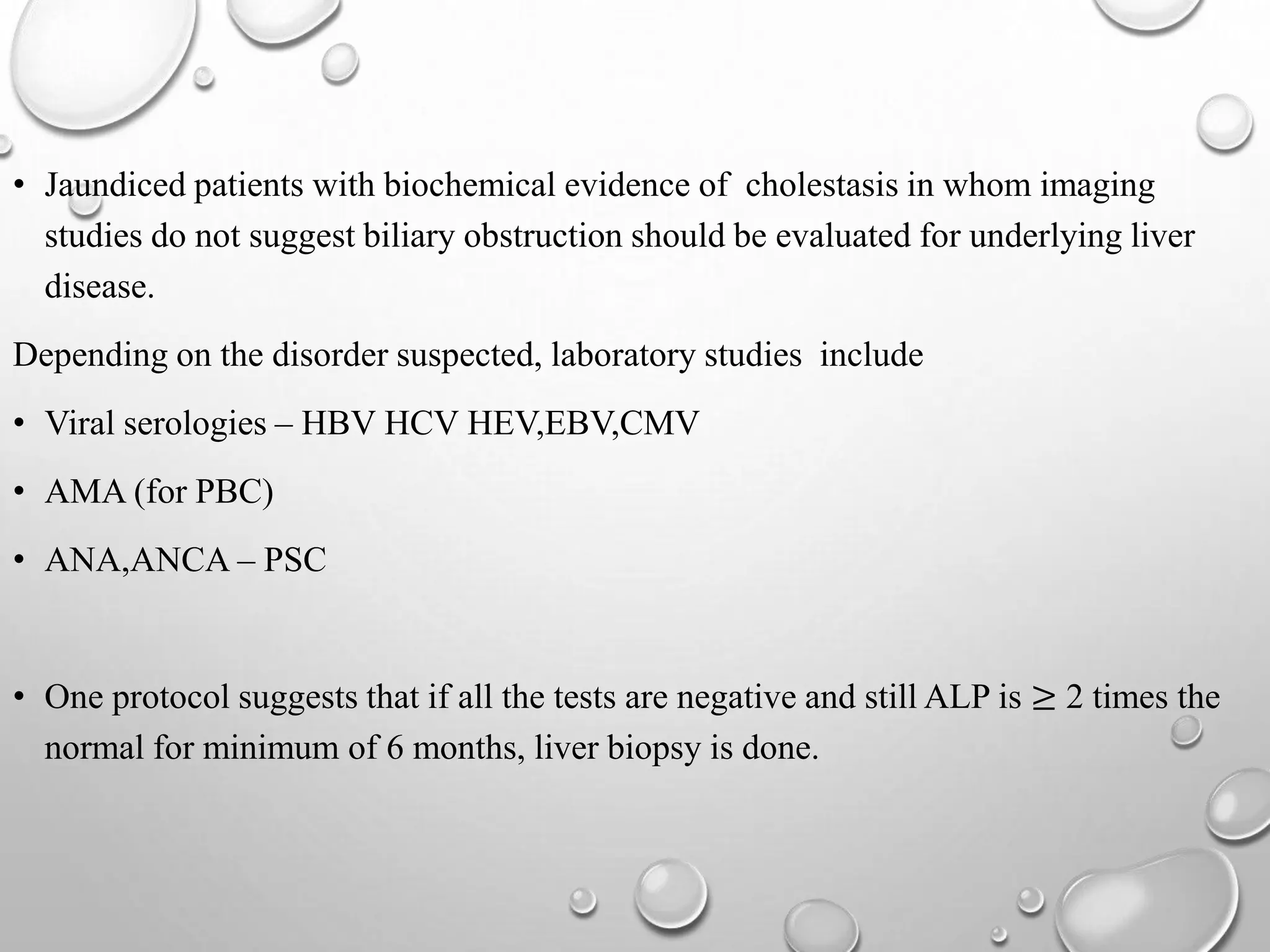
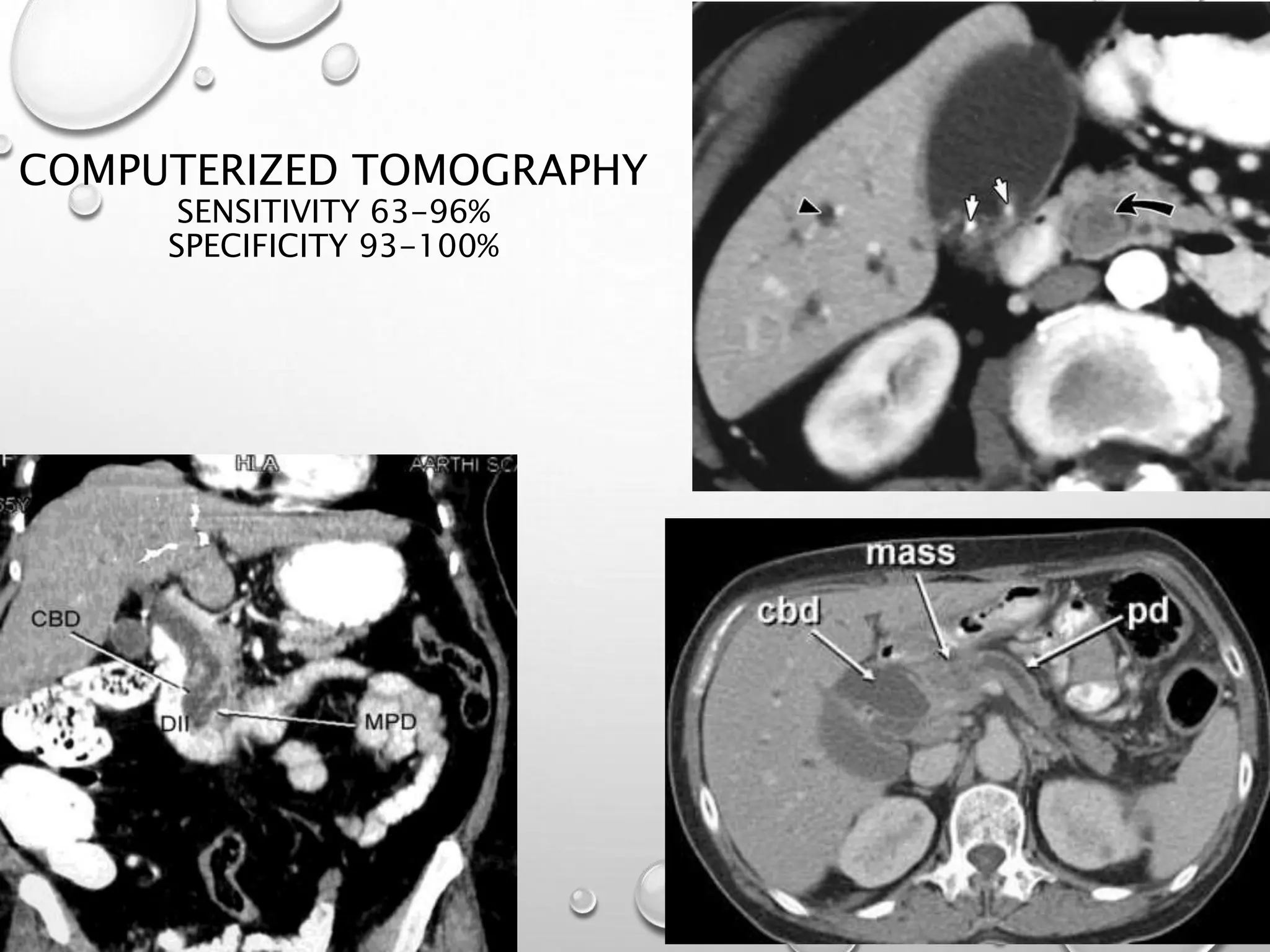
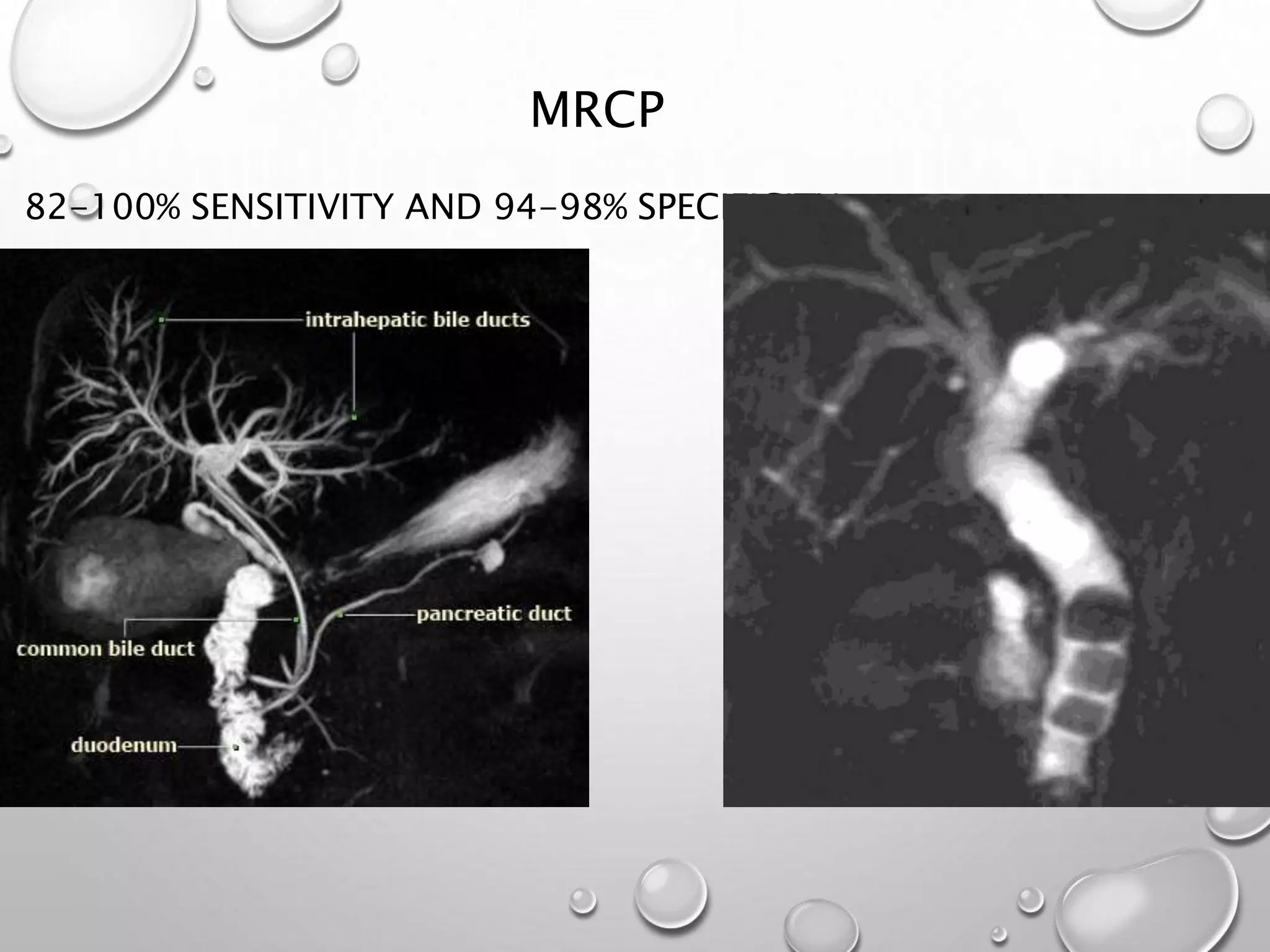
