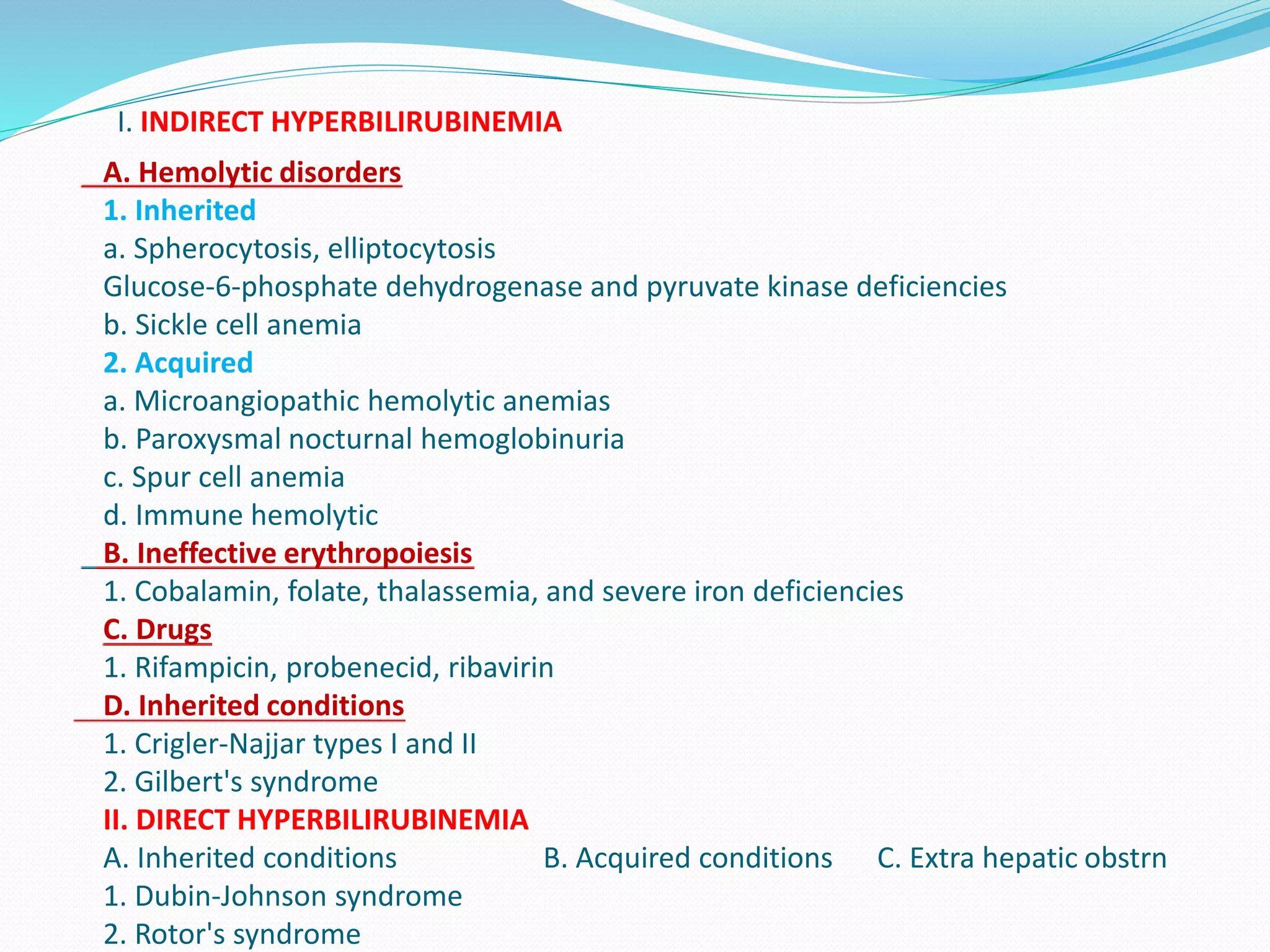
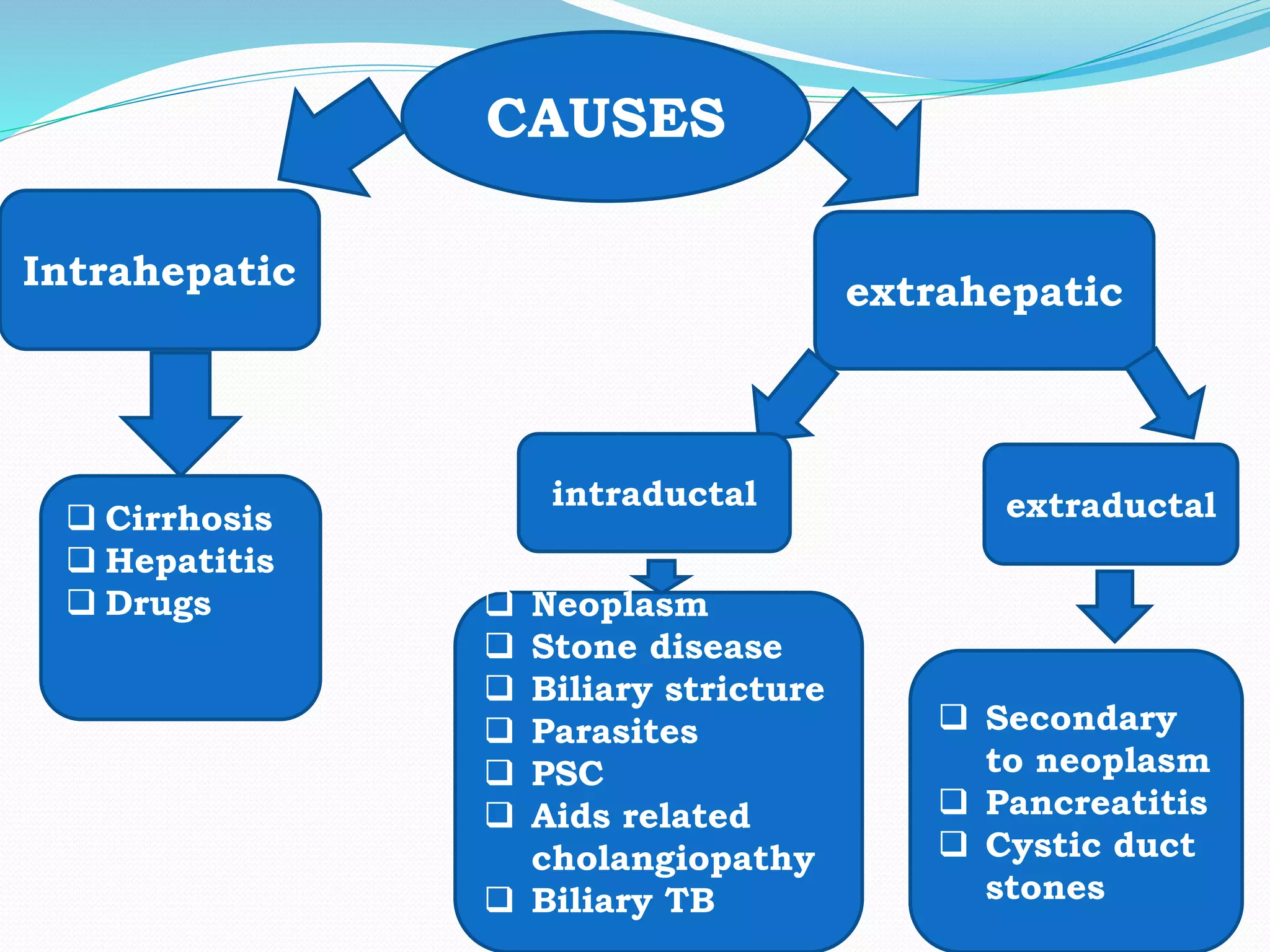
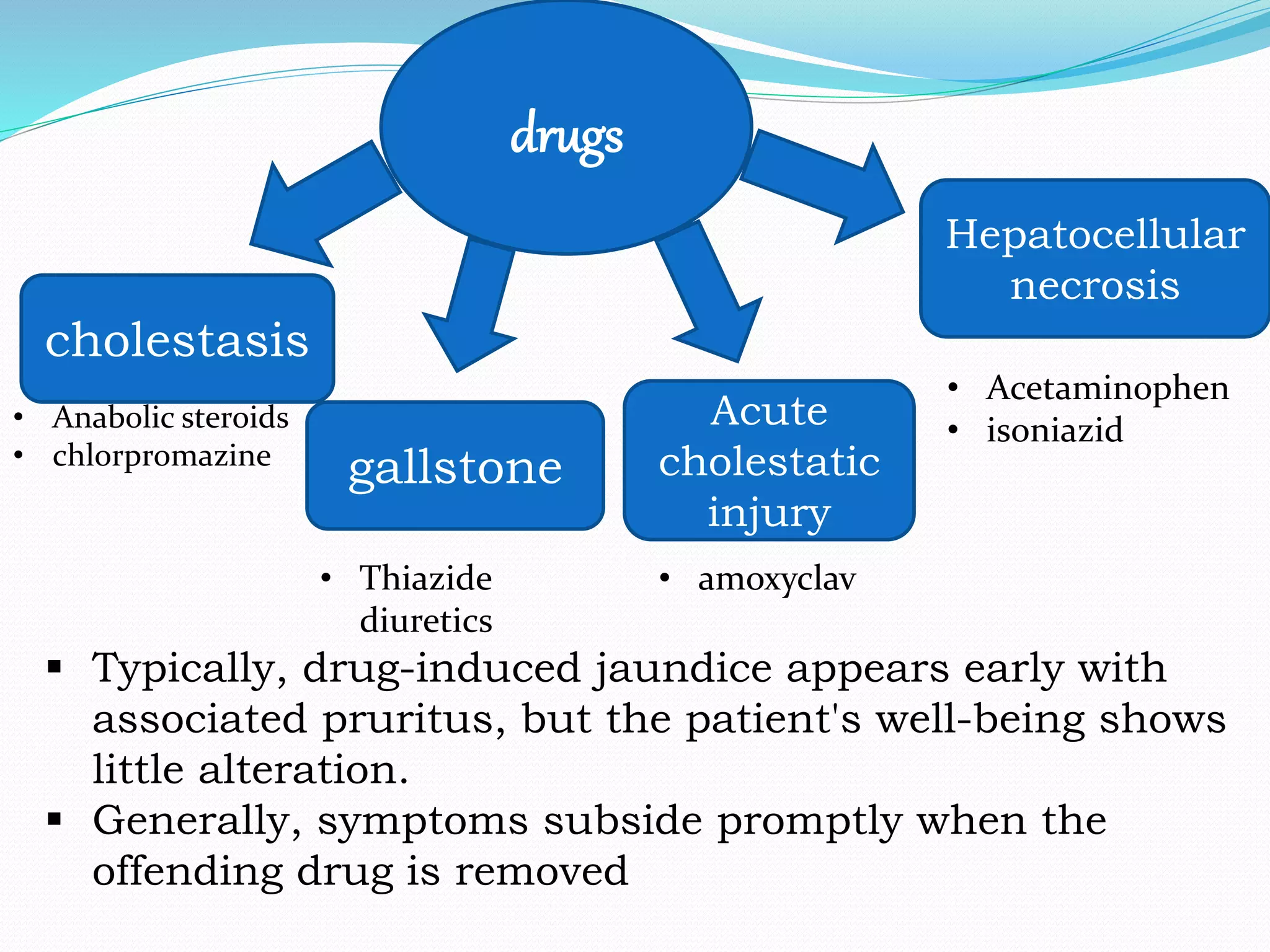
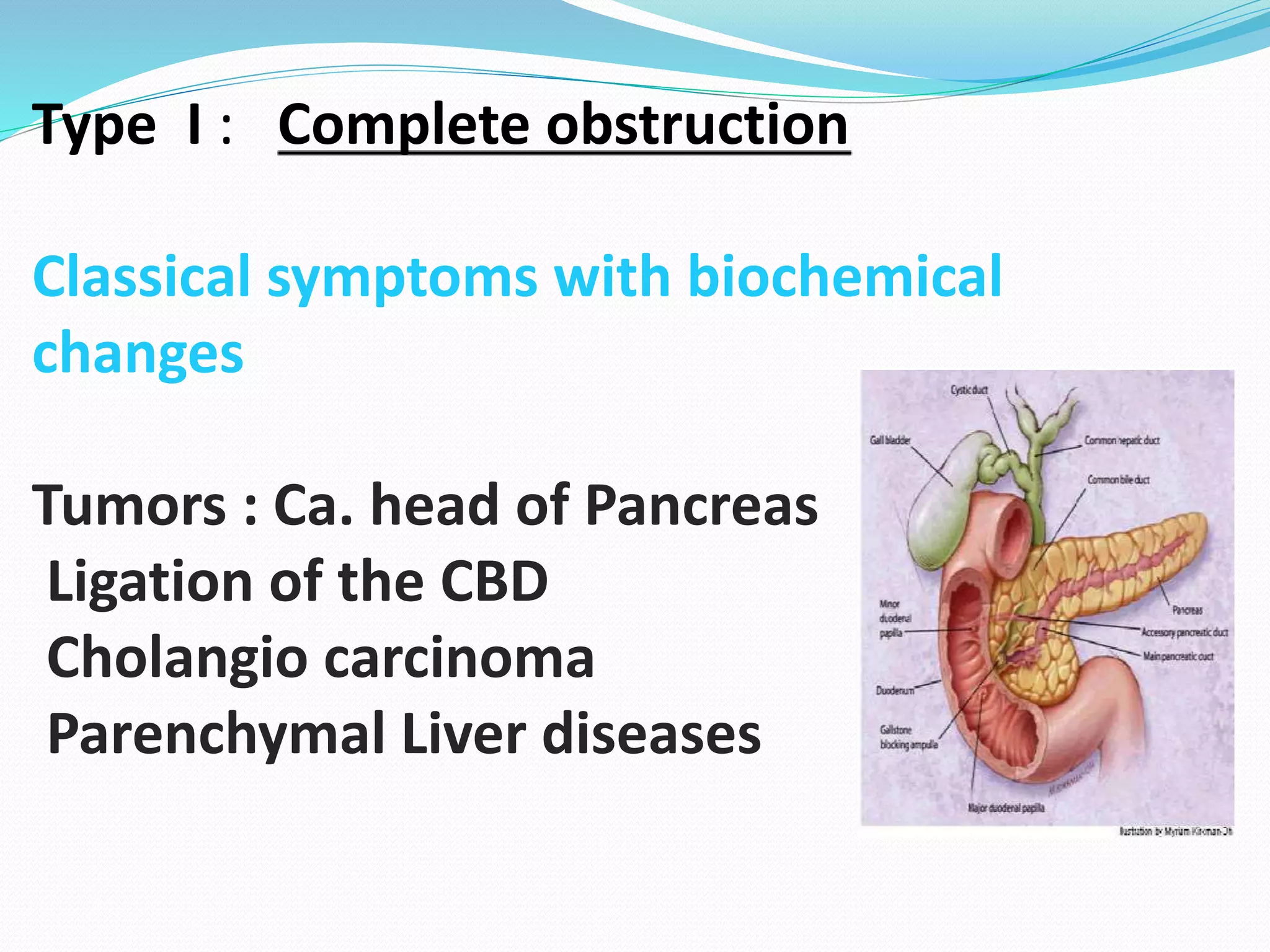
