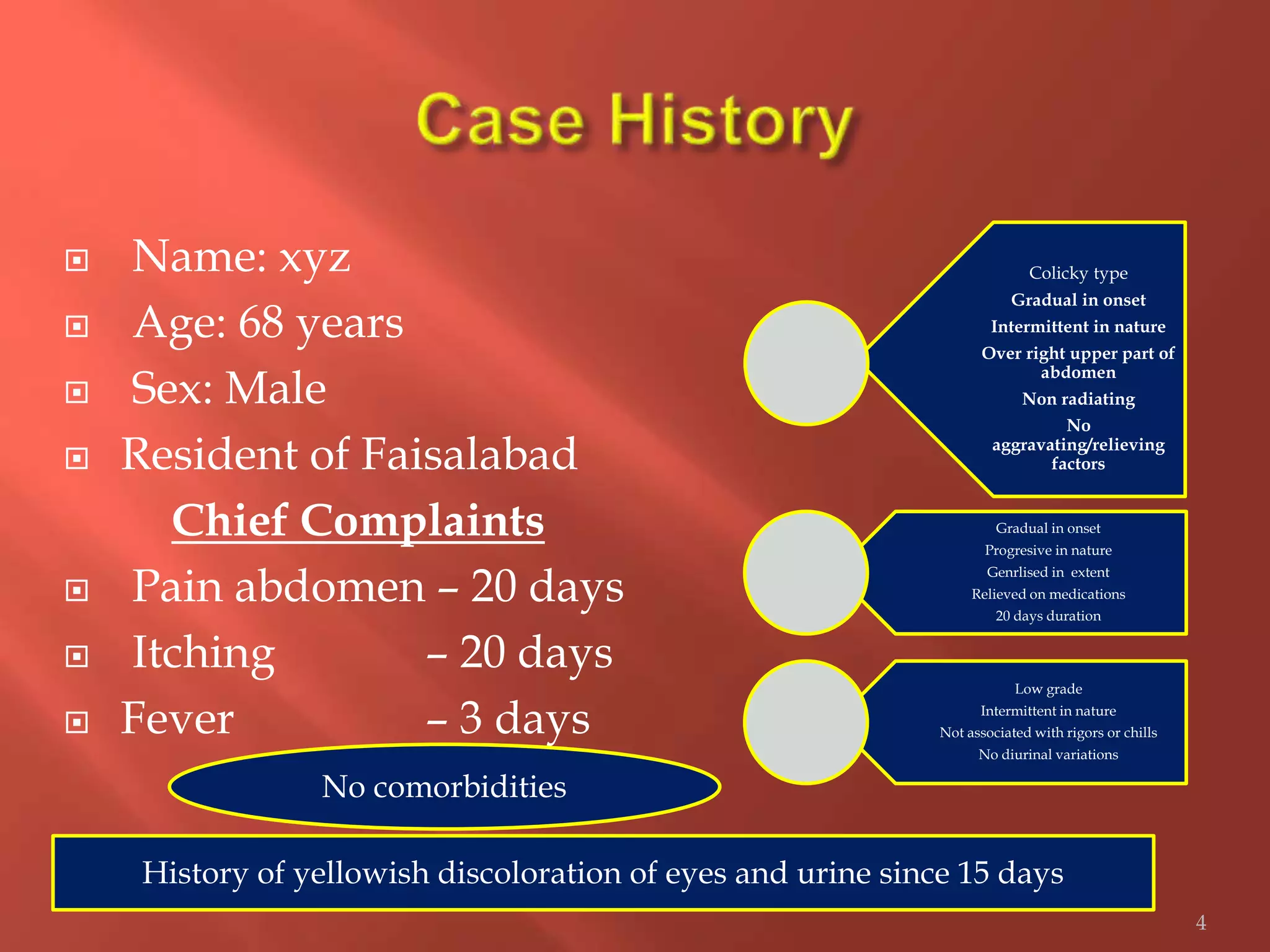
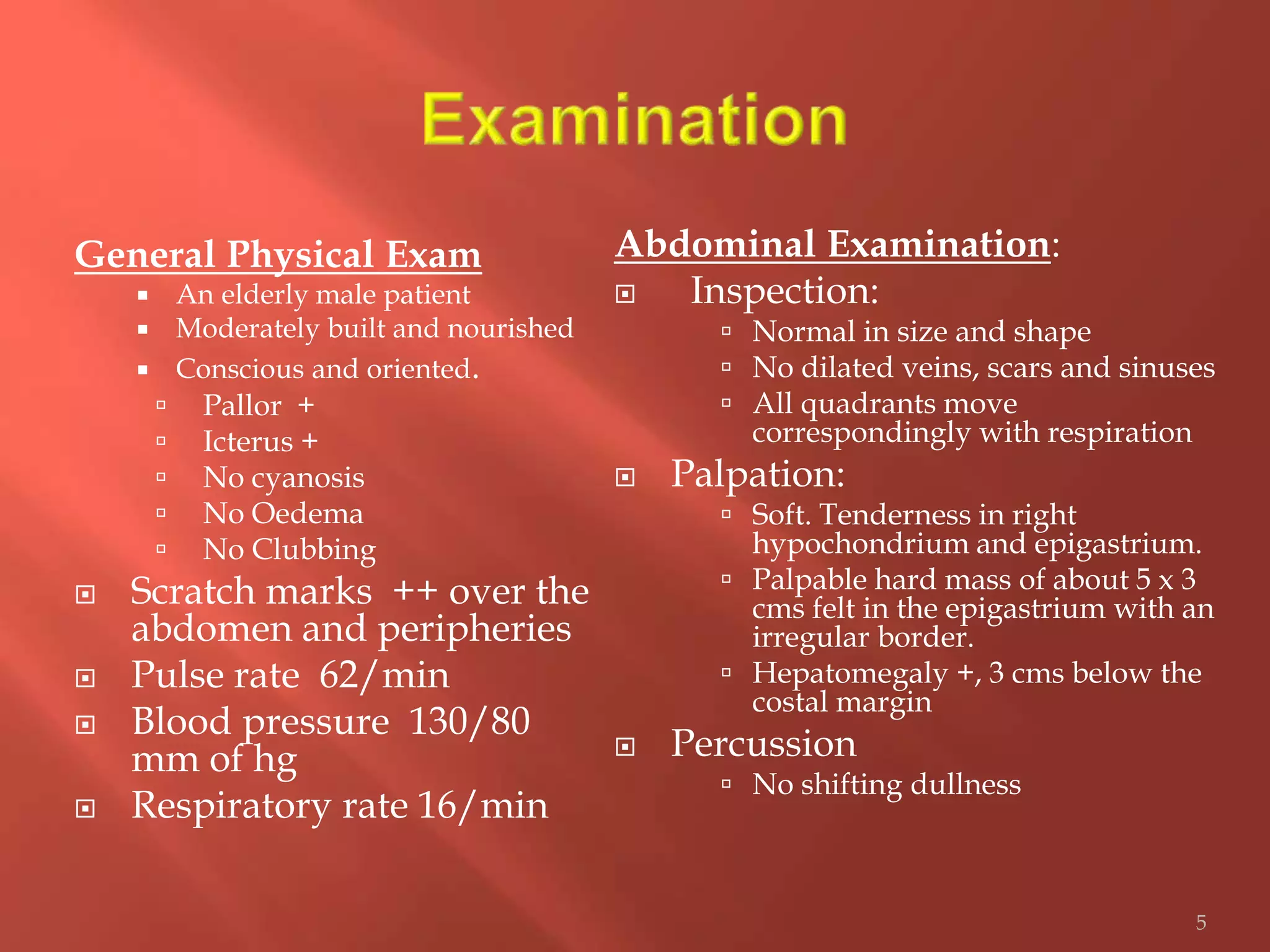
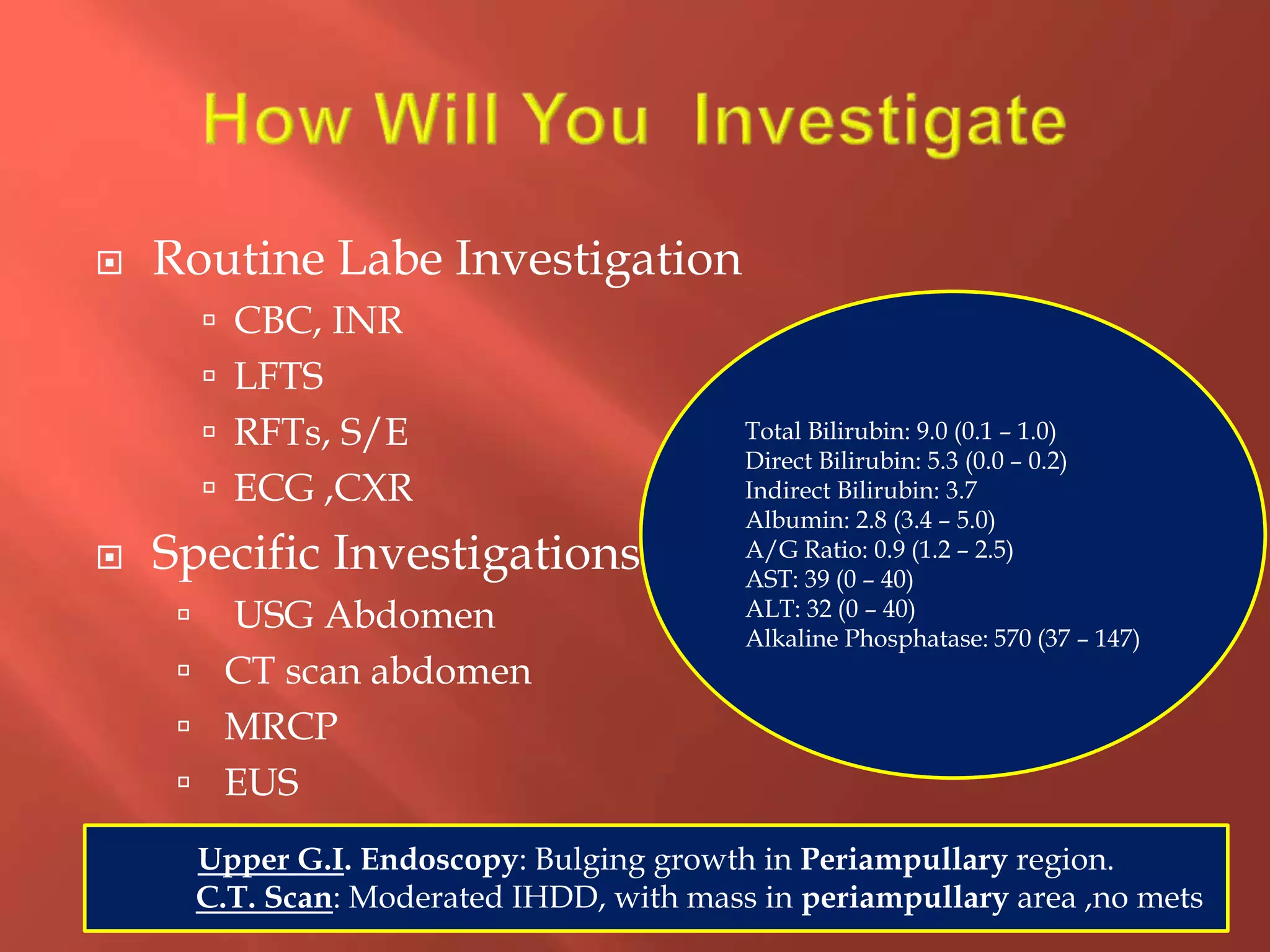
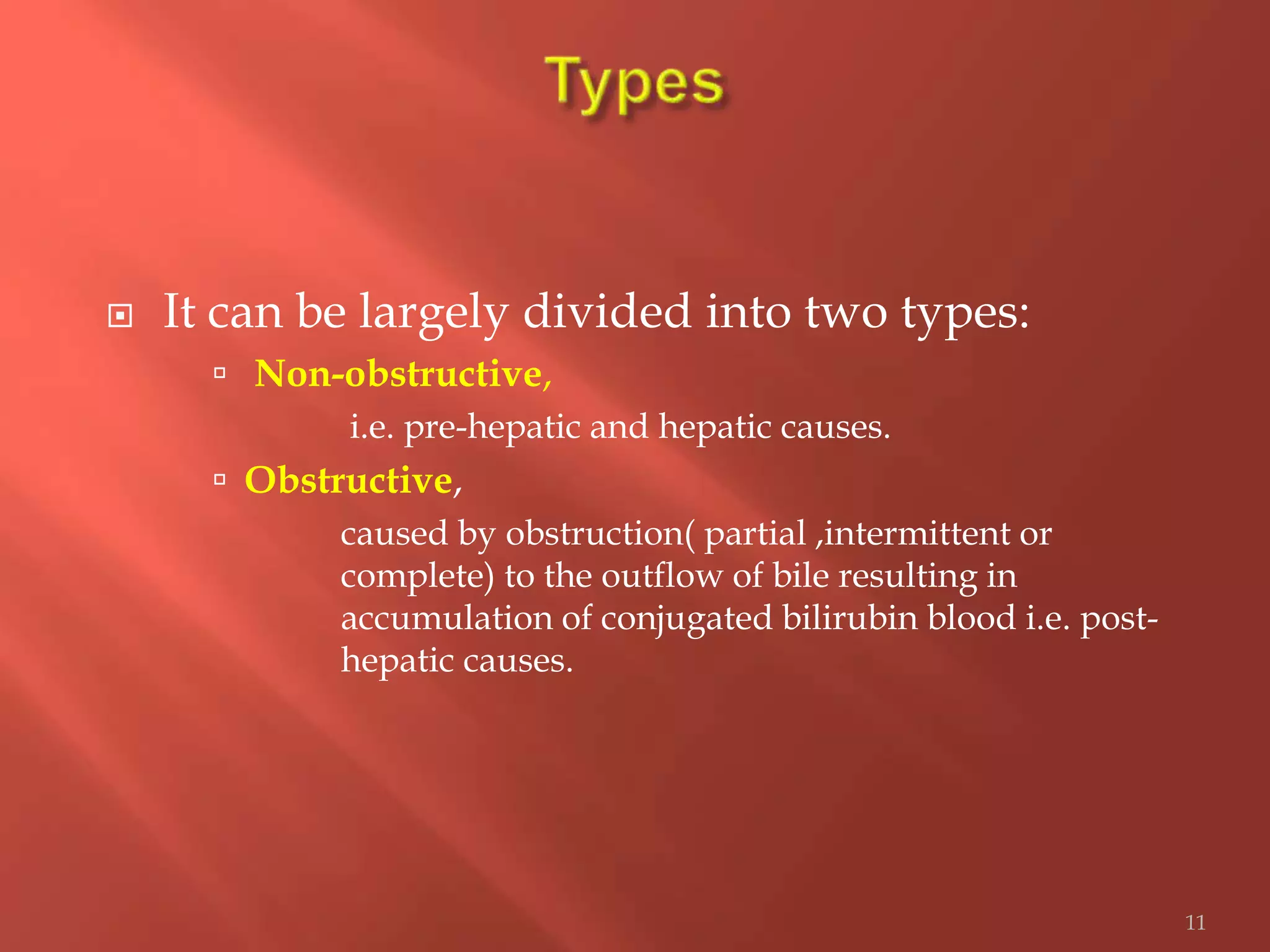