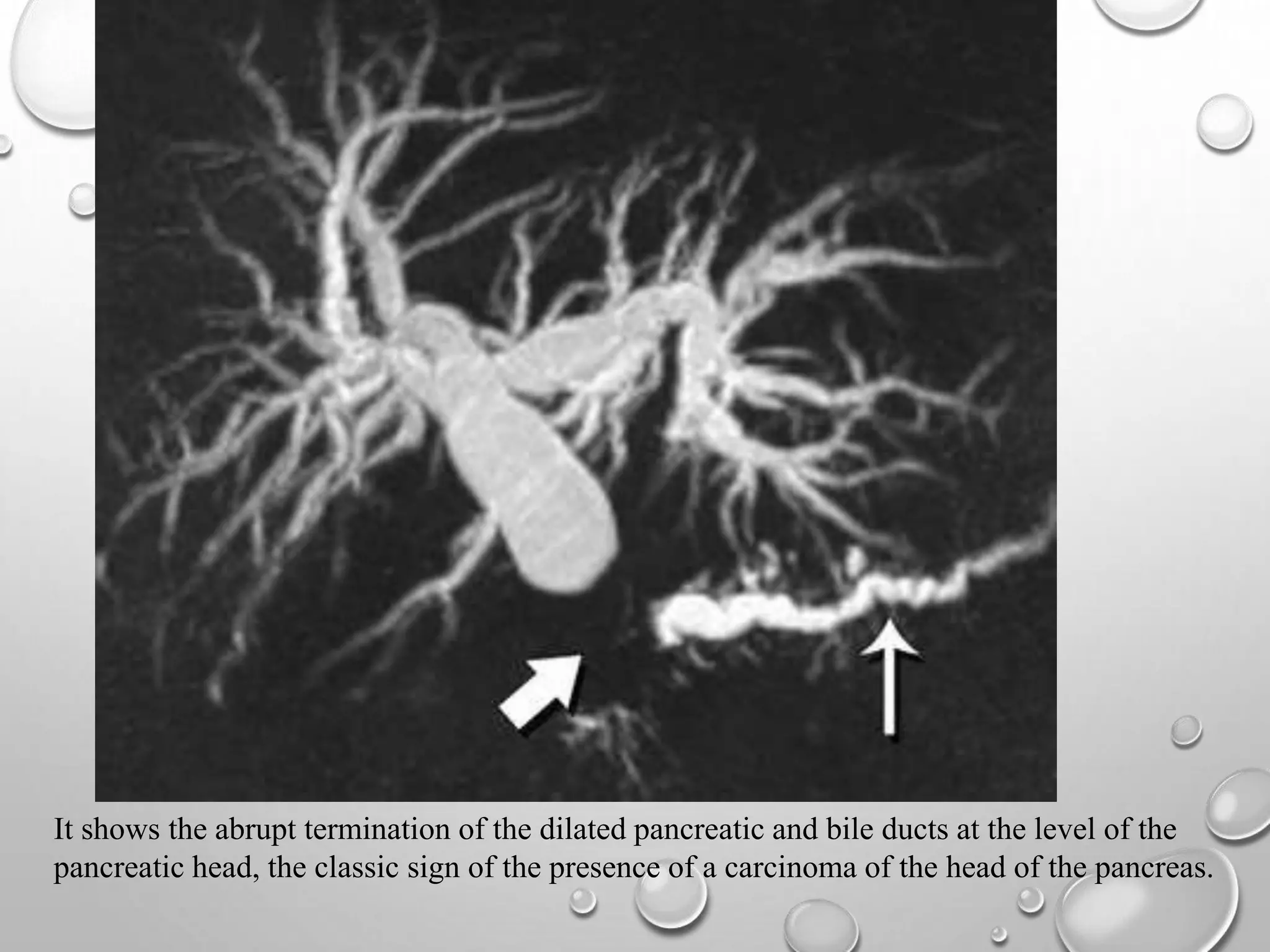
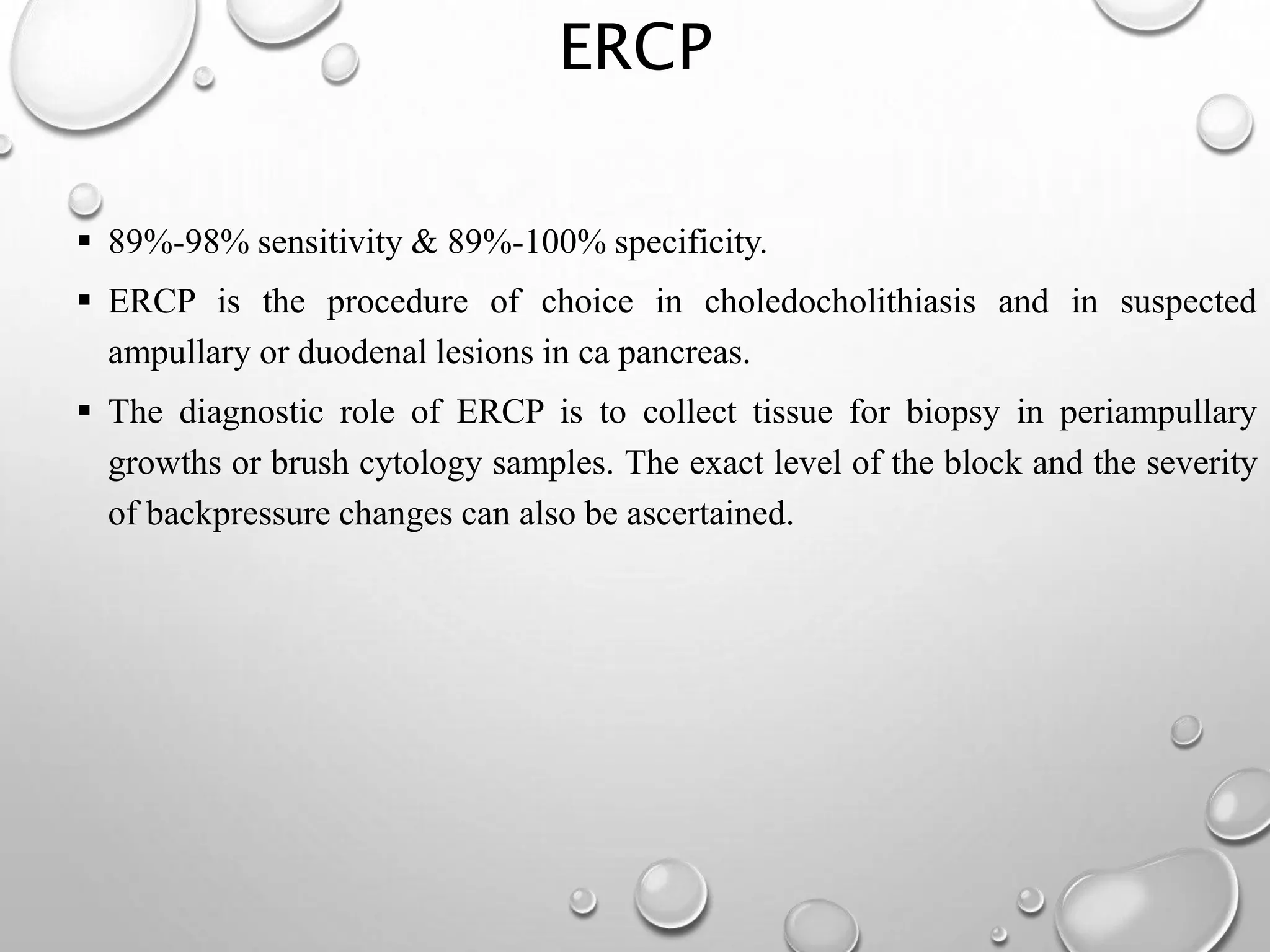
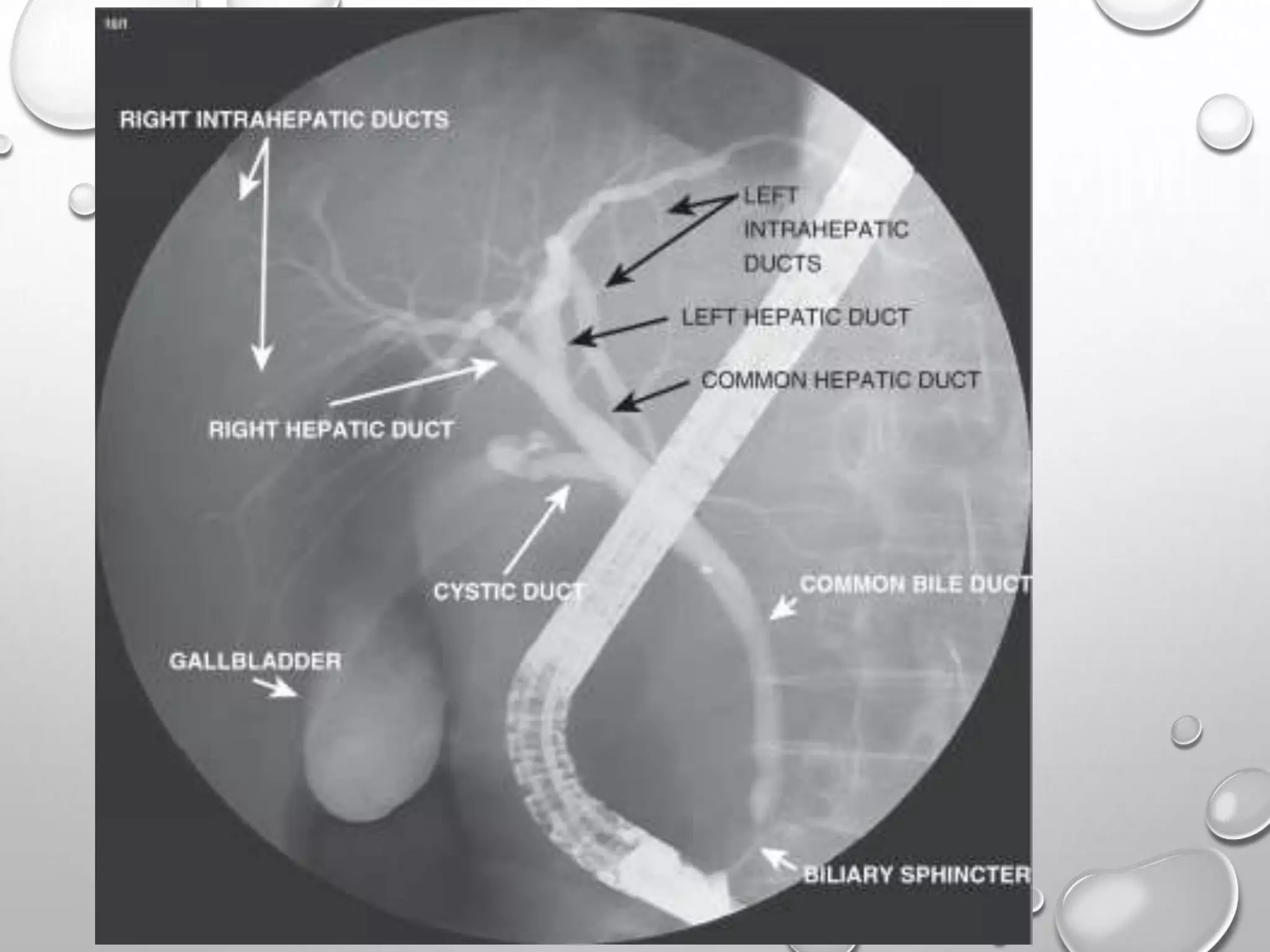
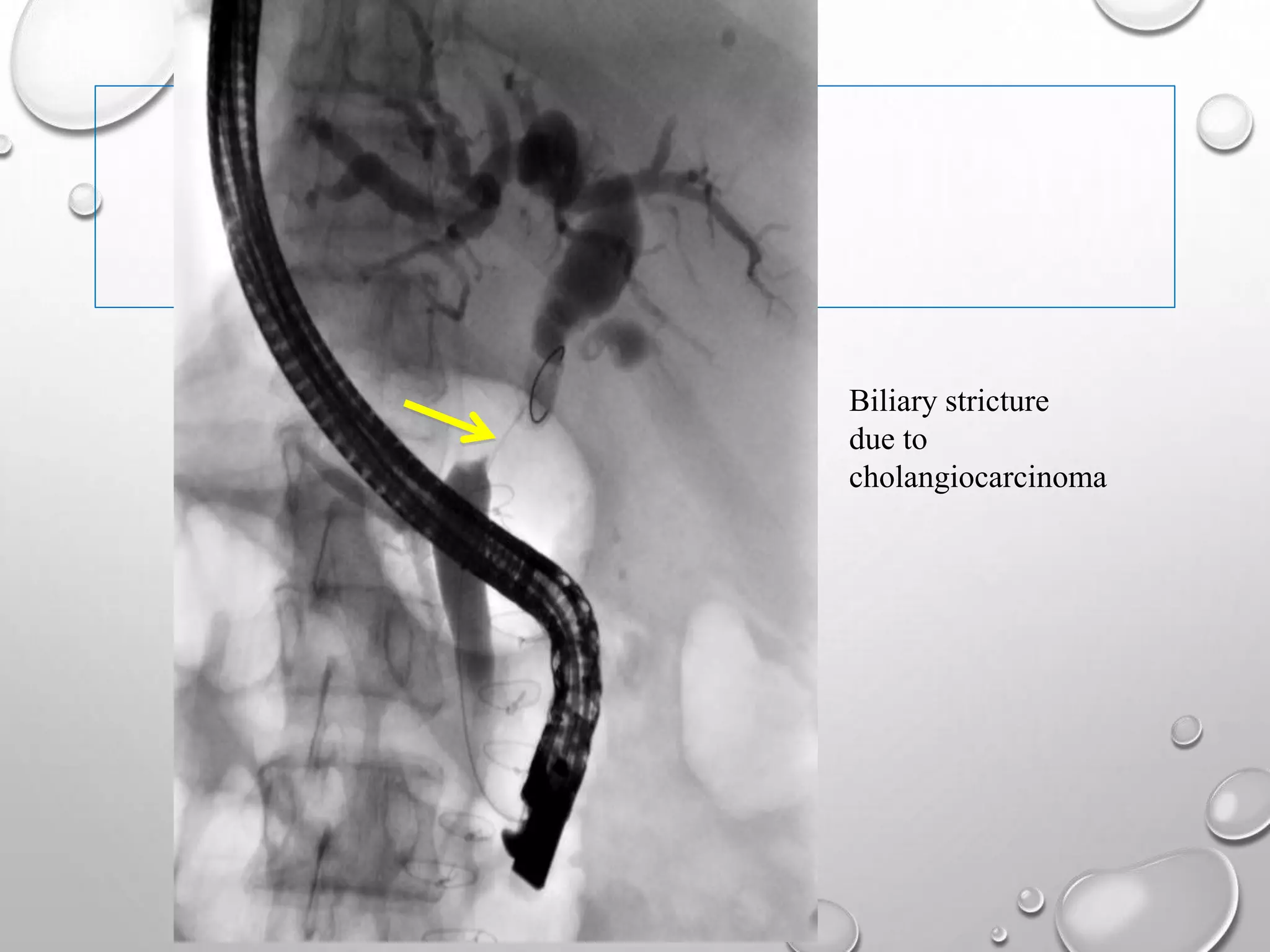