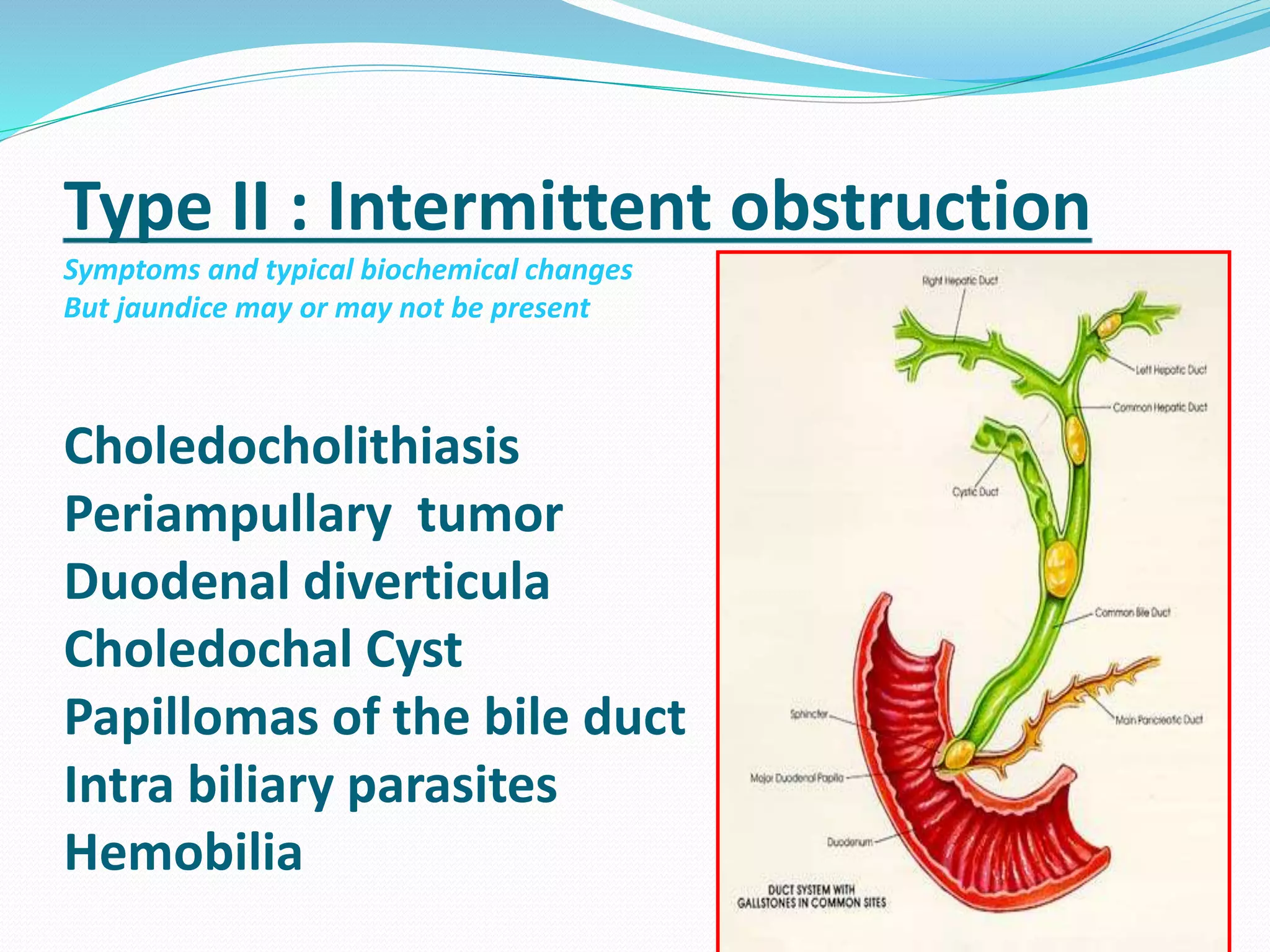
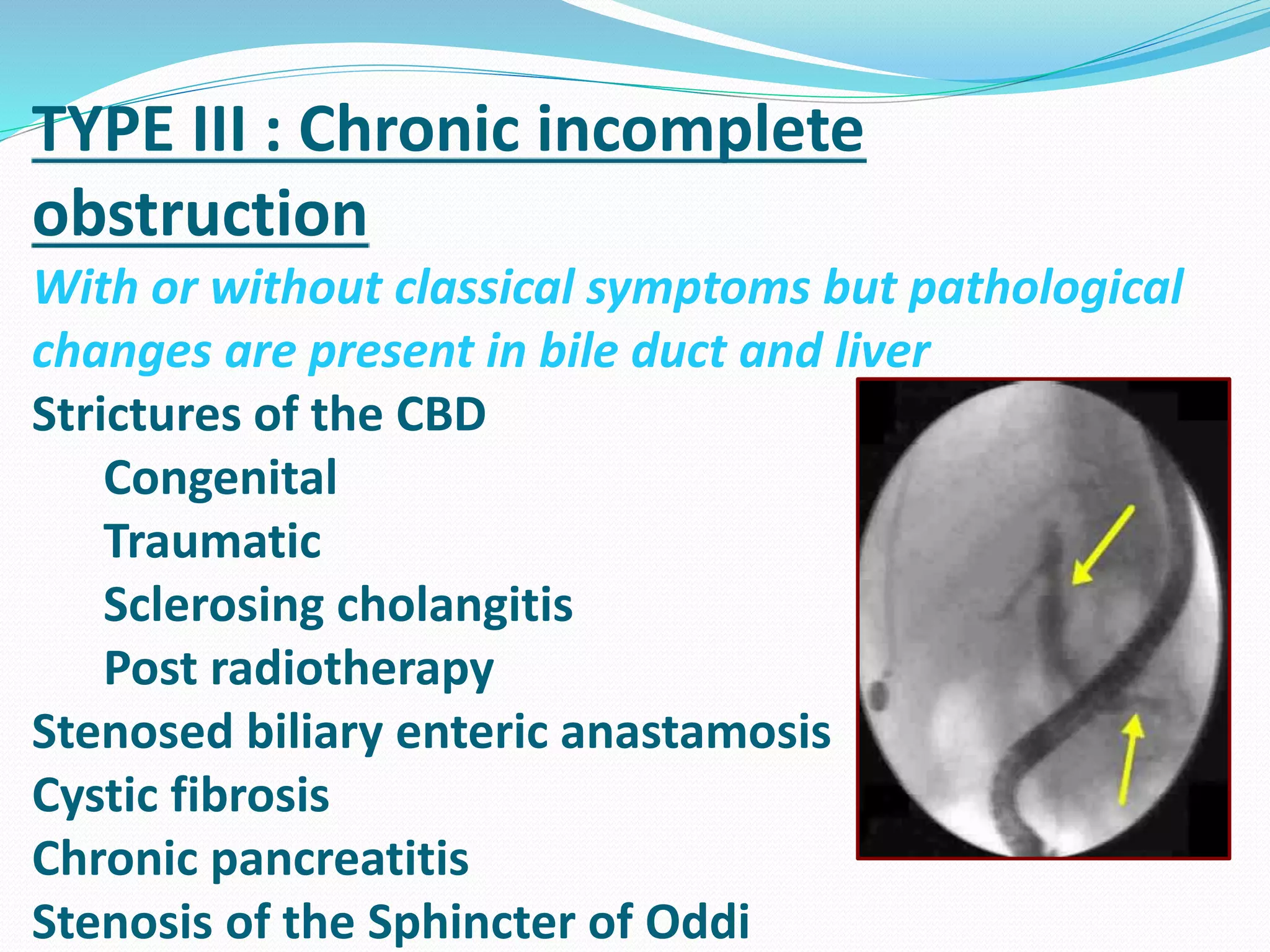
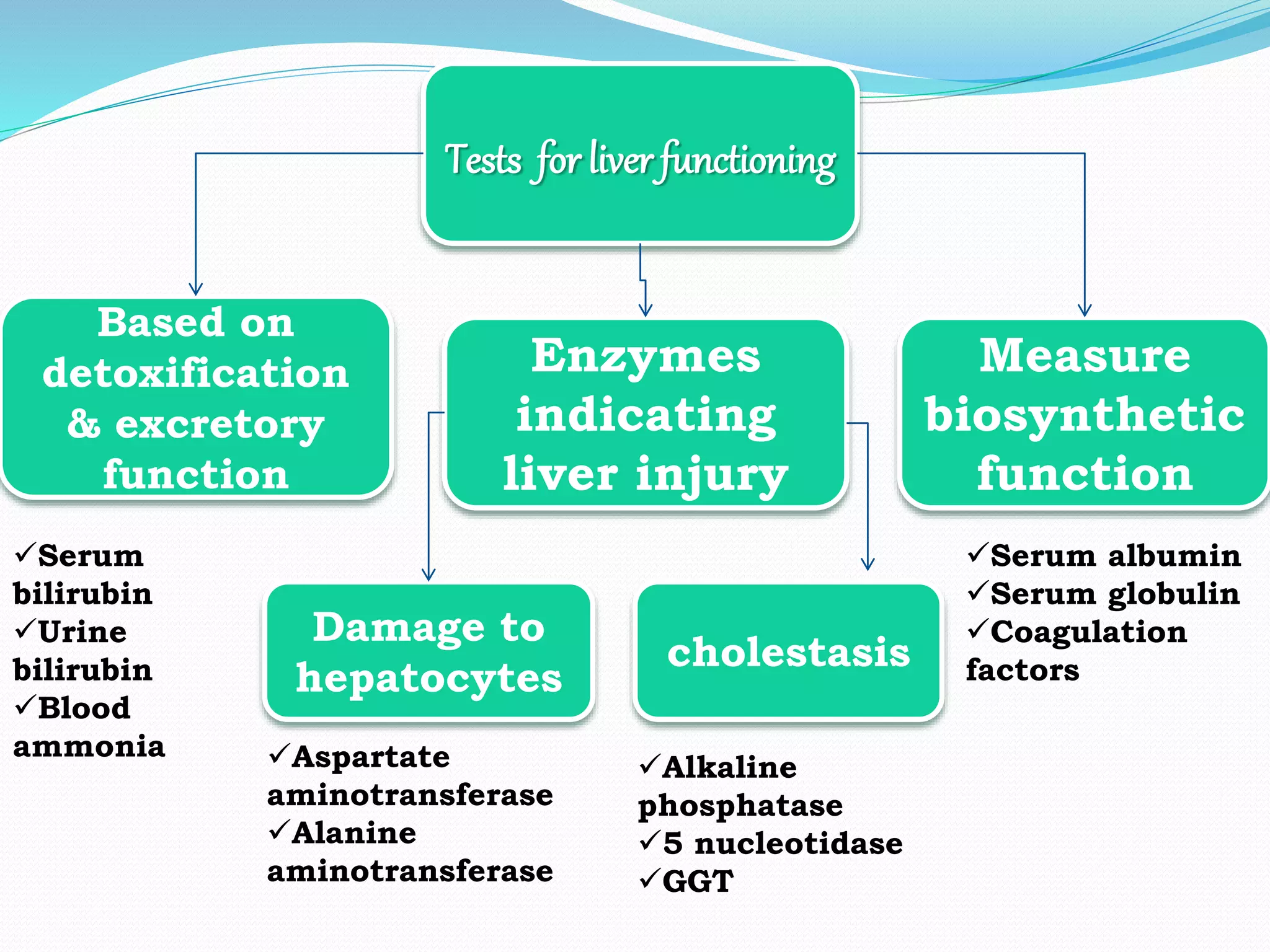
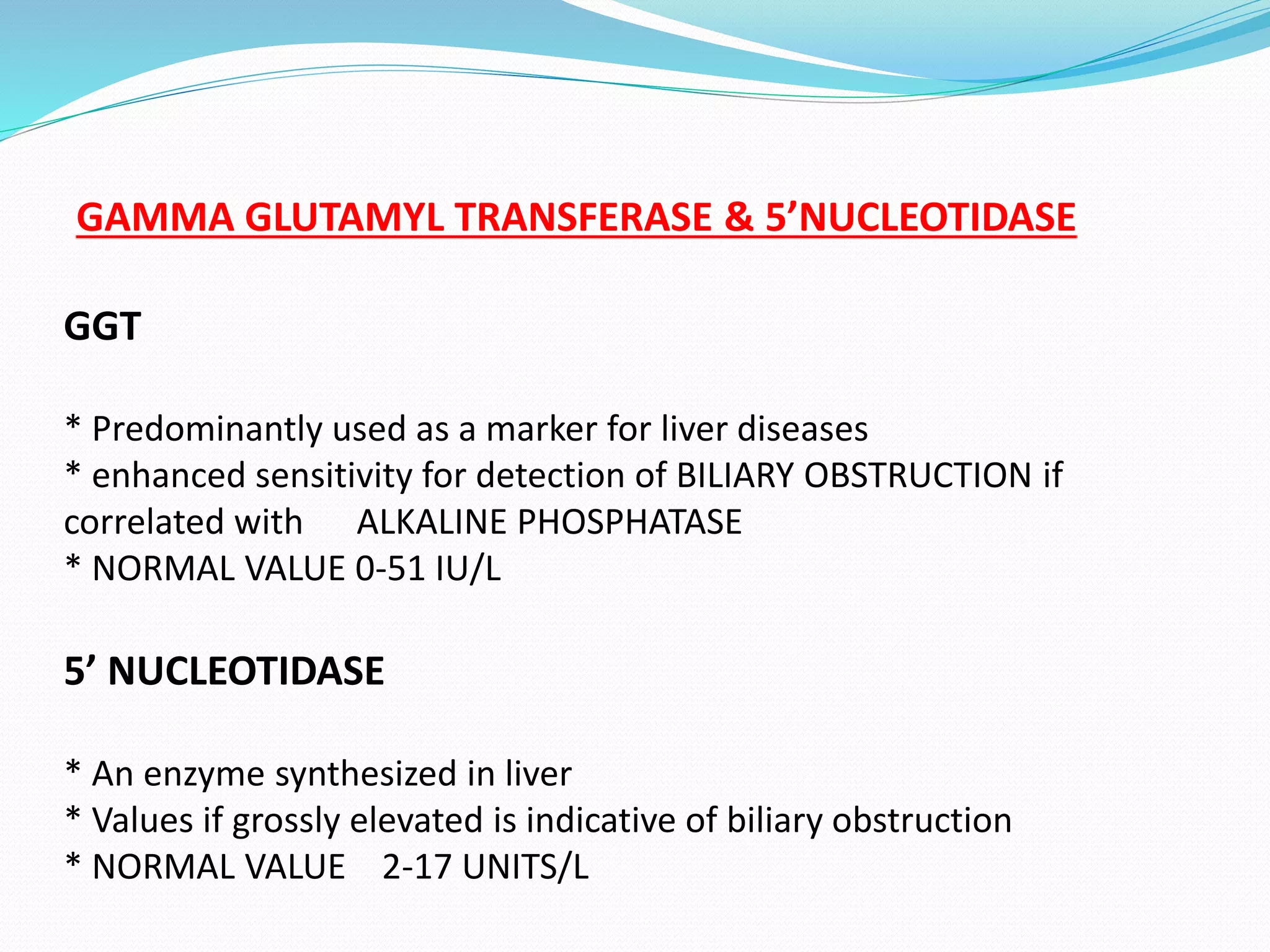
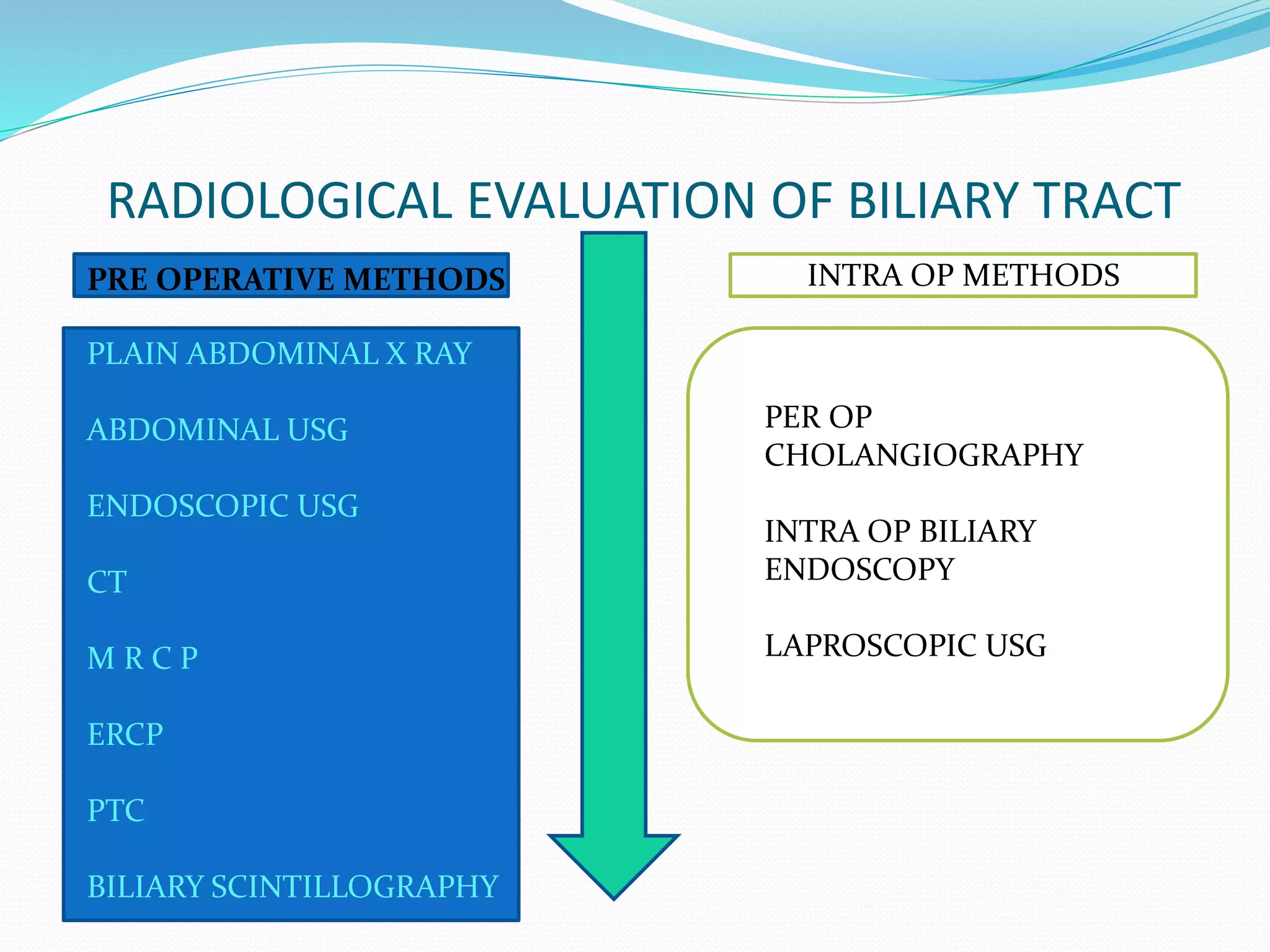
