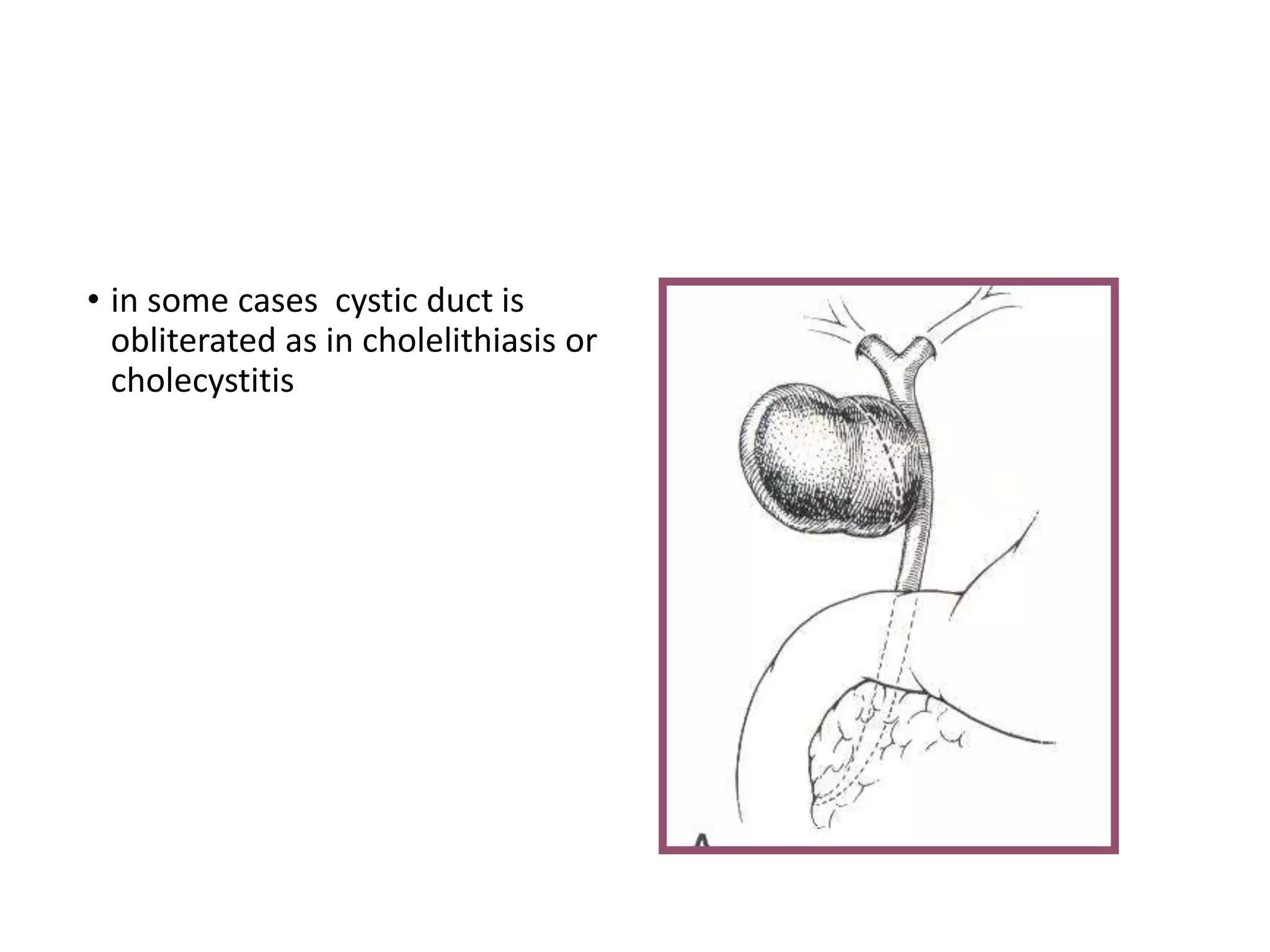