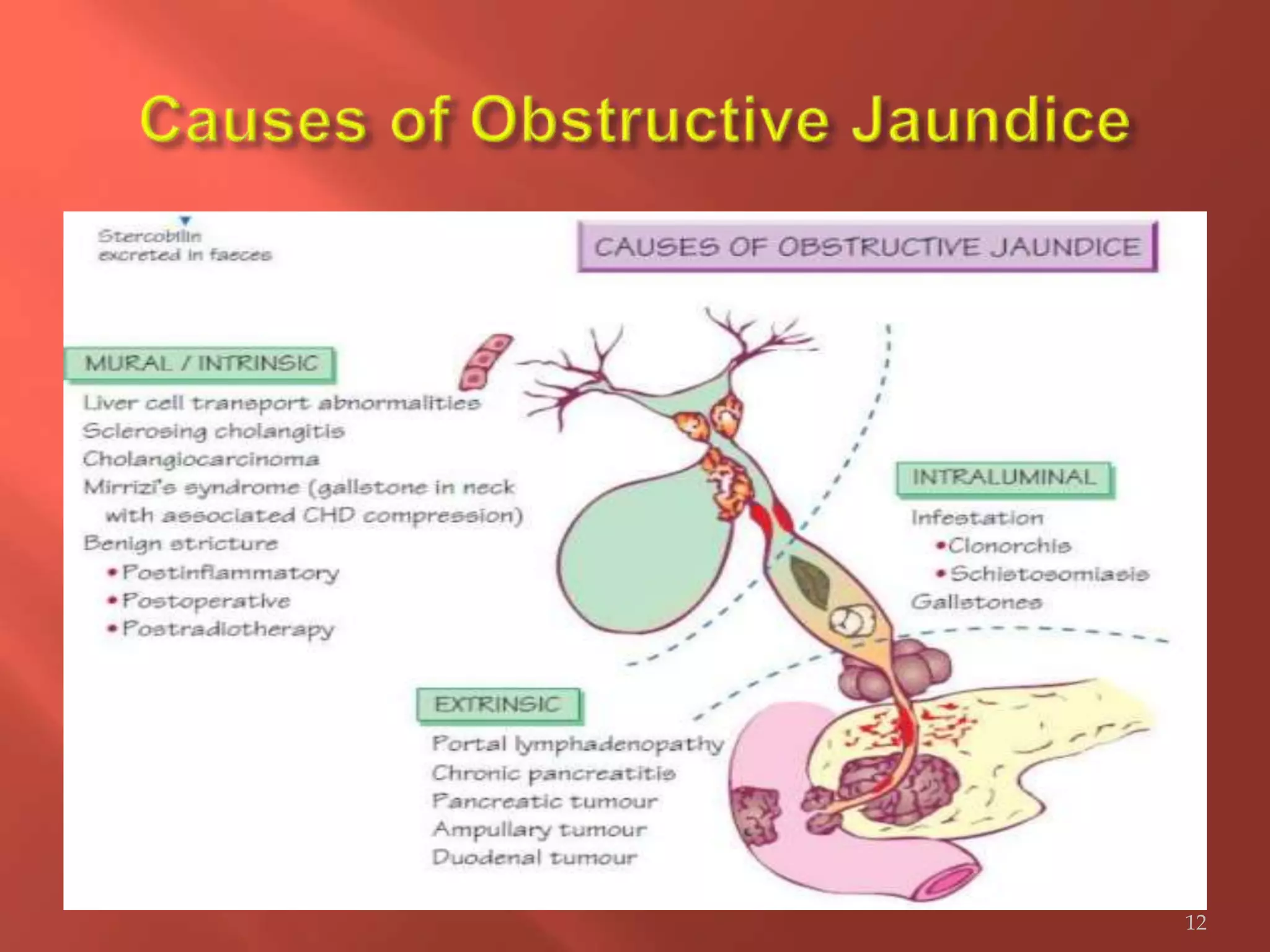
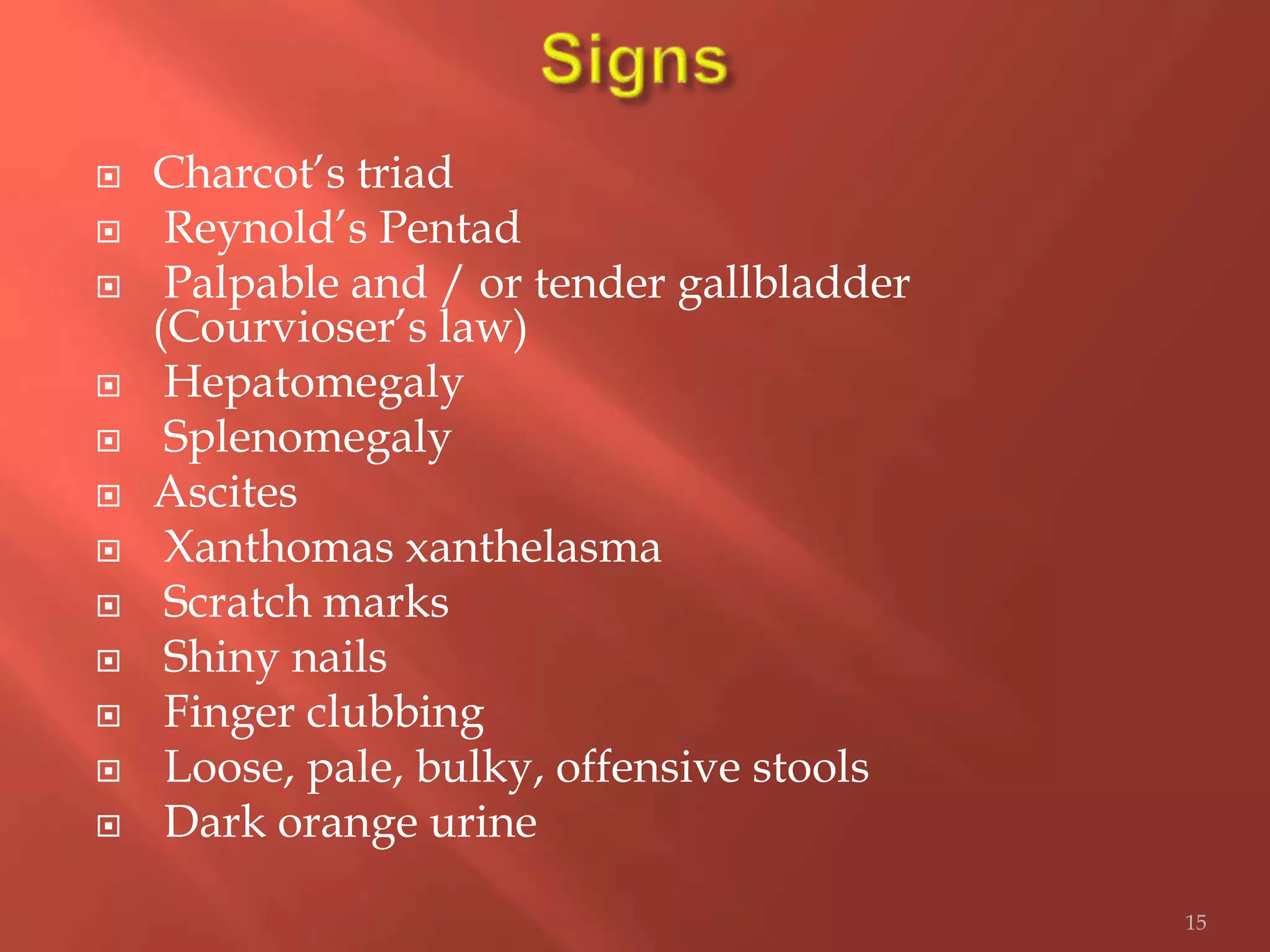
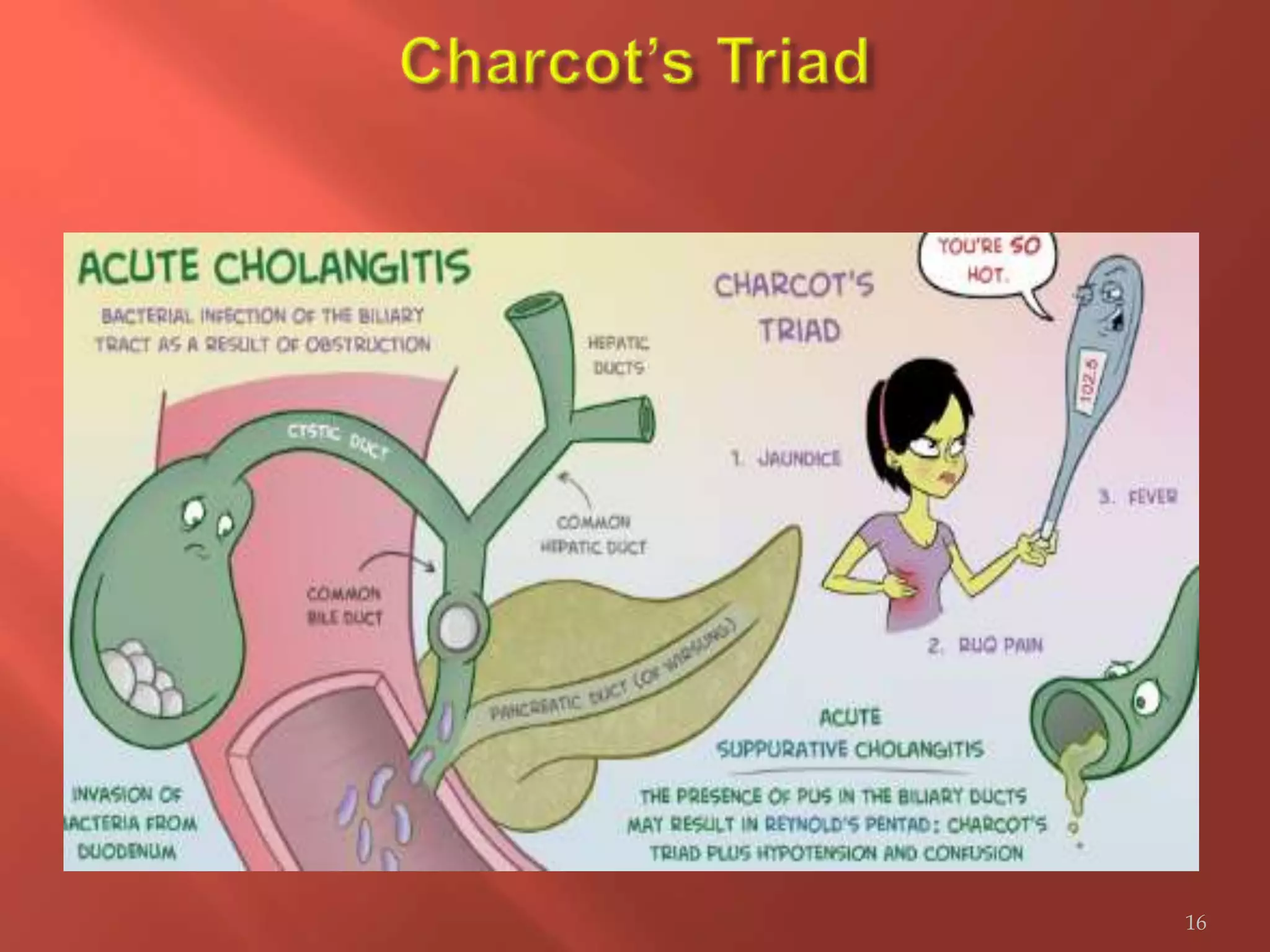
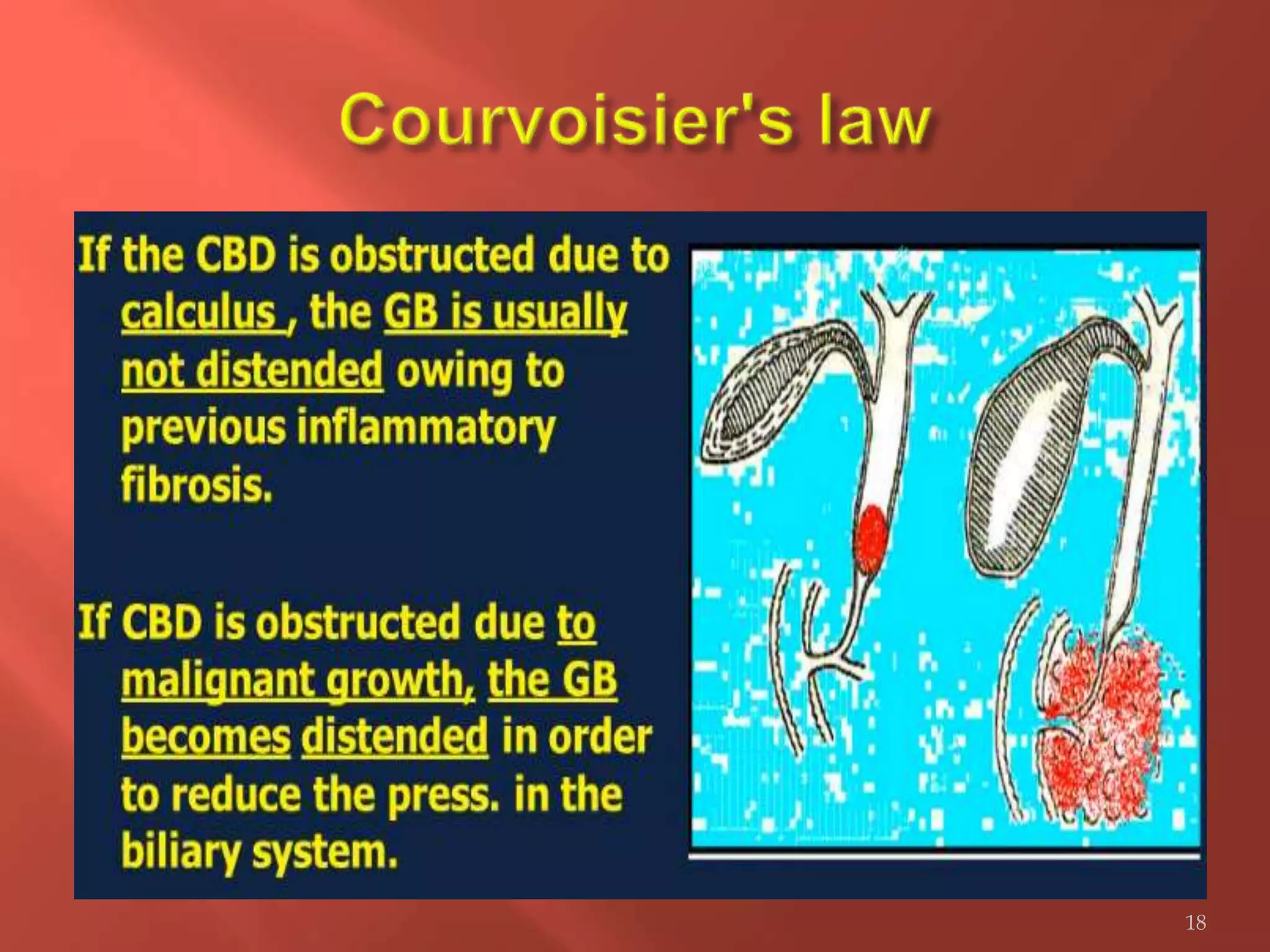
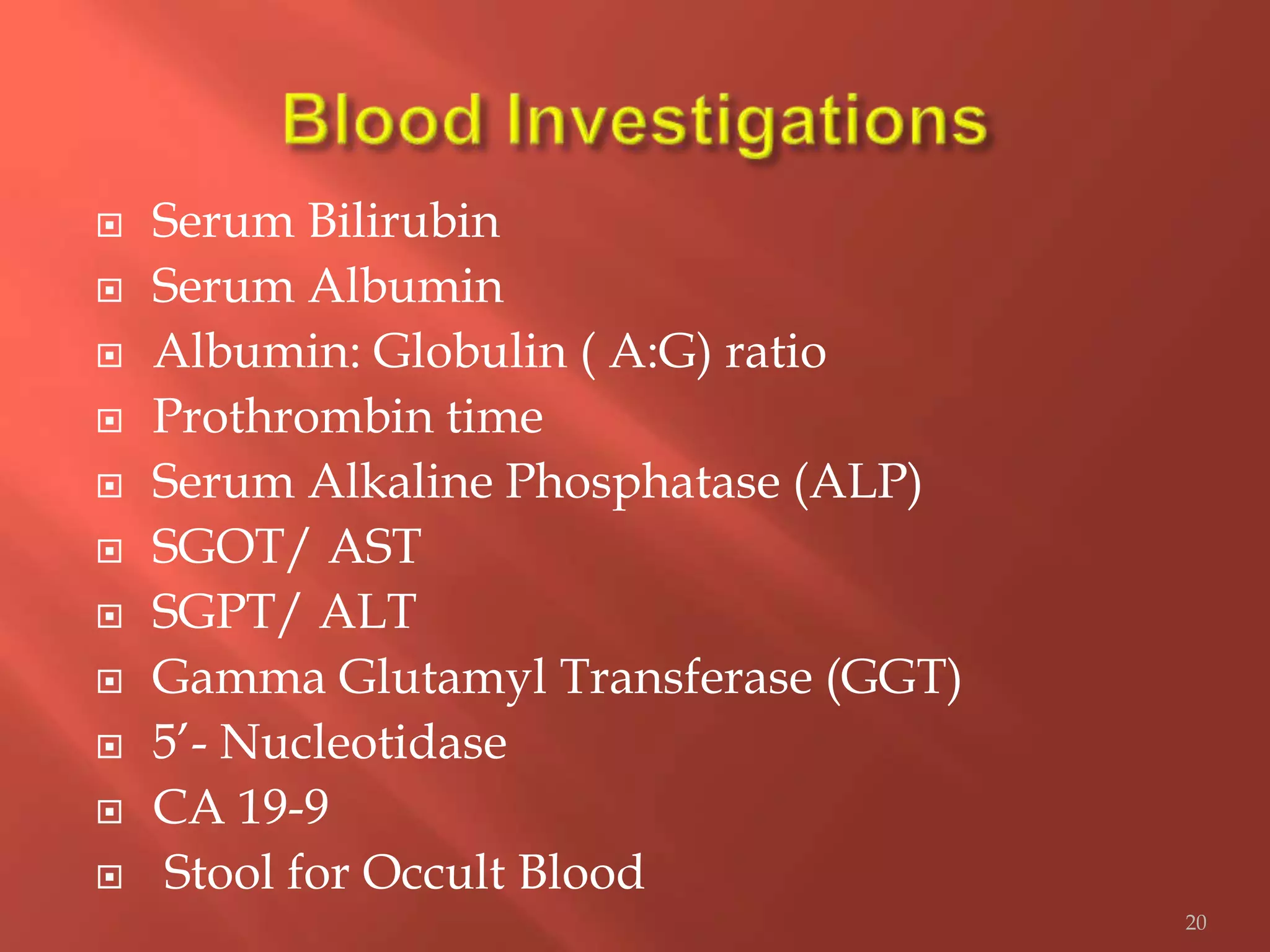