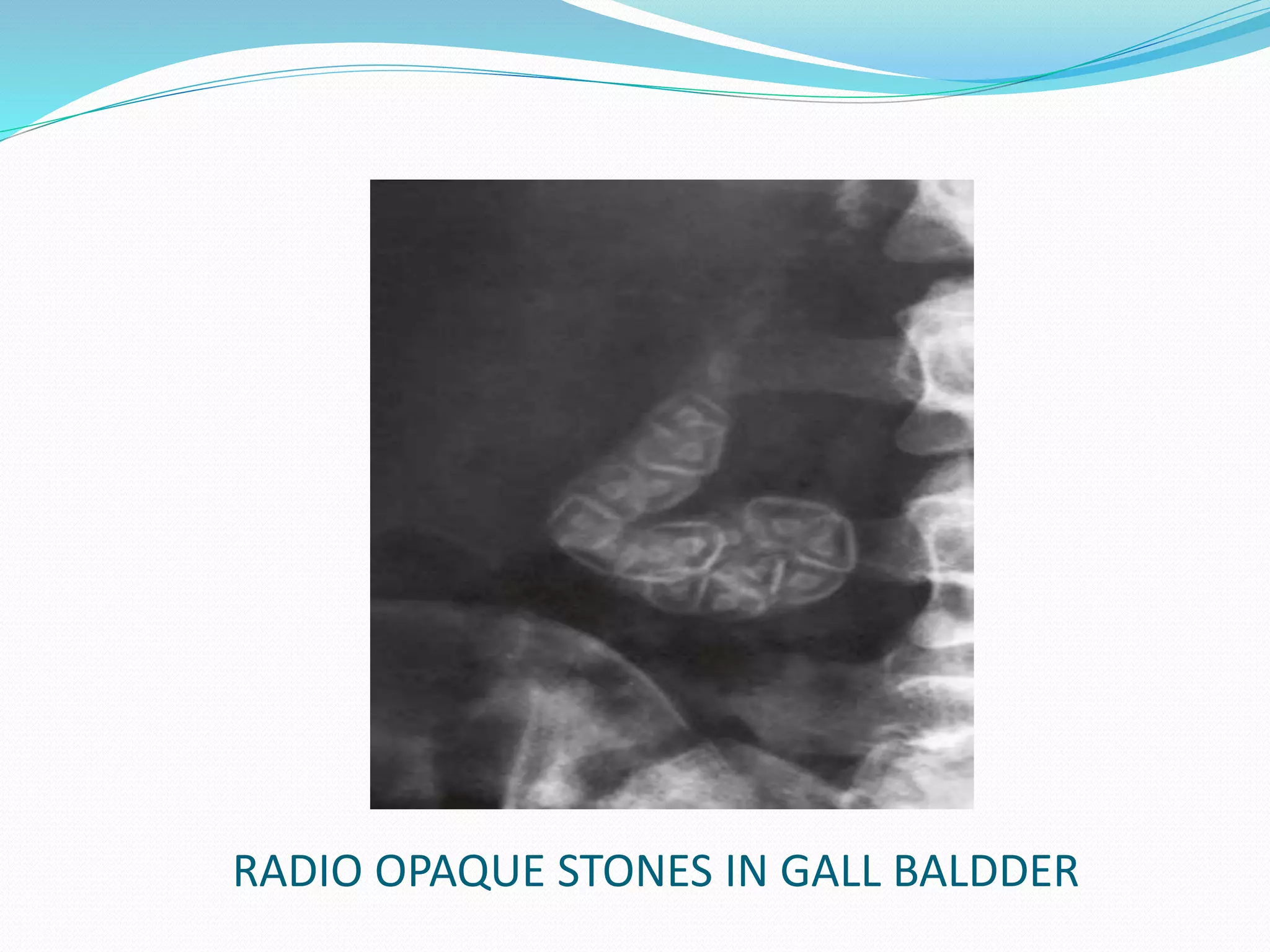
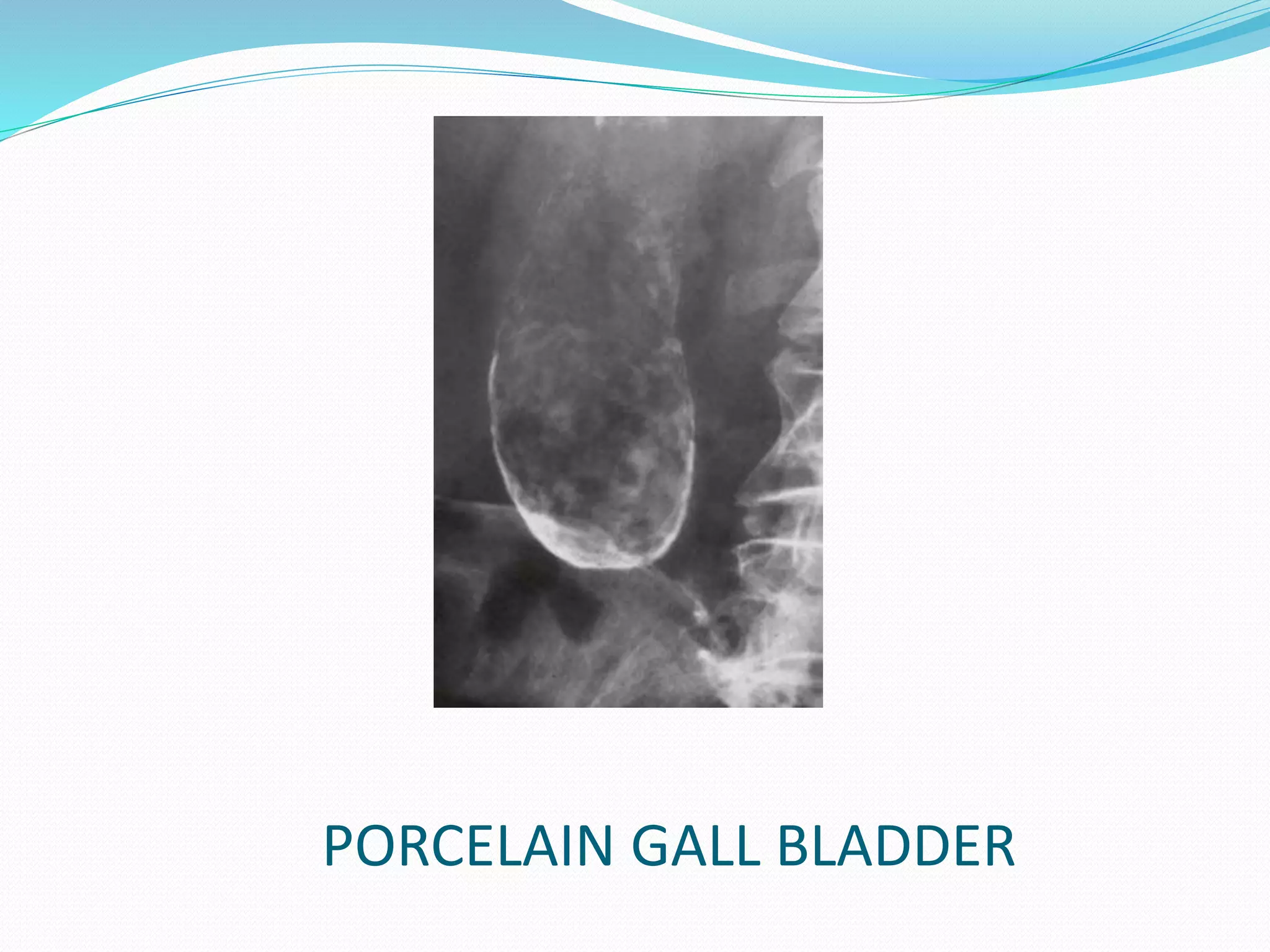
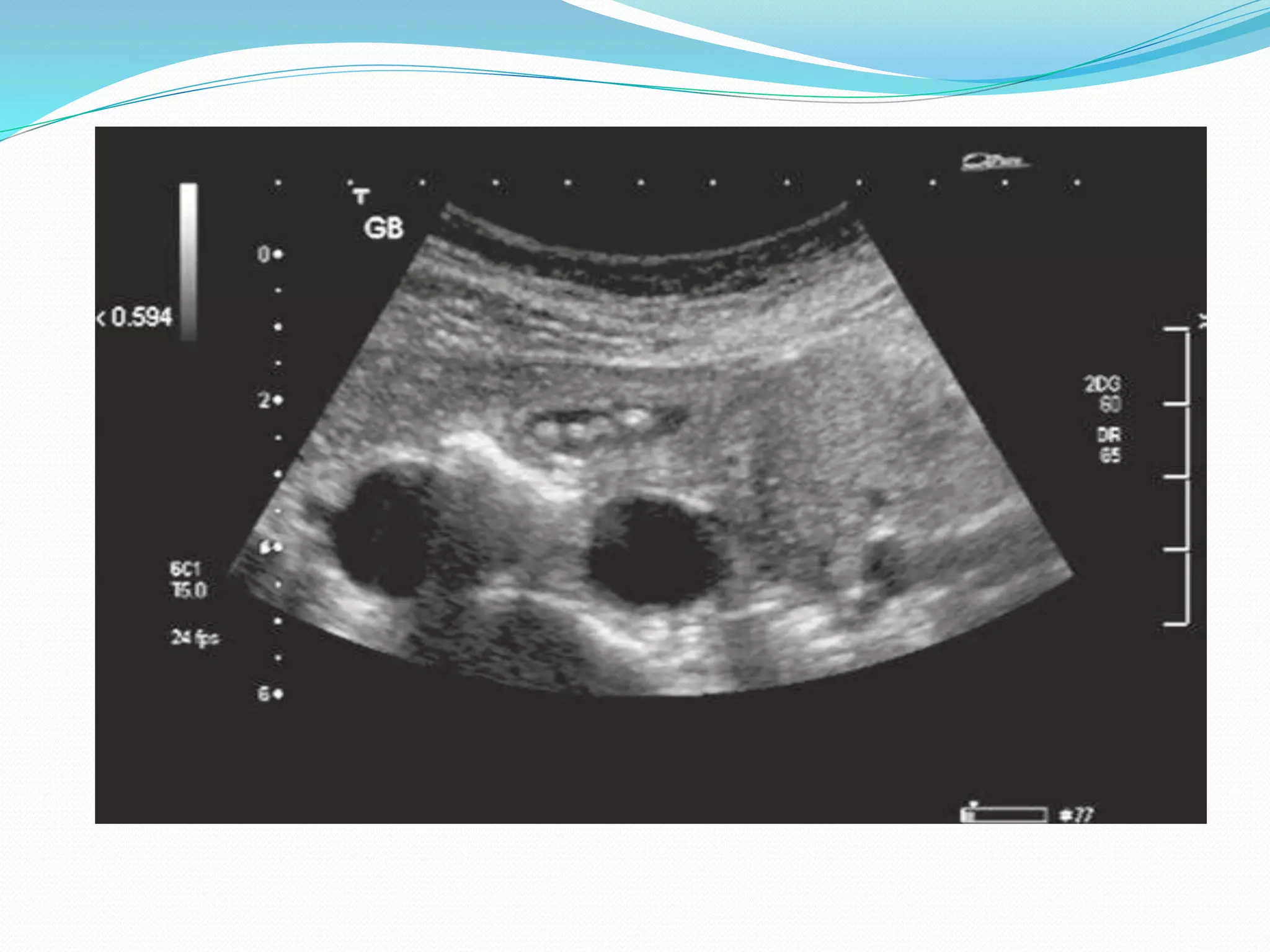
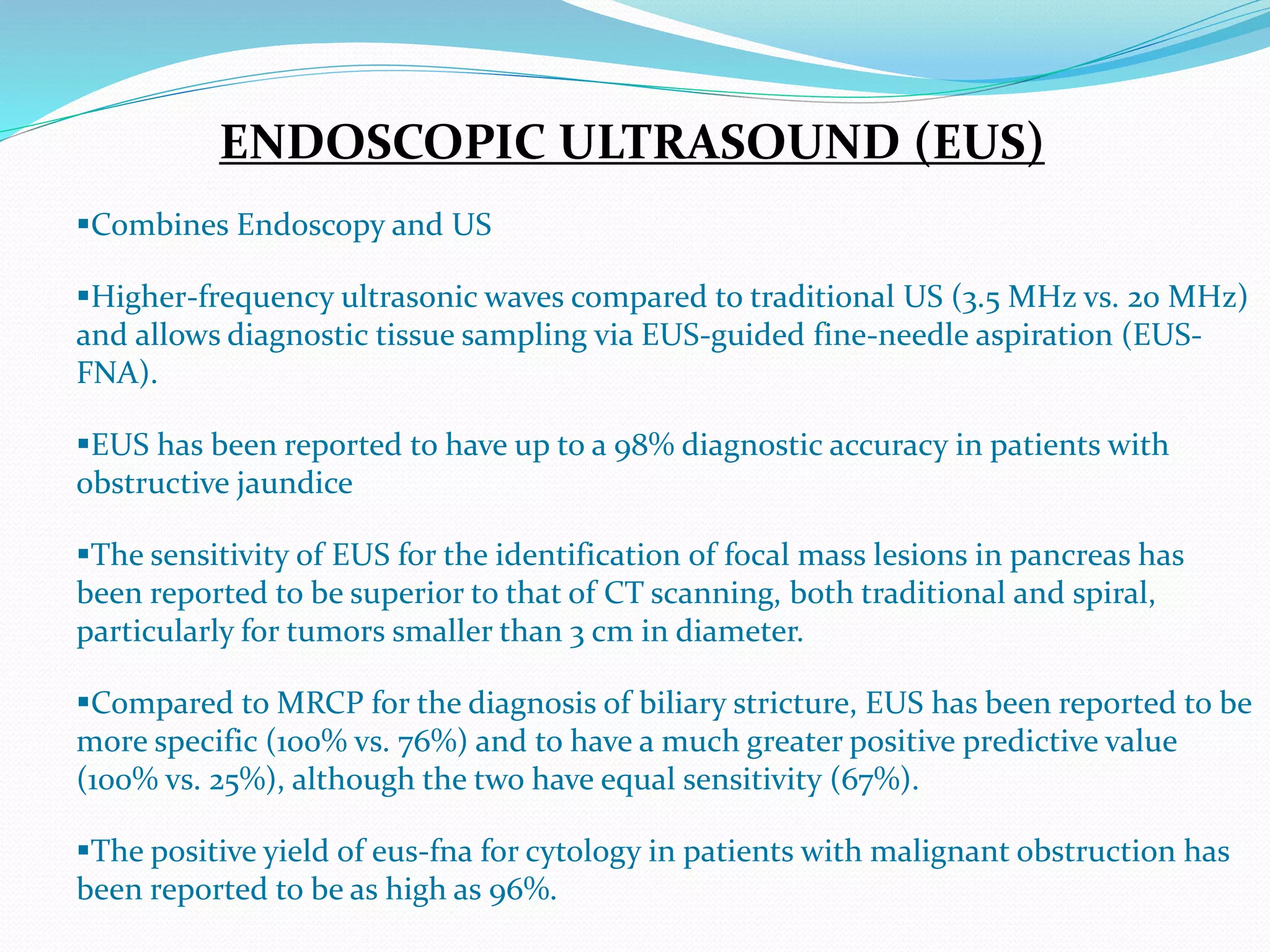