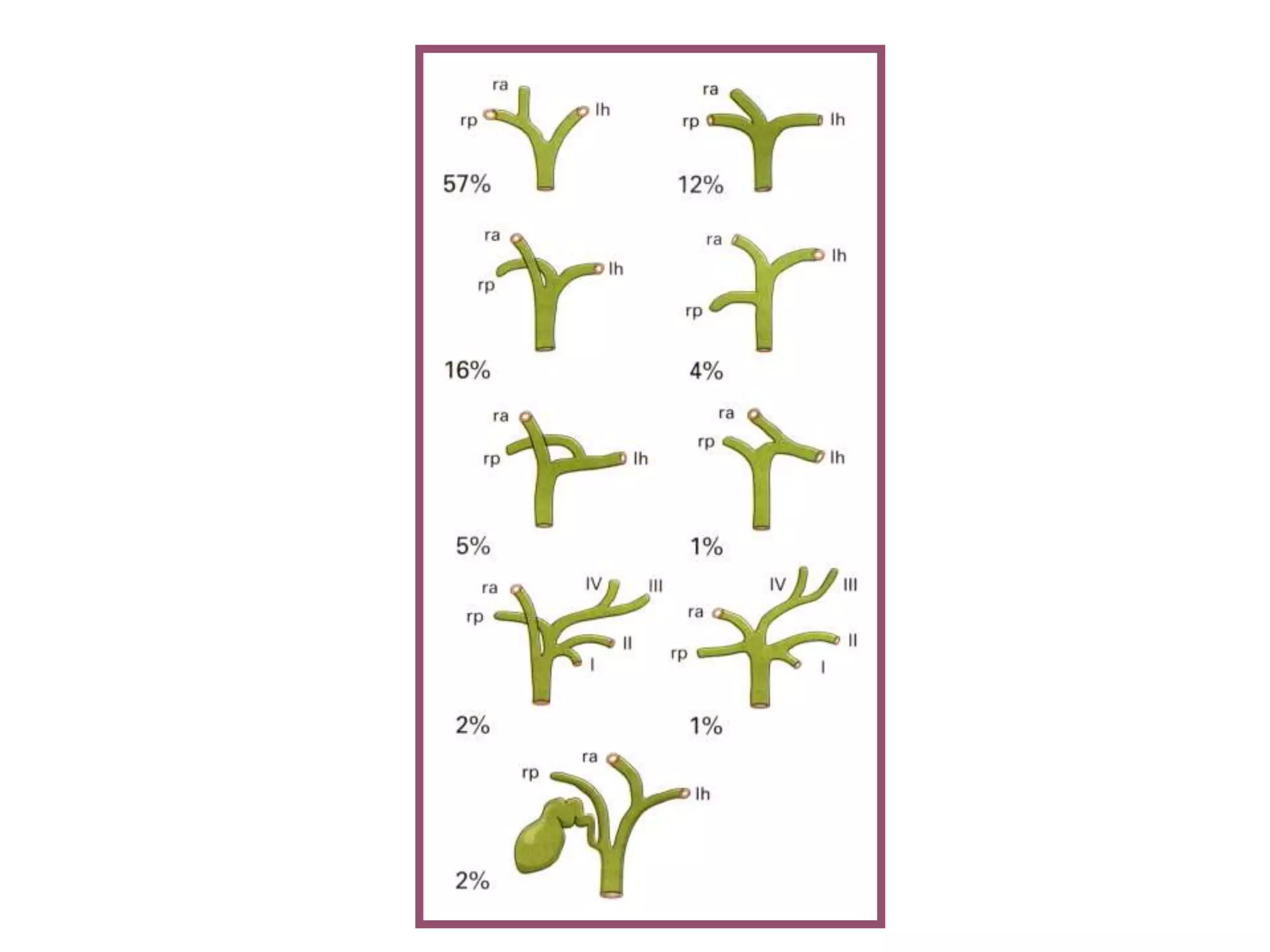