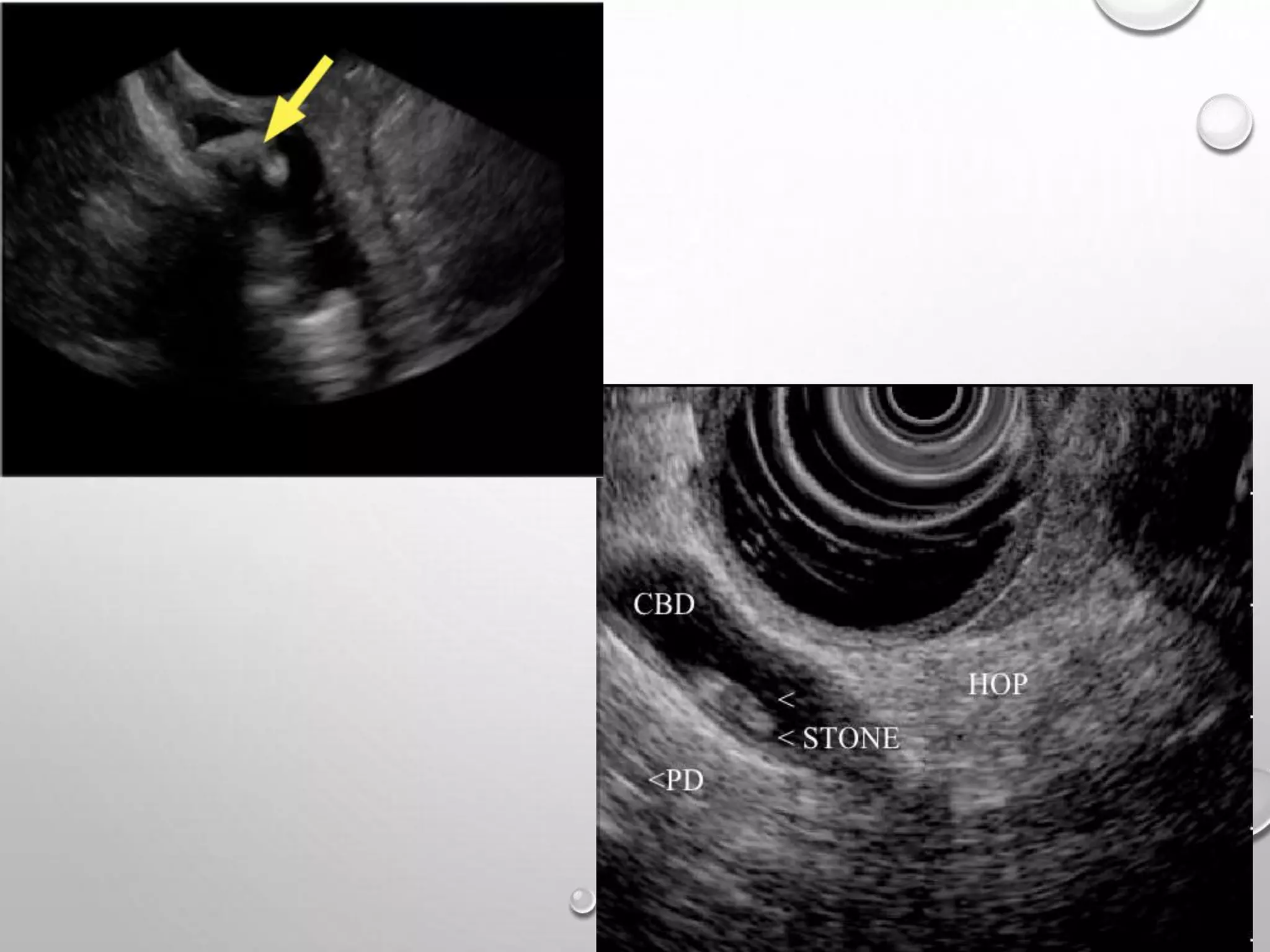
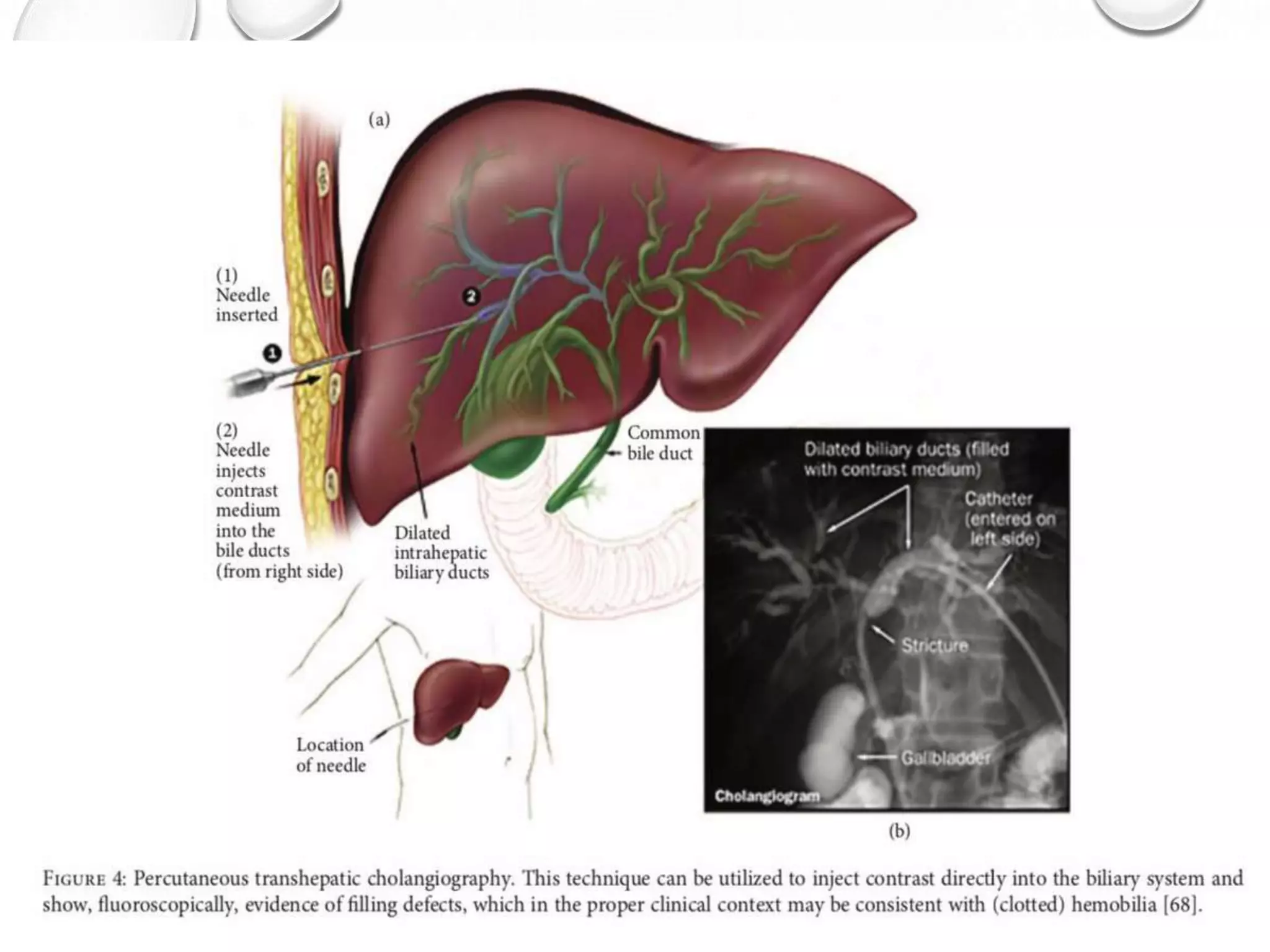
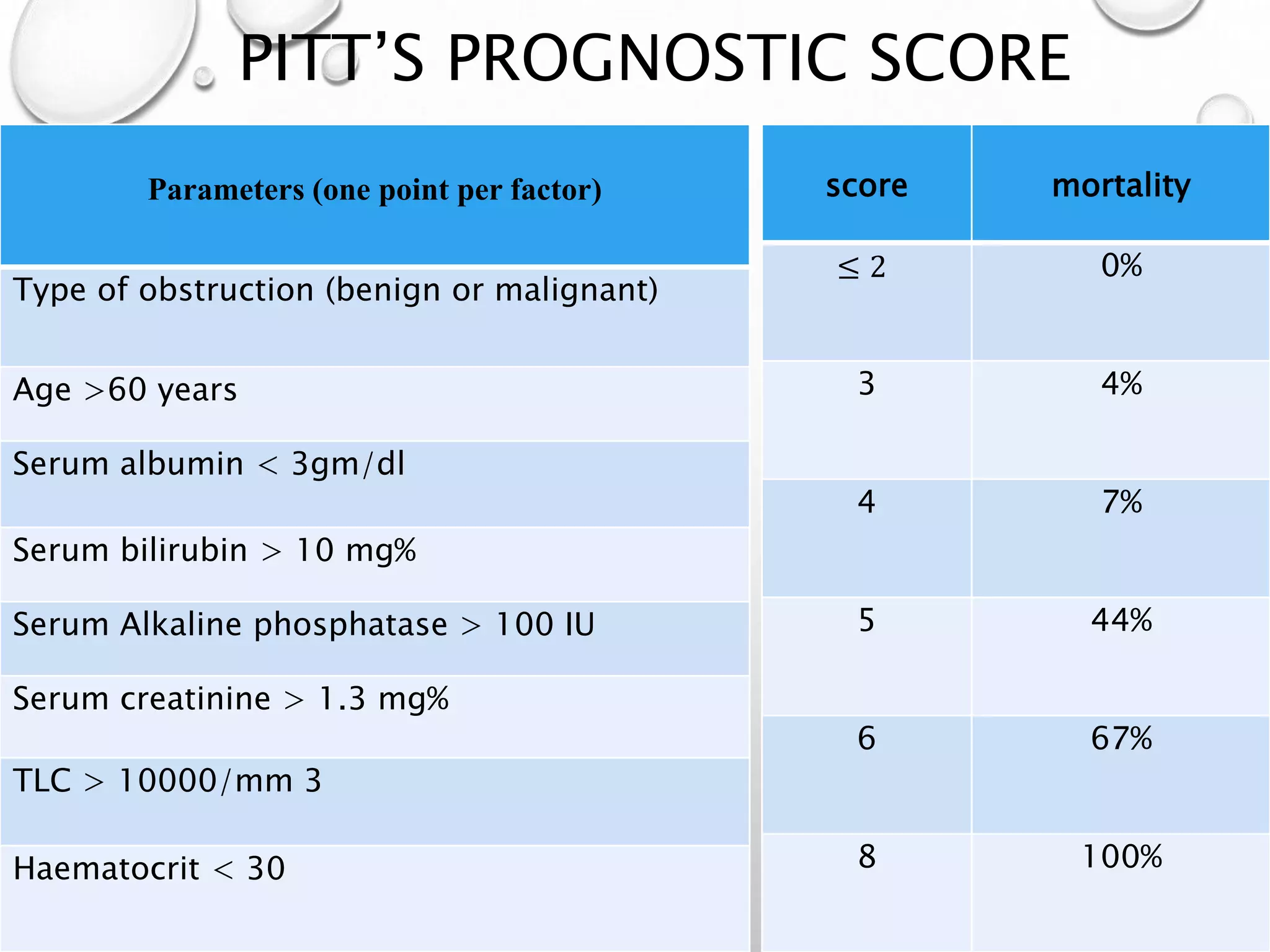