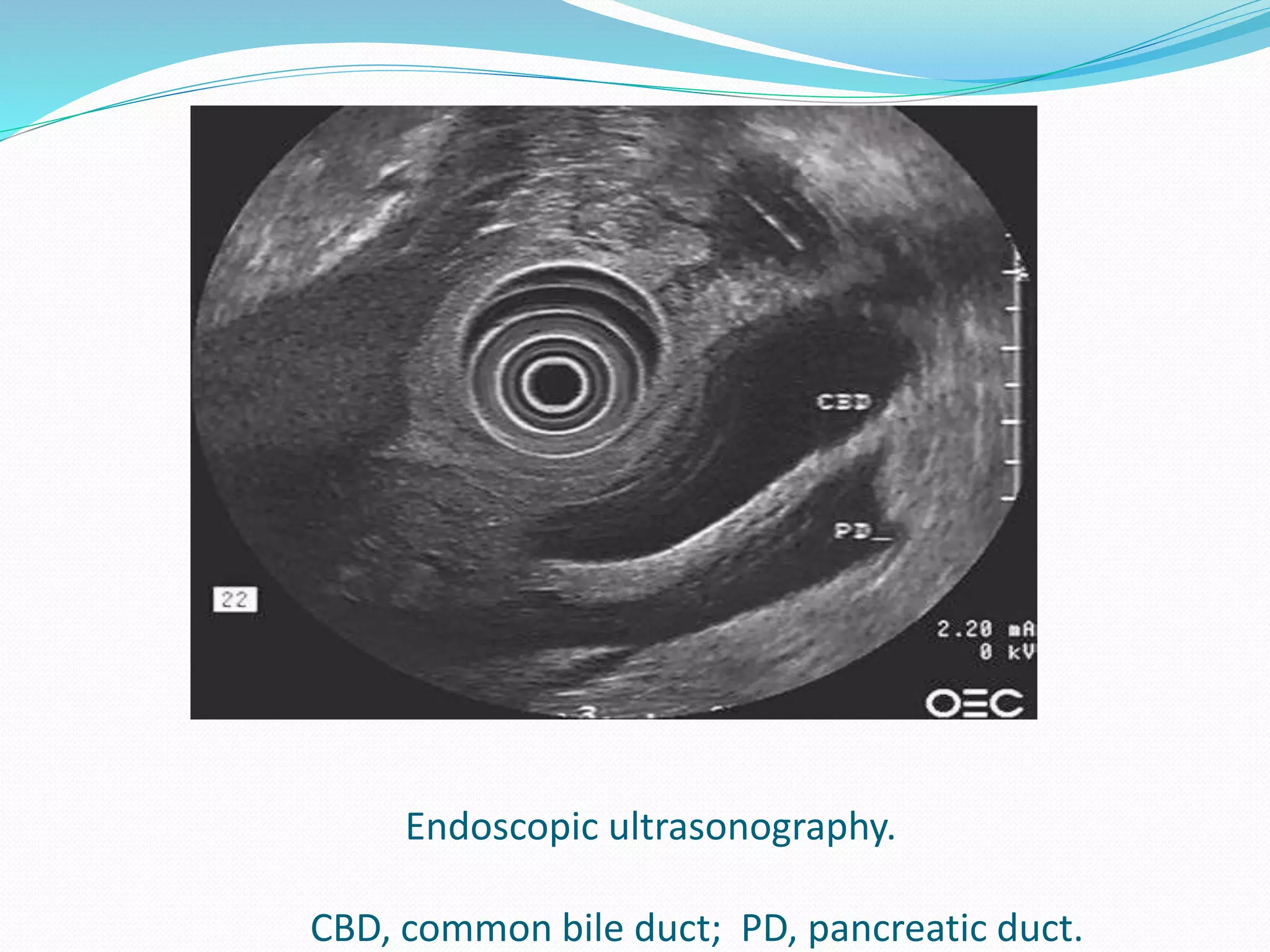
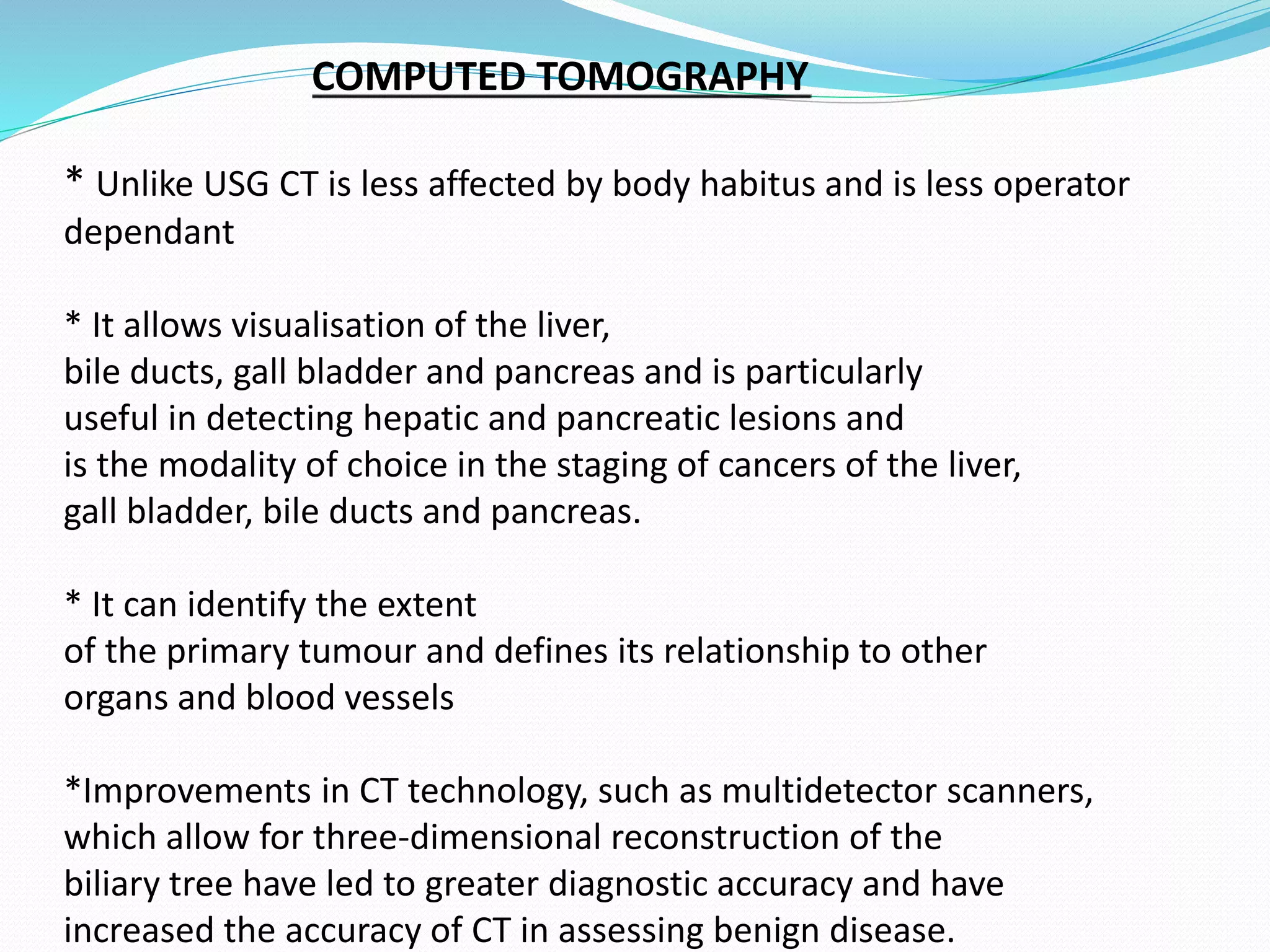
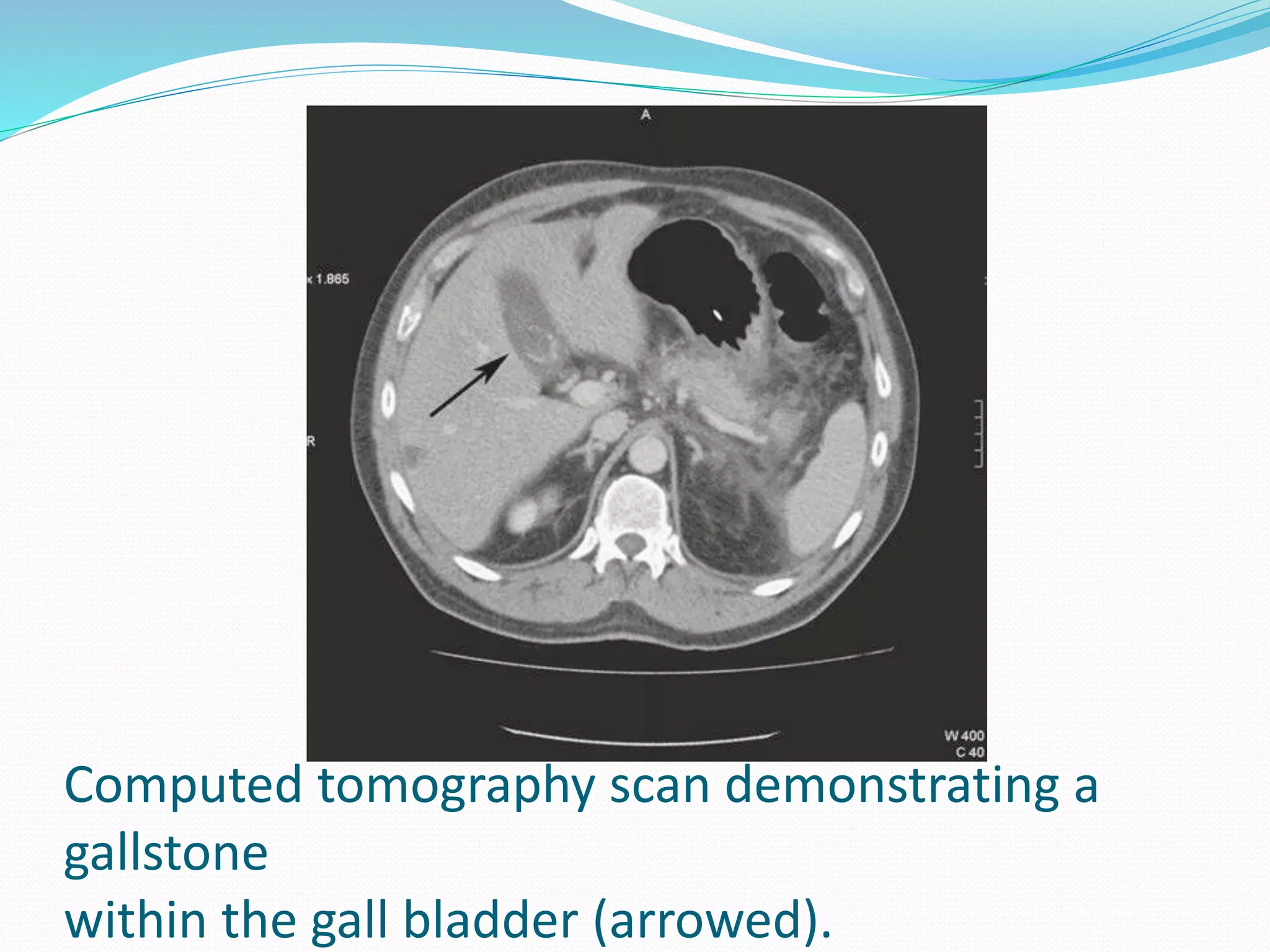
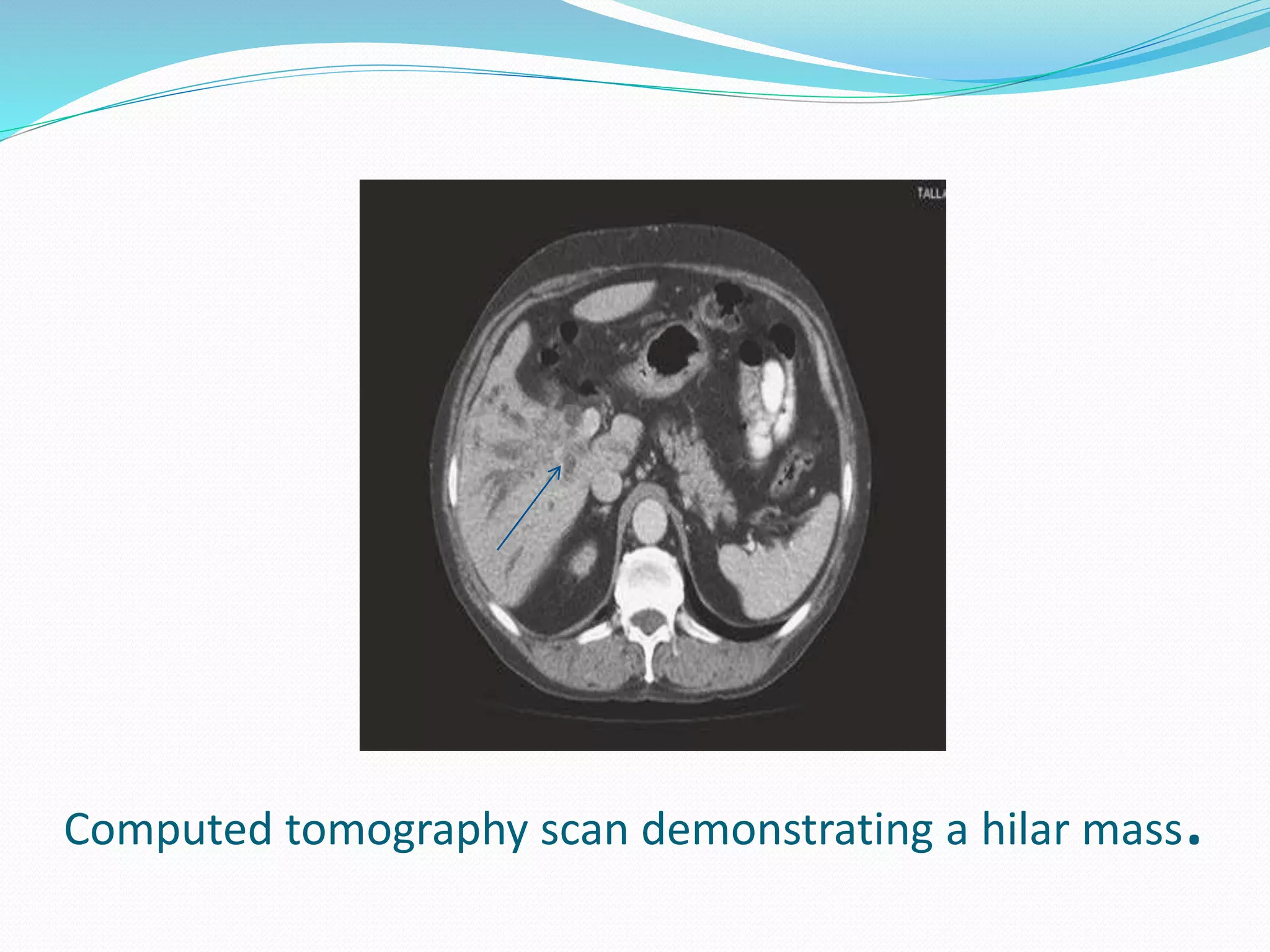
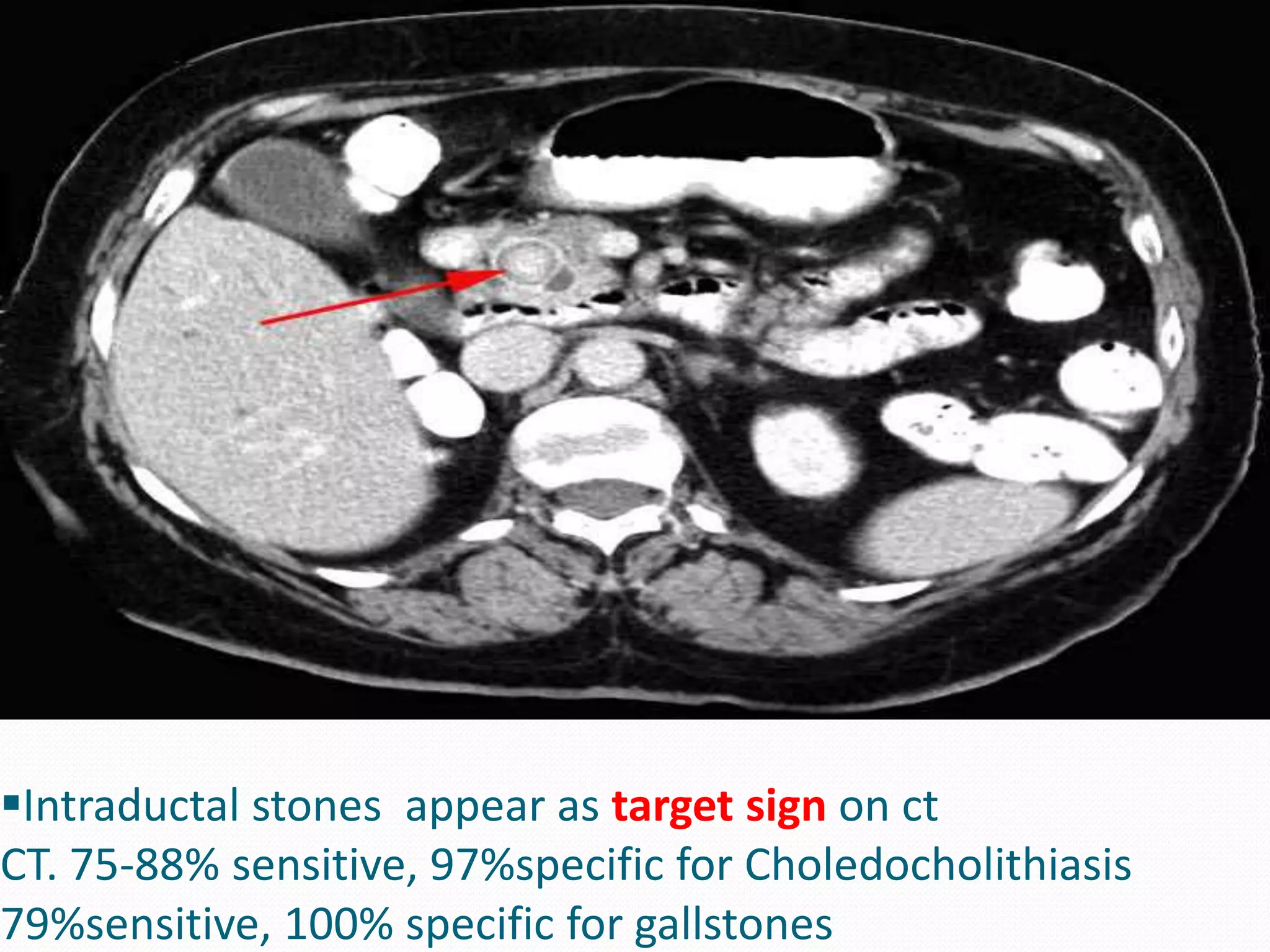