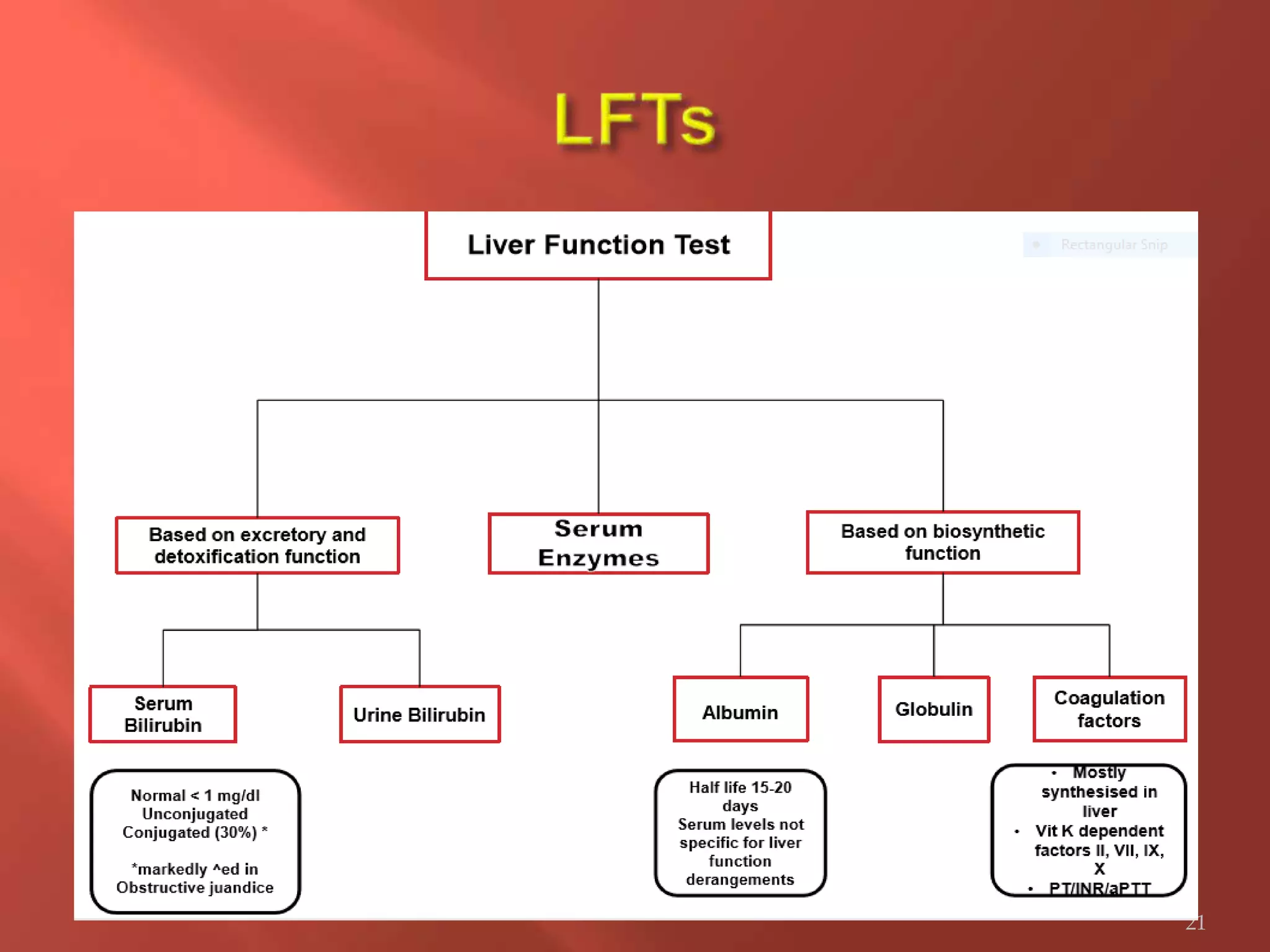
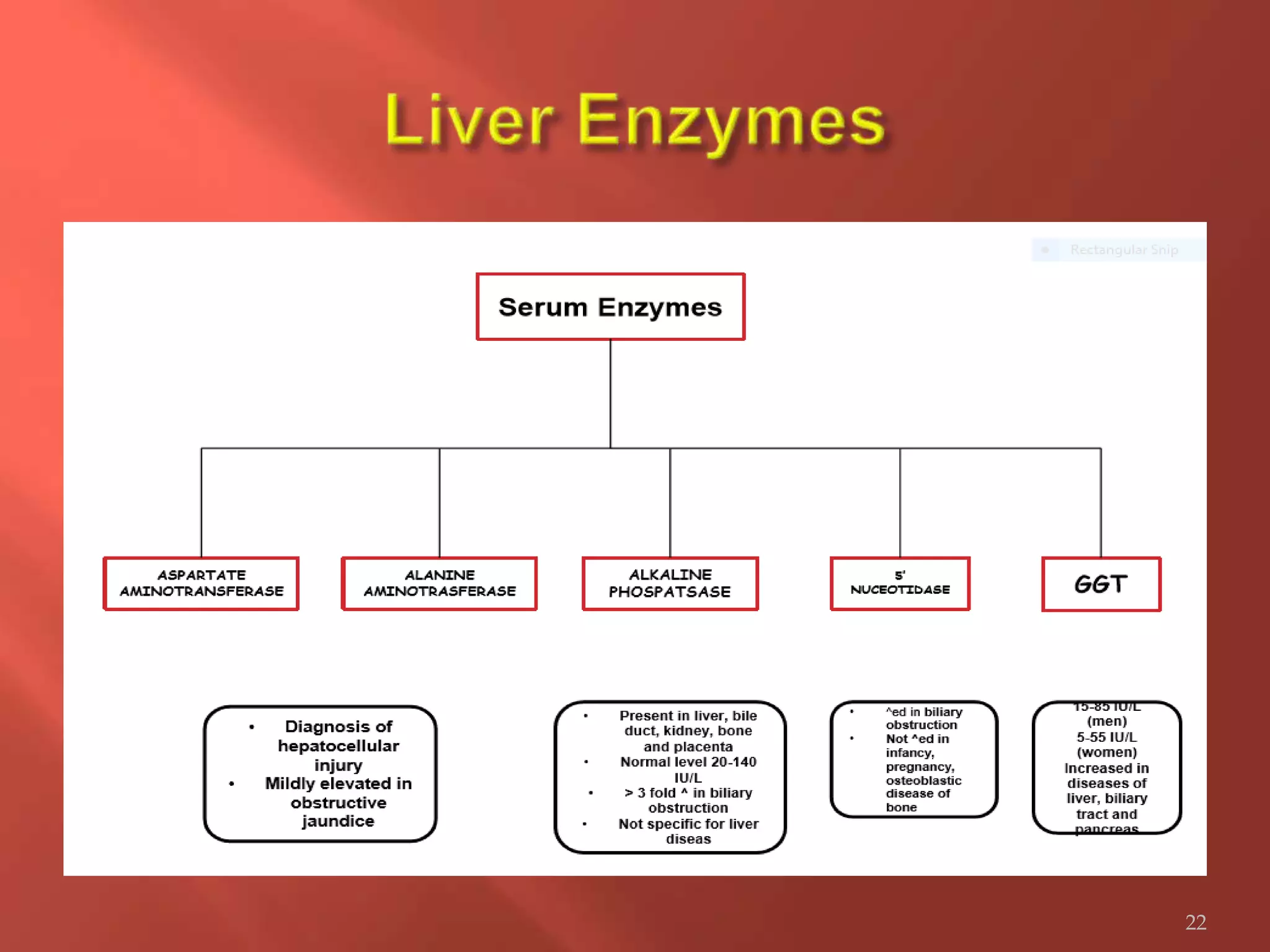
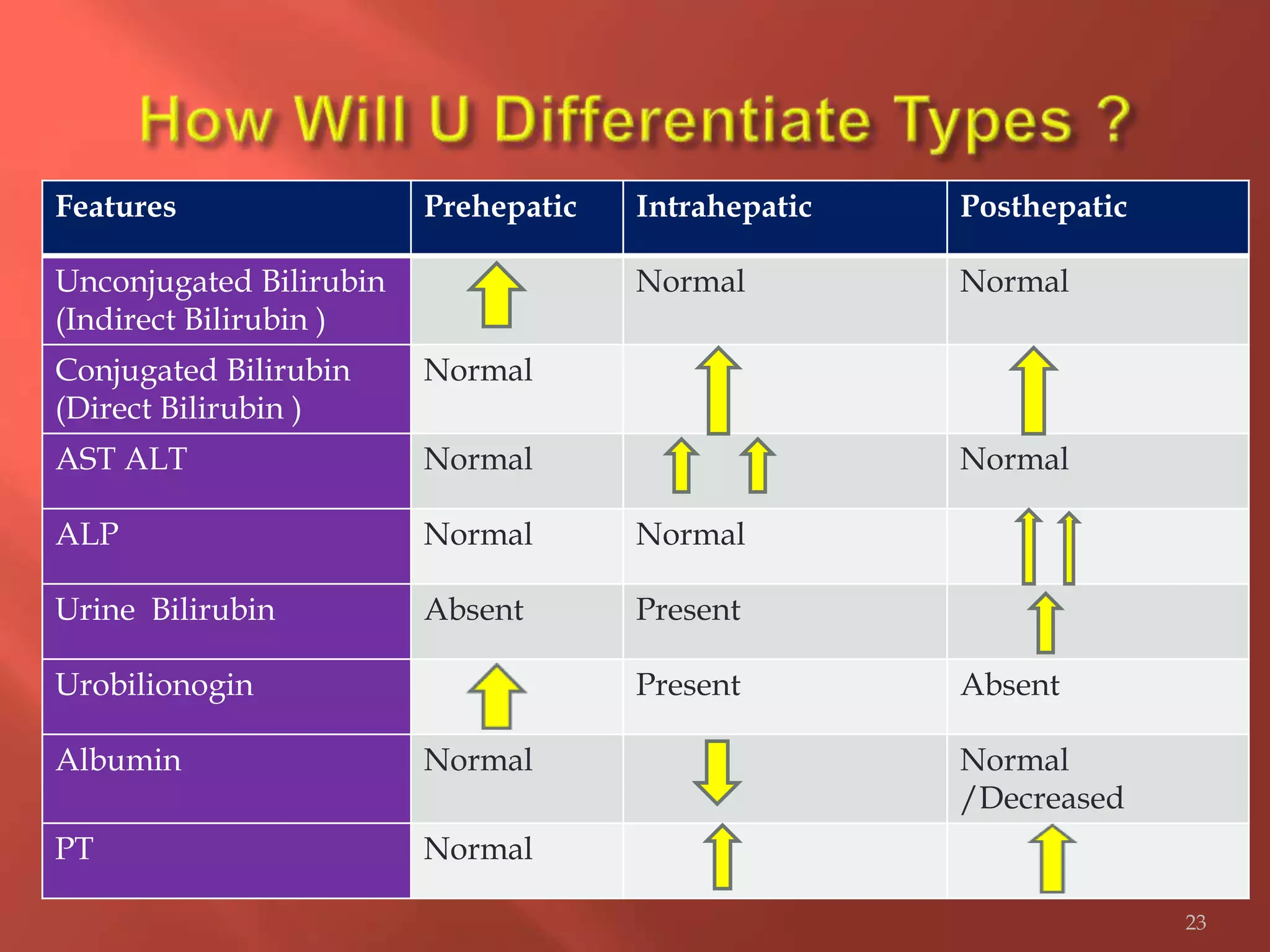
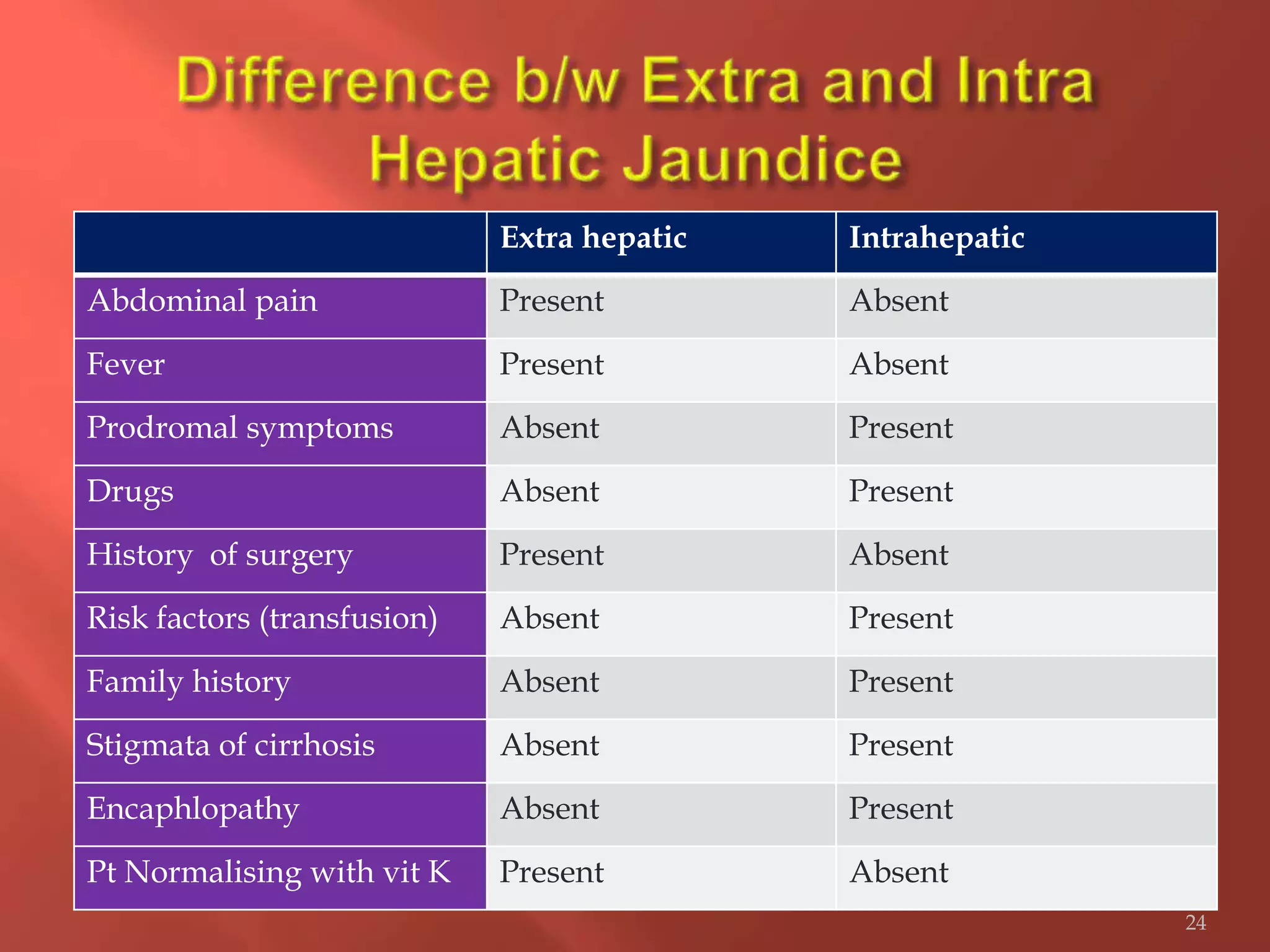