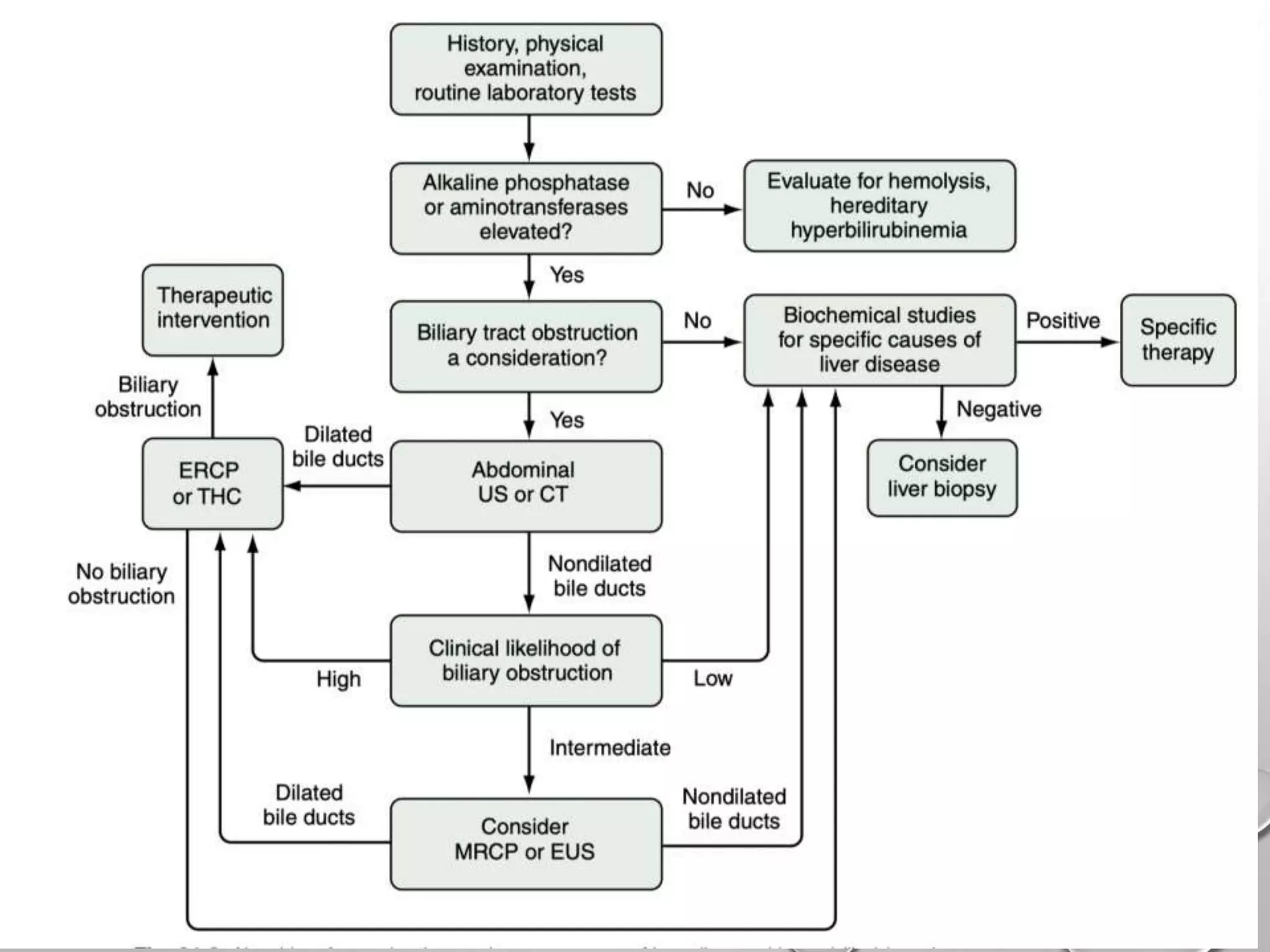
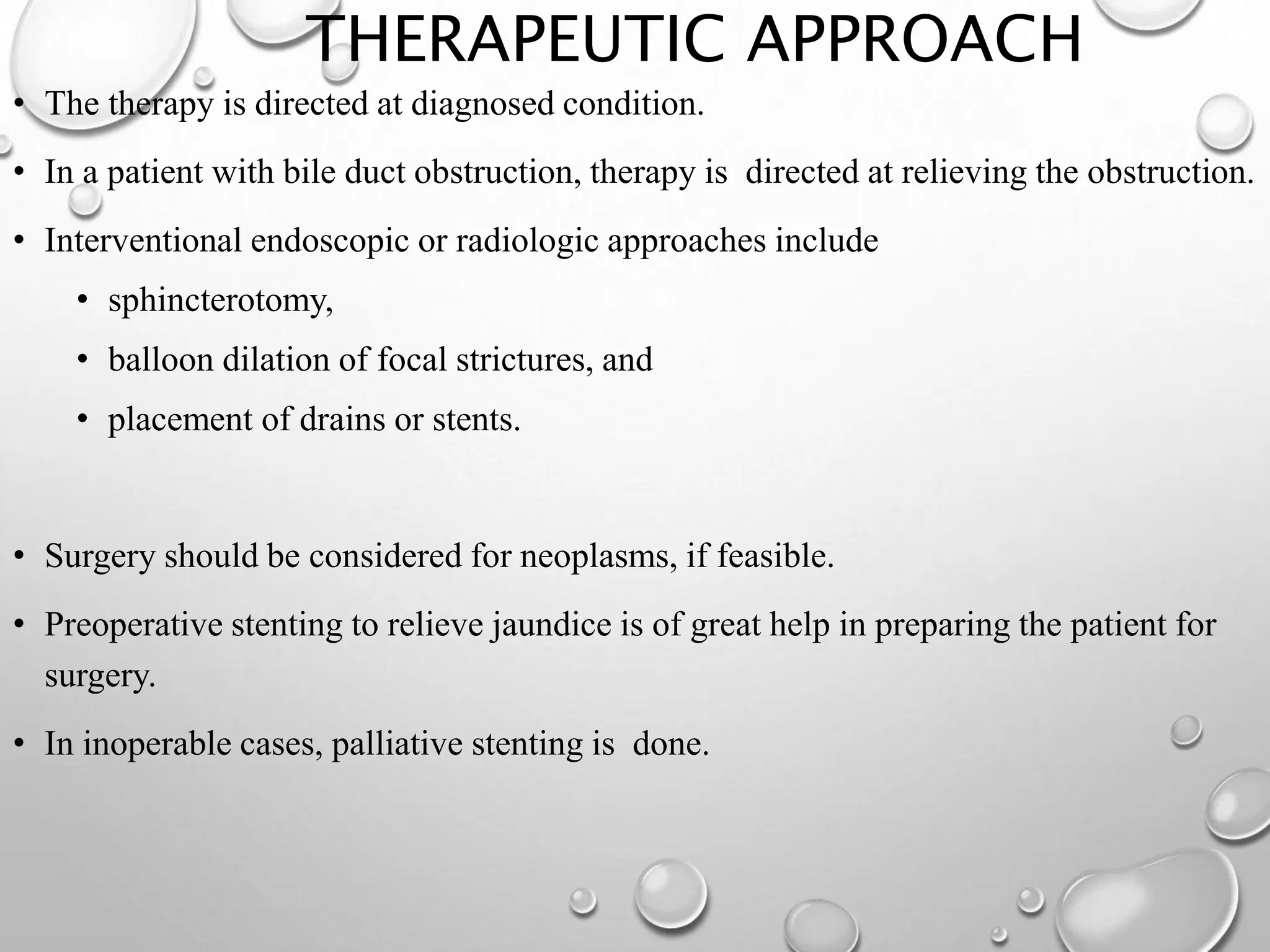
This document discusses obstructive jaundice and approaches to evaluation. It begins by describing the history and definitions of jaundice and obstructive jaundice. It then discusses the effects of biliary obstruction on various organ systems including the intestines, coagulation, renal, hepatic, and dermatologic systems. The document outlines the clinical evaluation of a patient with obstructive jaundice including history, examination, and initial investigations. It proposes an algorithm for imaging based on ultrasound findings and evaluates modalities like CT, MRCP, ERCP, EUS, and percutaneous transhepatic cholangiography.