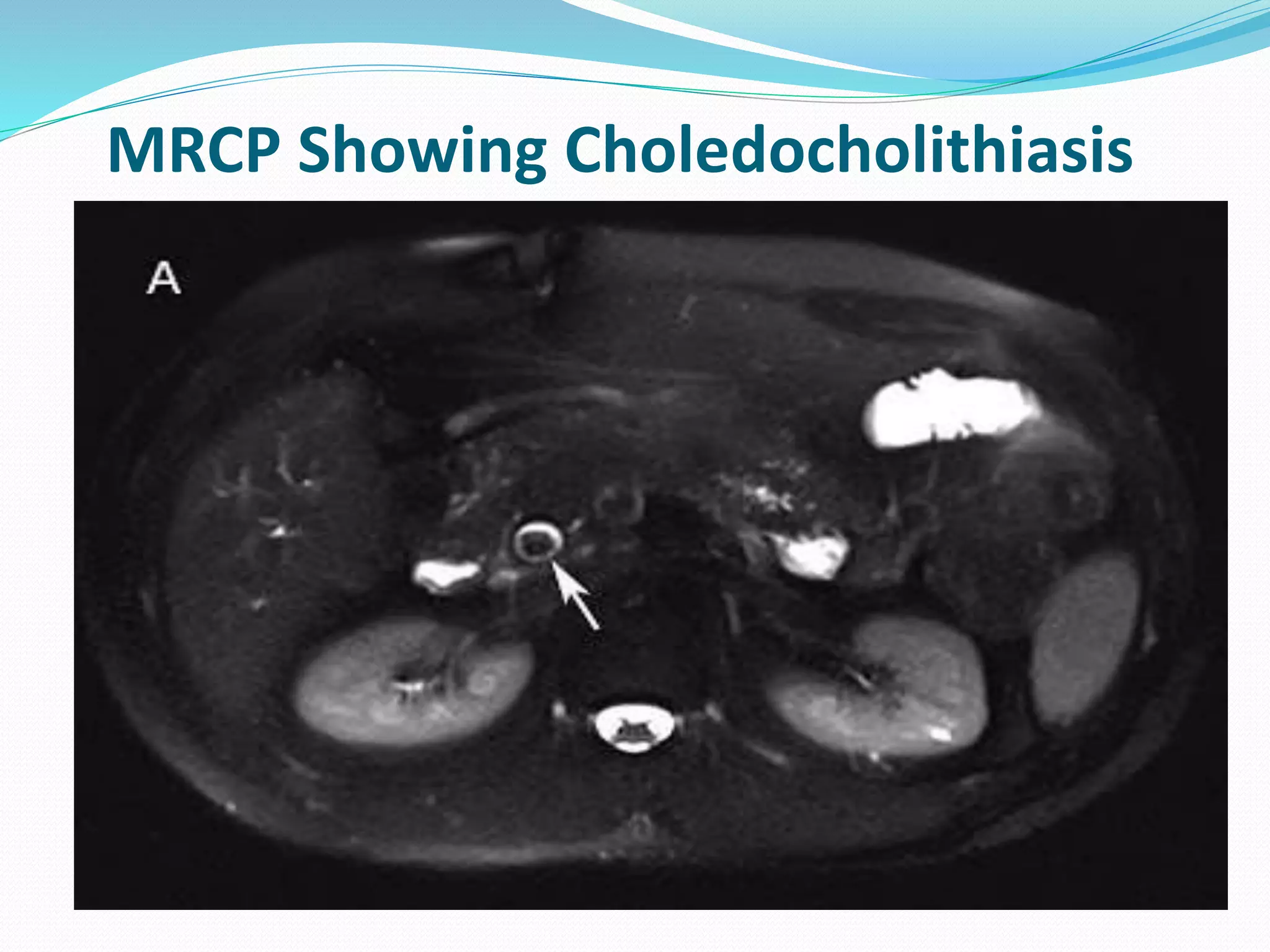
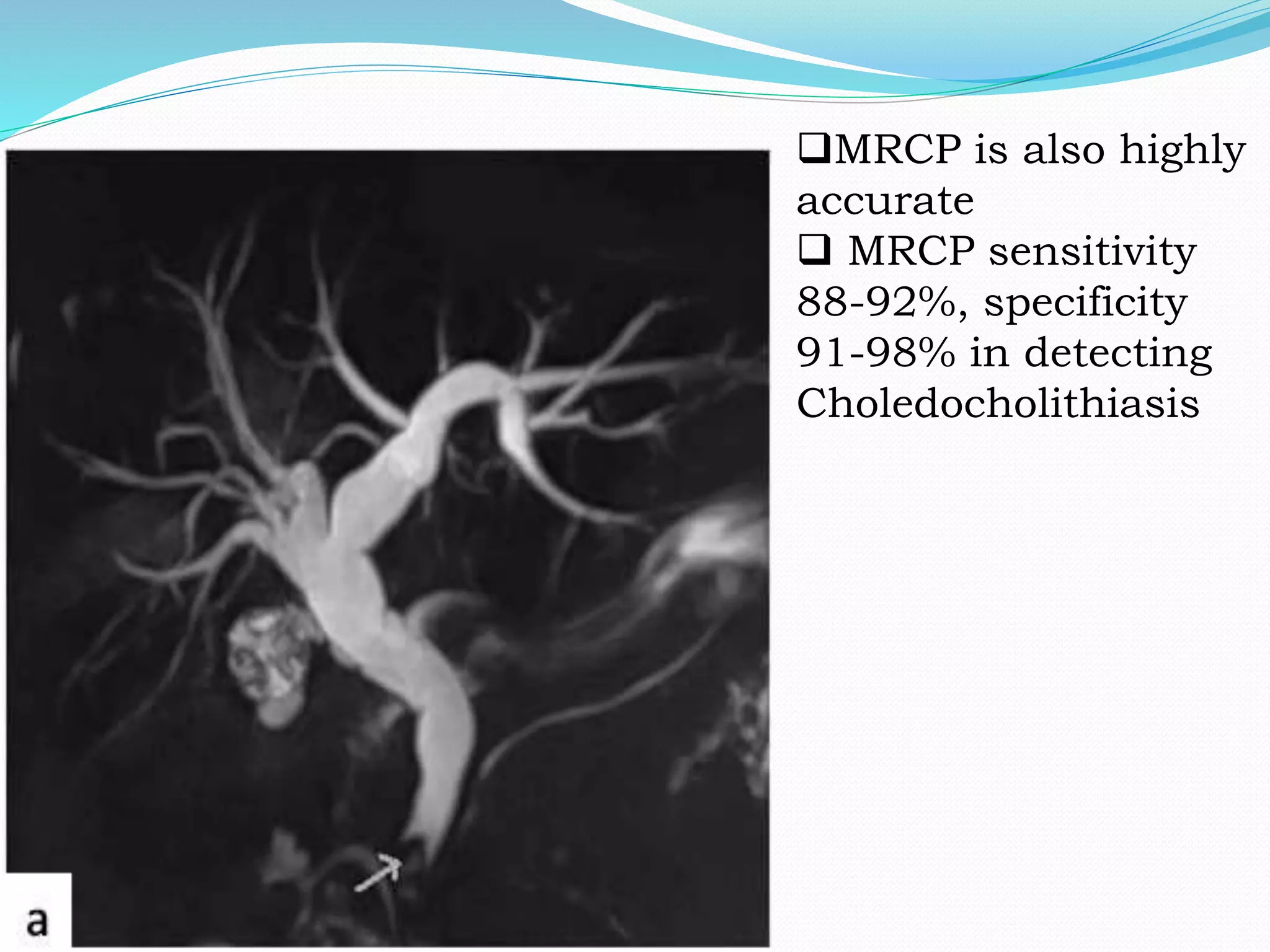
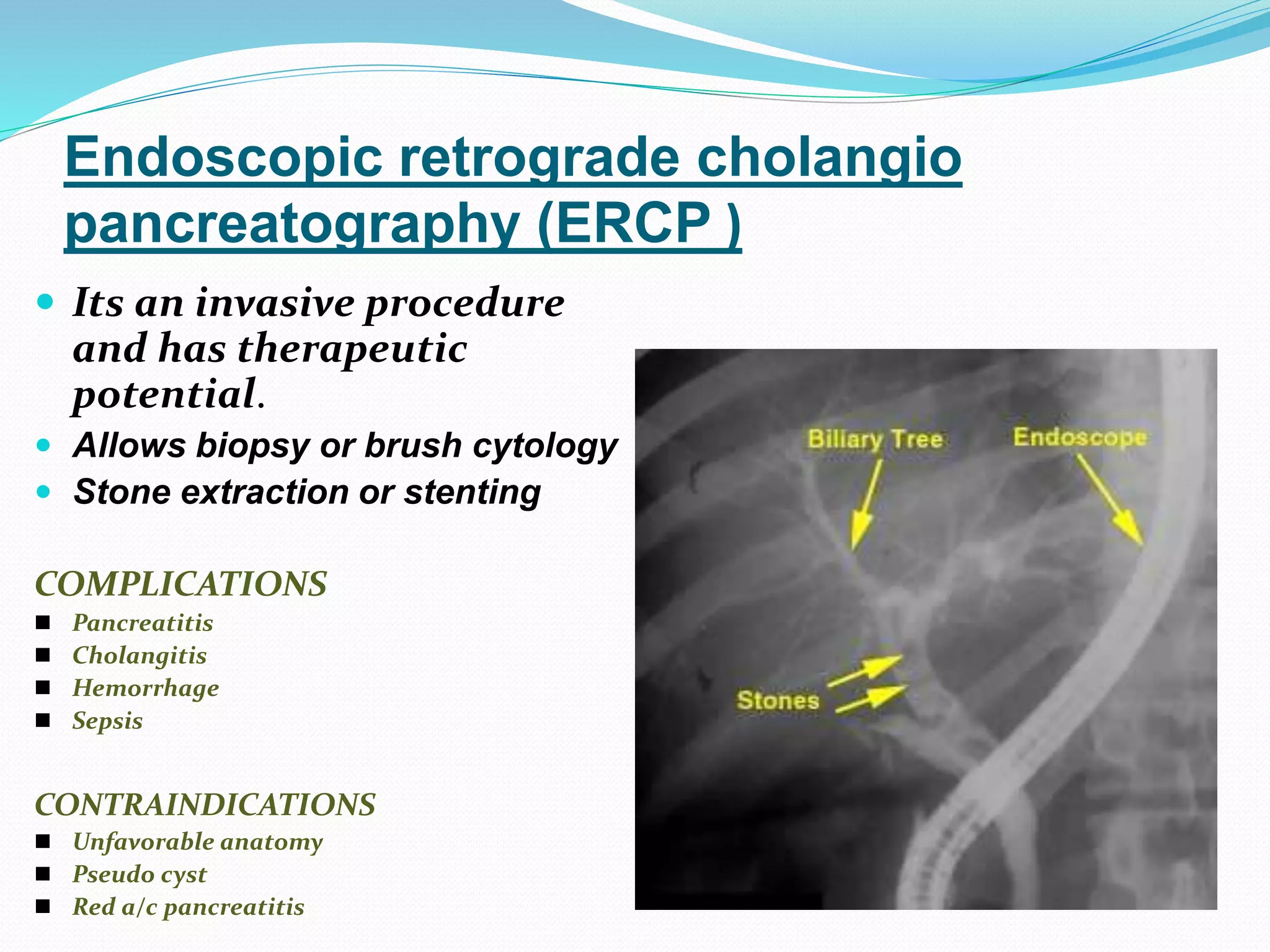
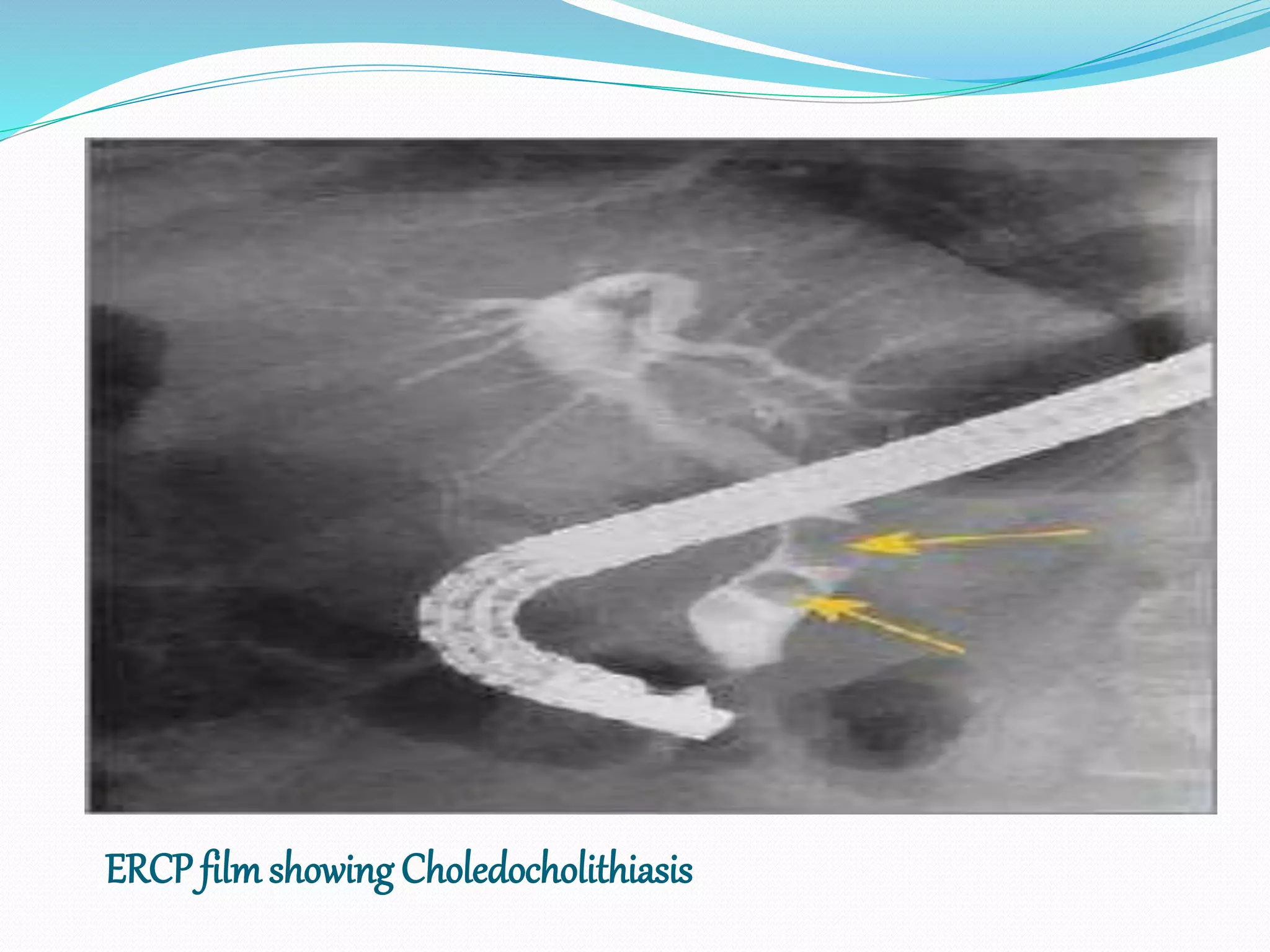
This document discusses the various investigations and classifications of obstructive jaundice, detailing the causes, laboratory tests, and imaging methods used for diagnosis. It outlines types of jaundice—complete, intermittent, chronic incomplete, and segmental obstruction—as well as laboratory and radiological evaluations essential for determining the level and cause of obstruction. Additionally, it reviews diagnostic techniques such as endoscopic ultrasound and imaging methods, including CT and MRCP, highlighting their respective sensitivities and specificities.