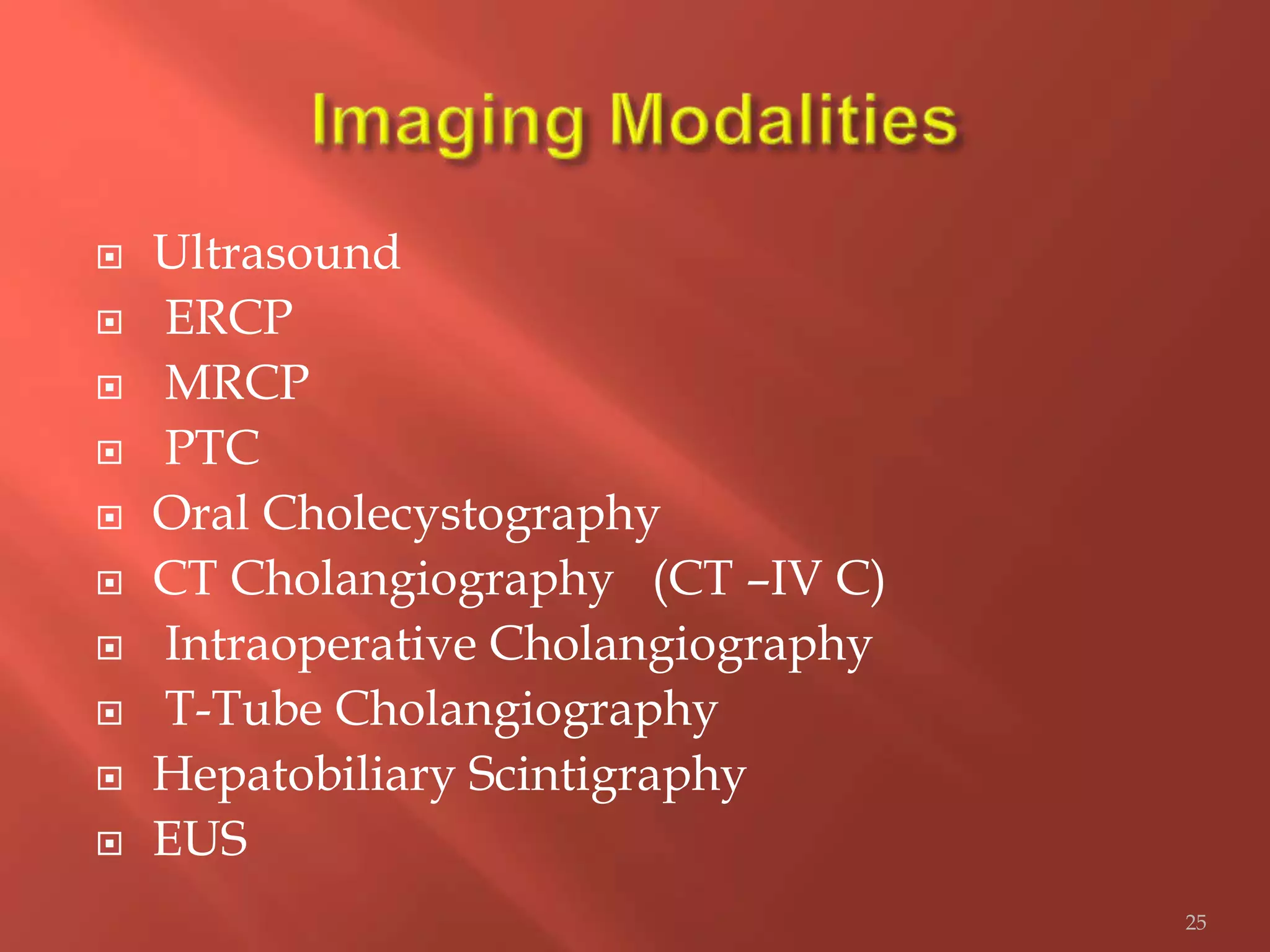
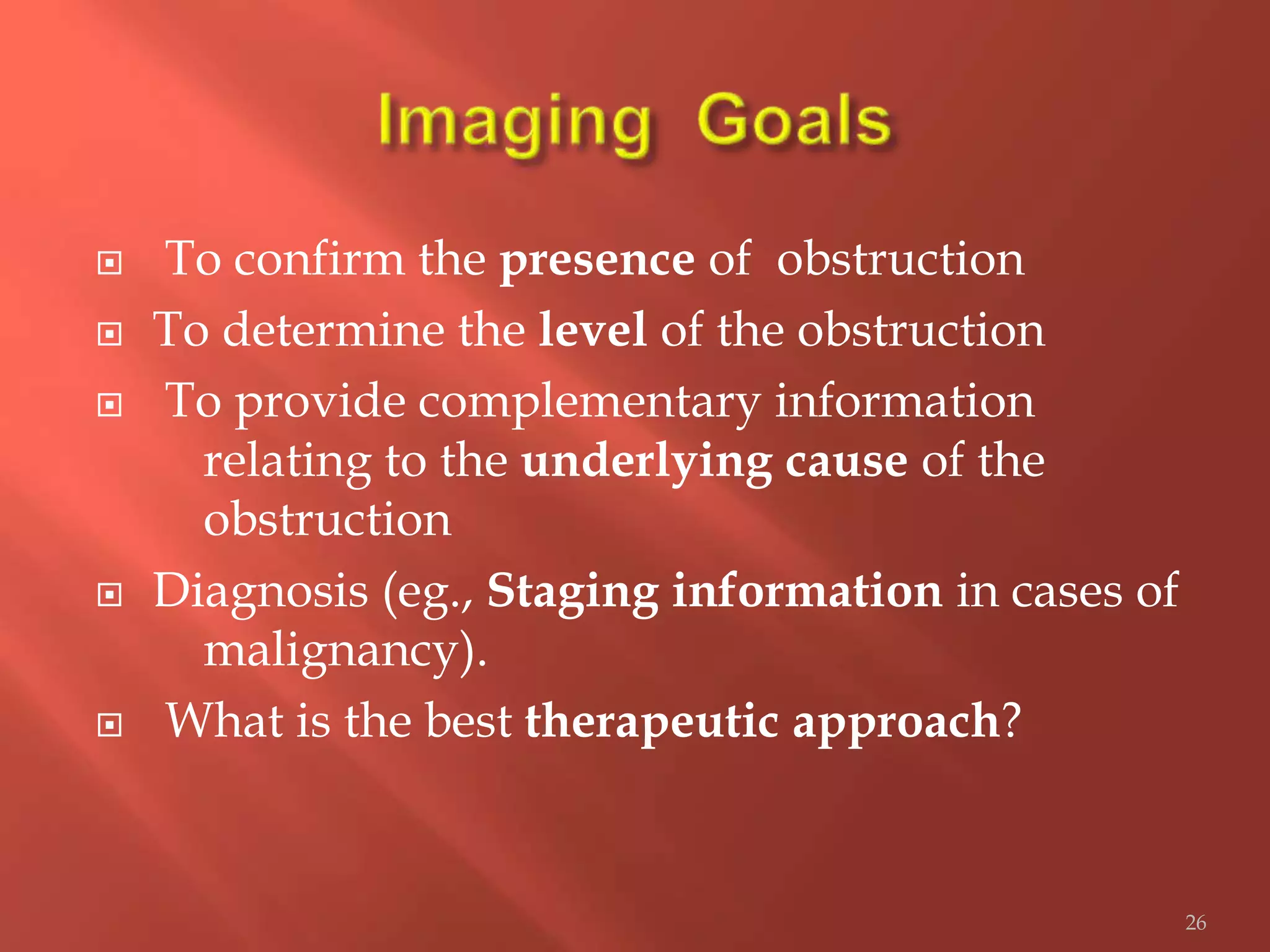
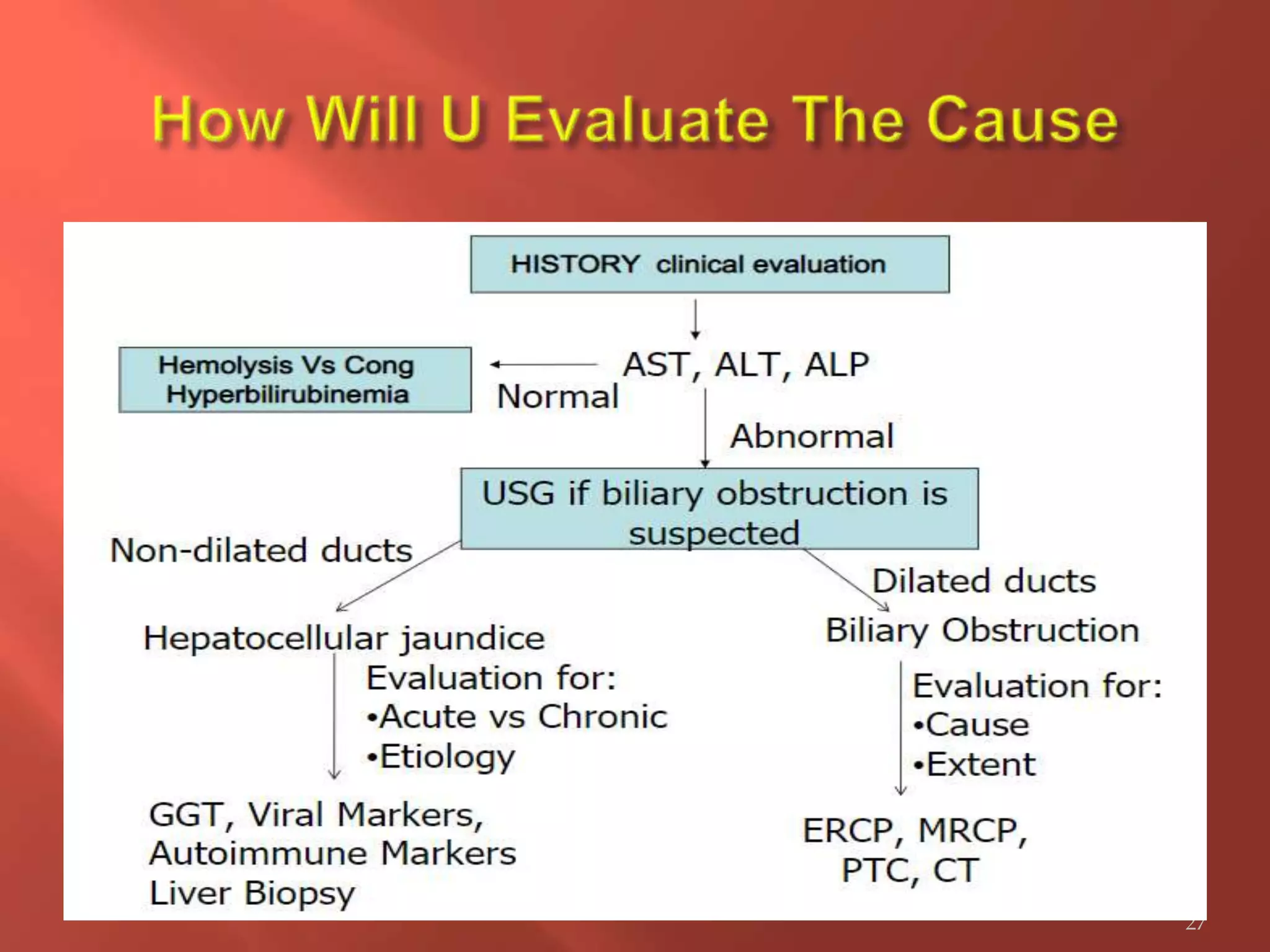
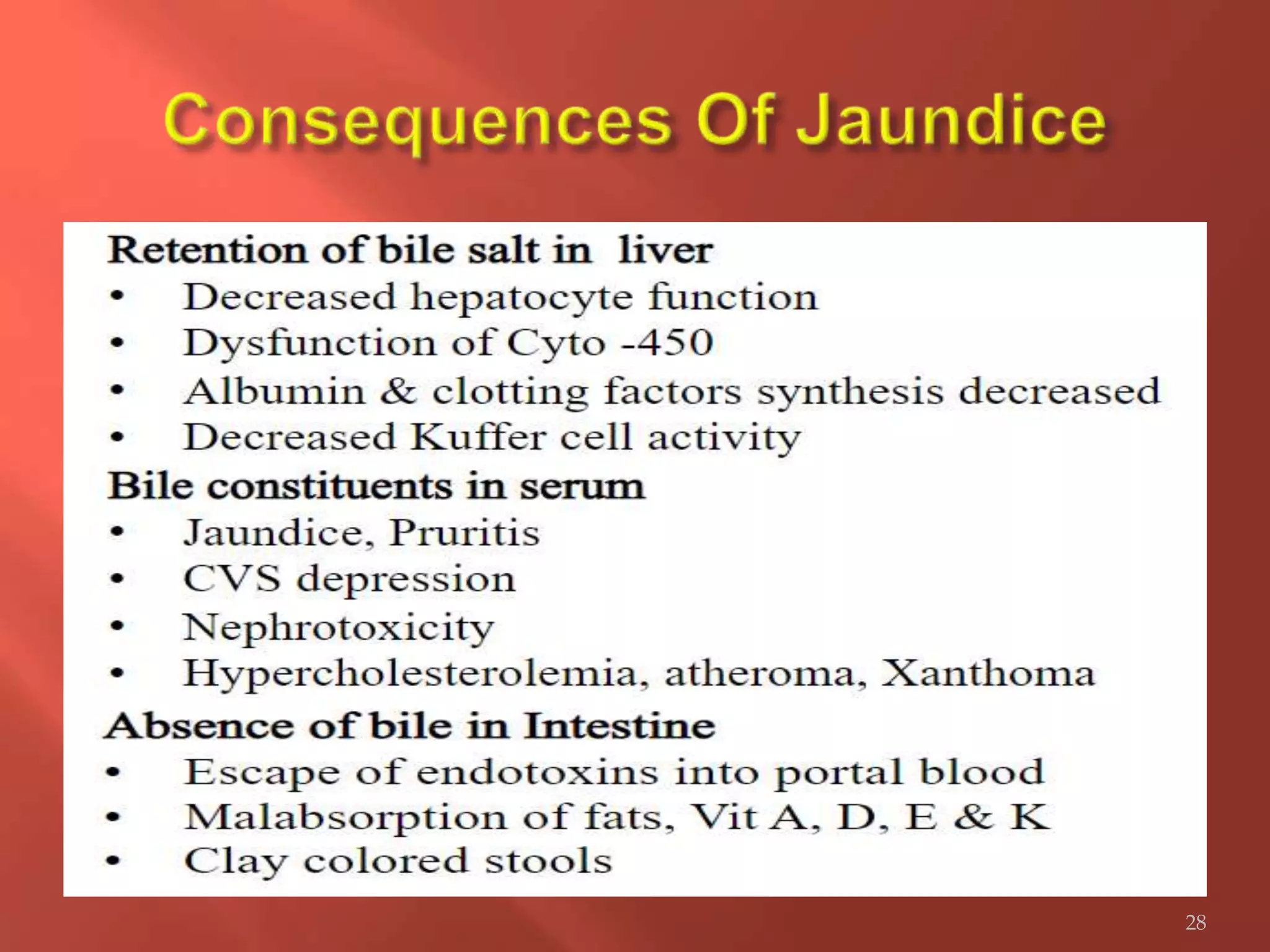
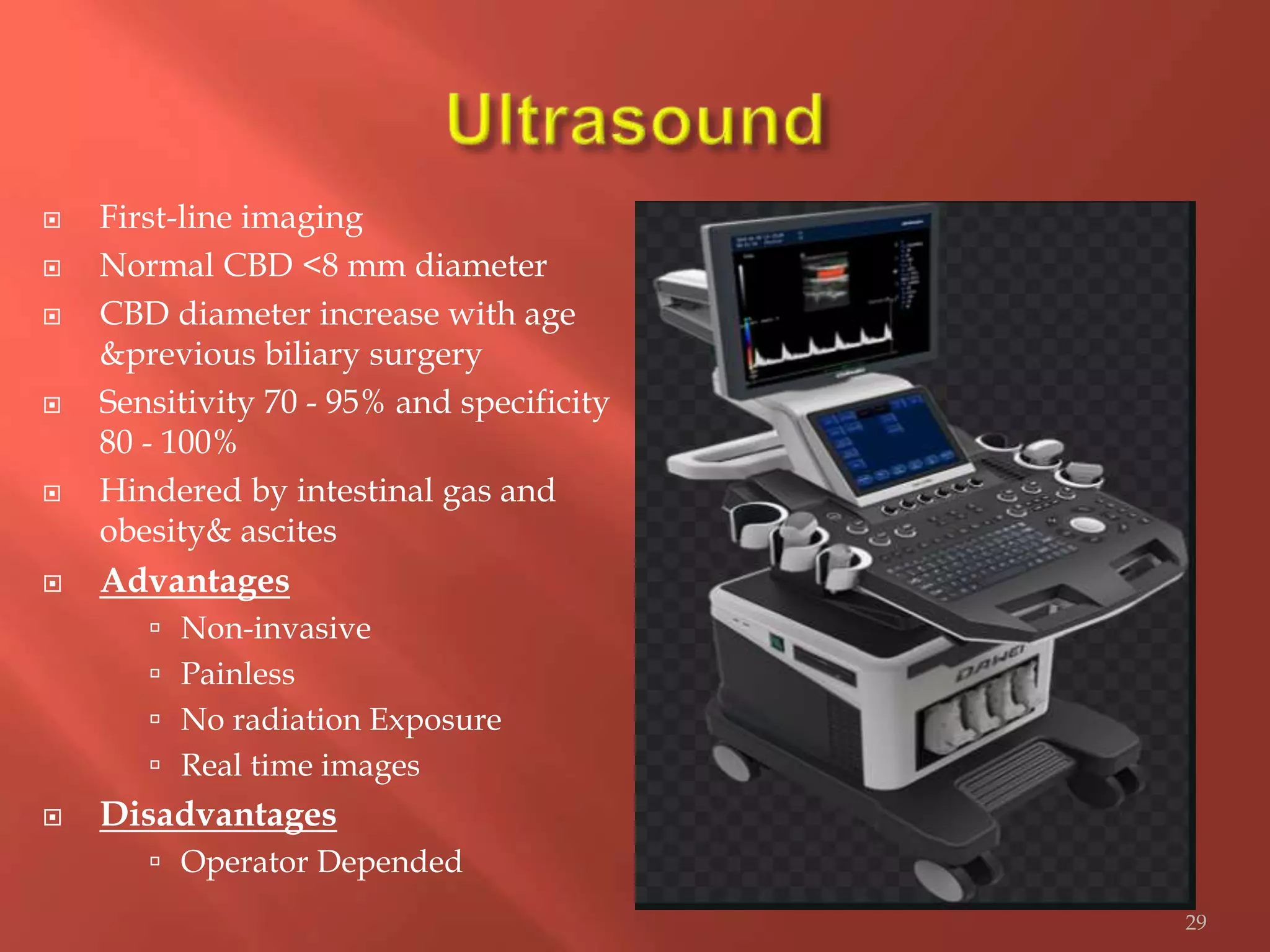
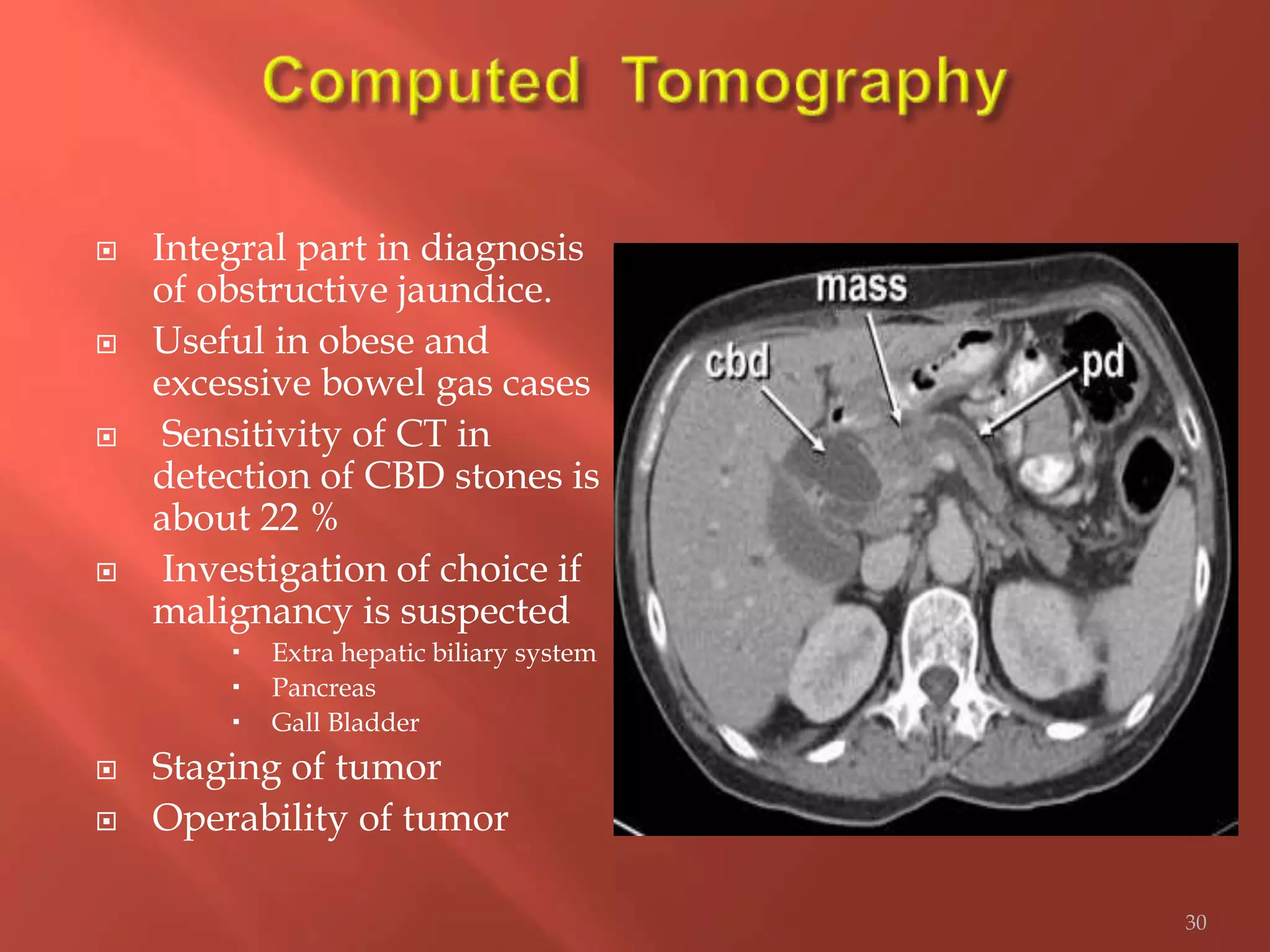
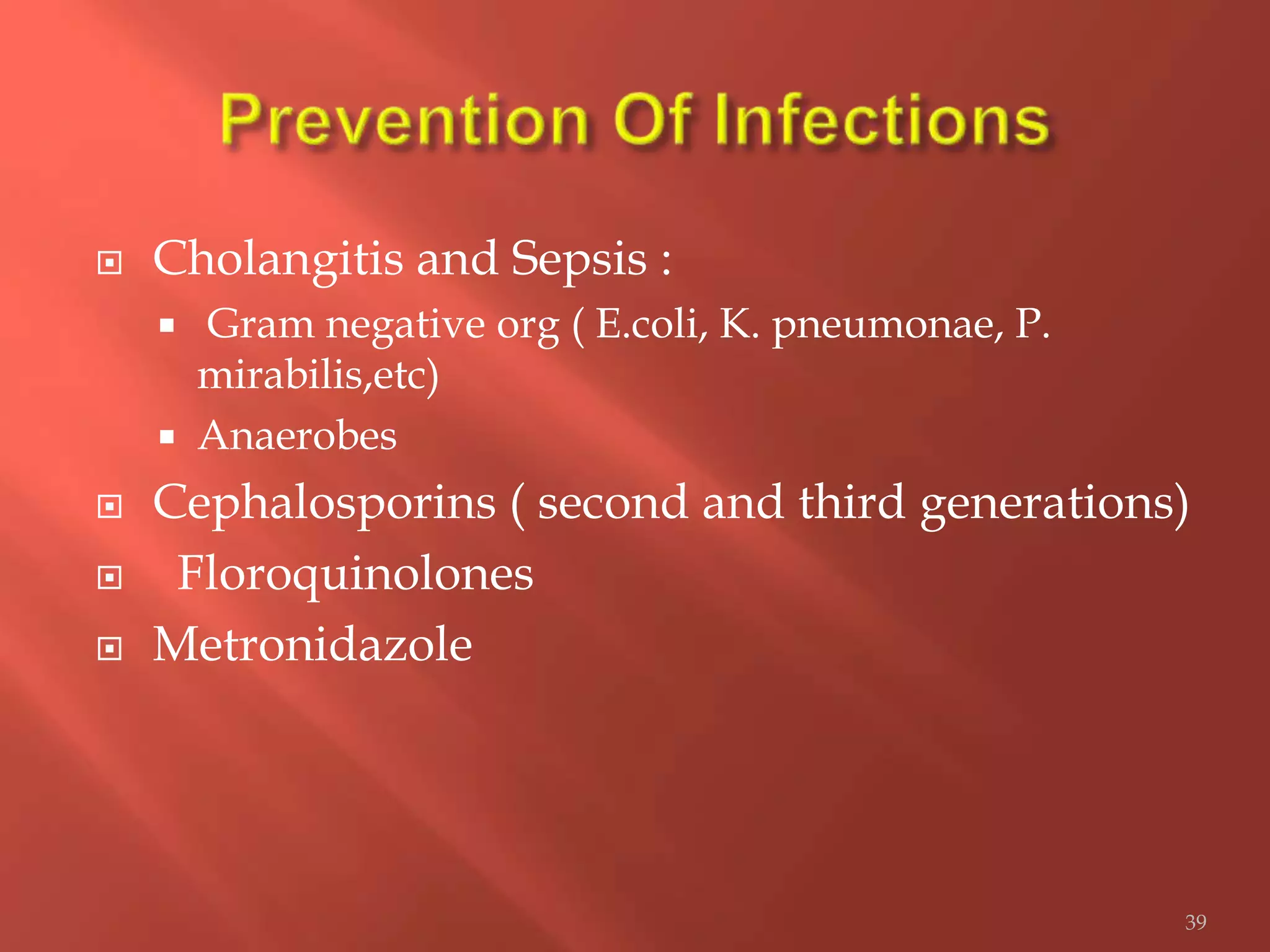
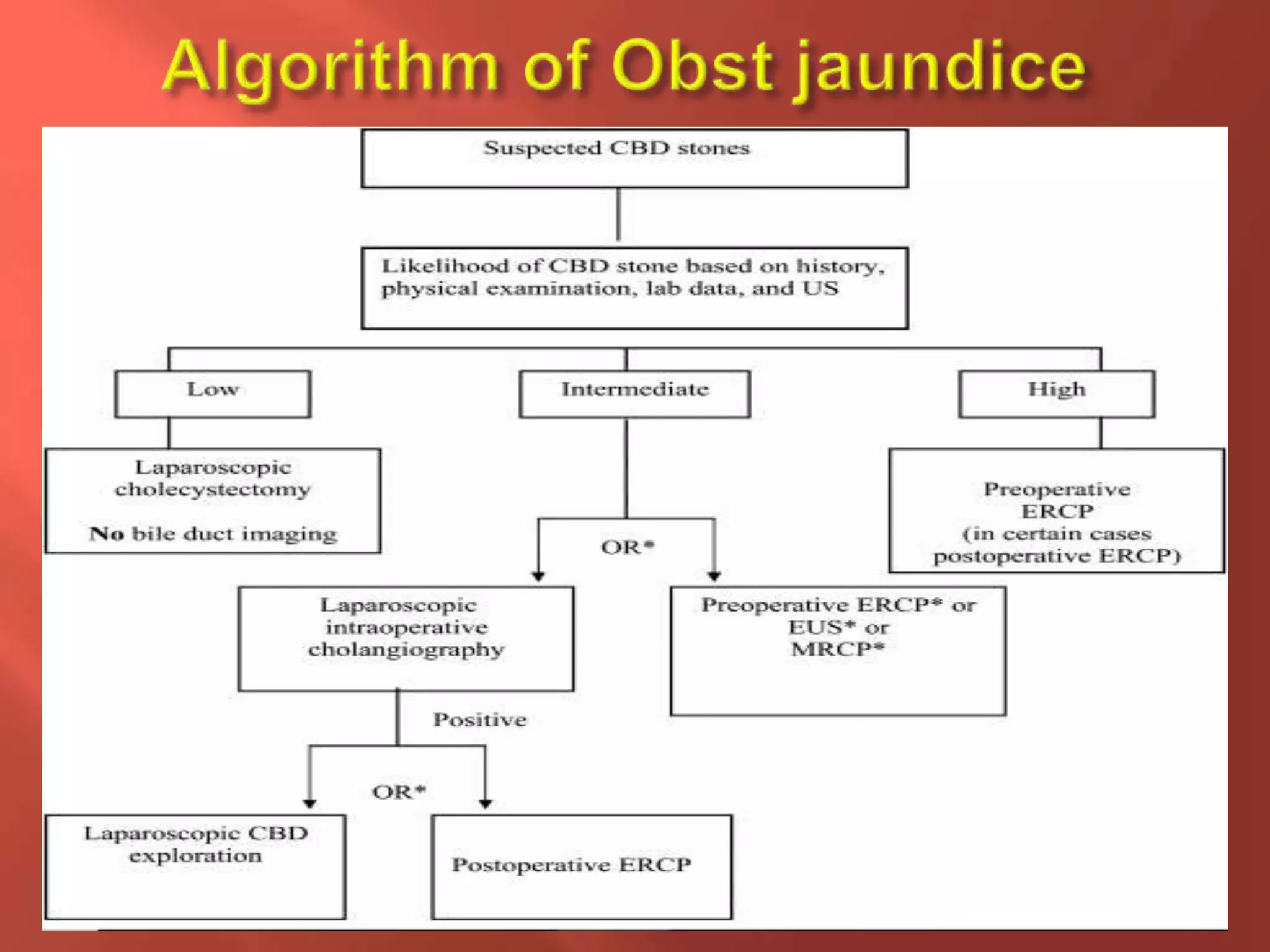
This document provides a case history, examination findings, investigations, and management plan for a 68-year-old male presenting with jaundice, abdominal pain, and itching for 20 days. Examination found jaundice, hepatomegaly, and abdominal tenderness. Liver function tests showed elevated bilirubin and alkaline phosphatase. Ultrasound and CT scan identified a mass in the periampullary region. The patient was diagnosed with obstructive jaundice likely due to a periampullary tumor and treated with antibiotics and pain medication.