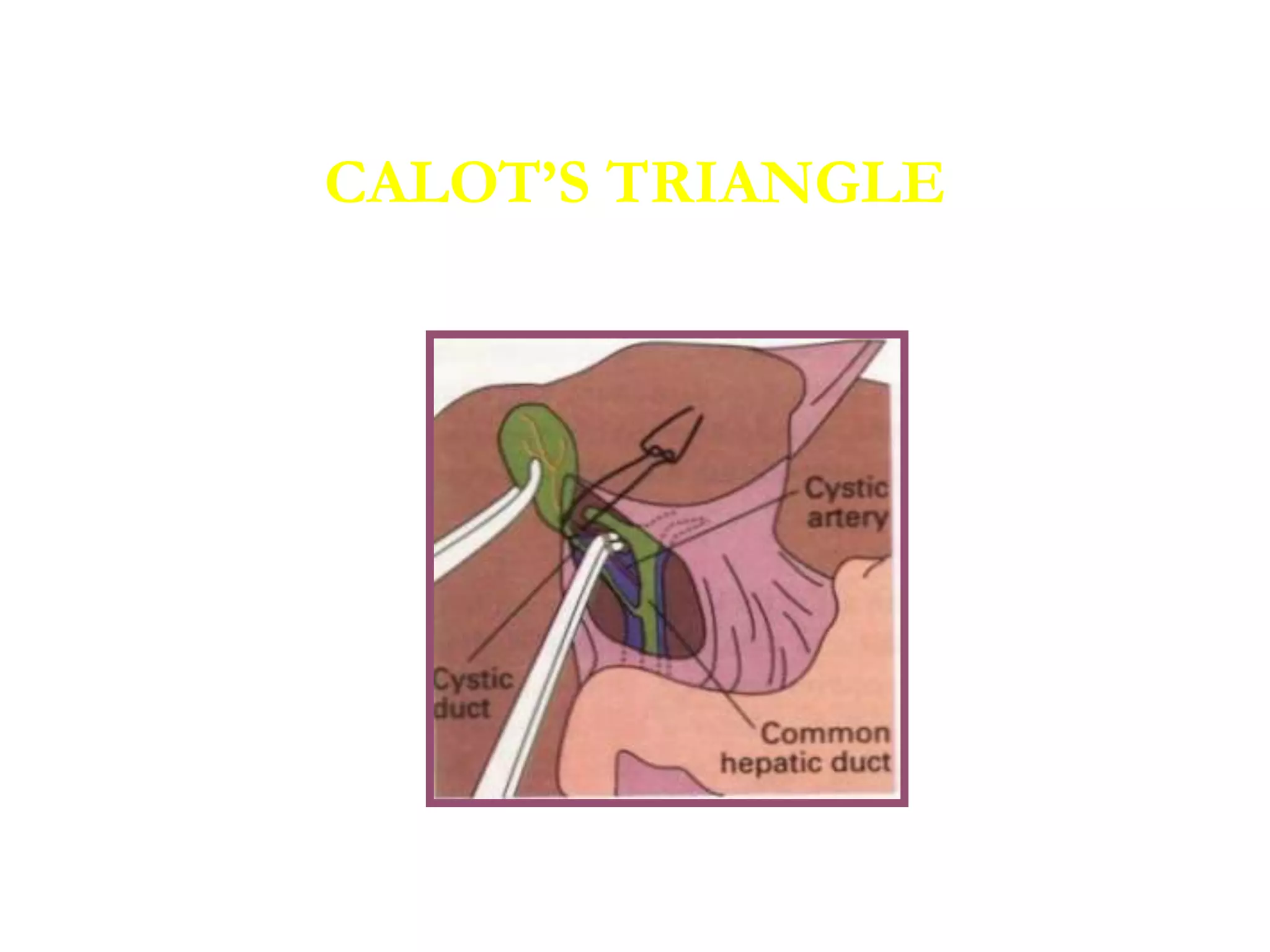
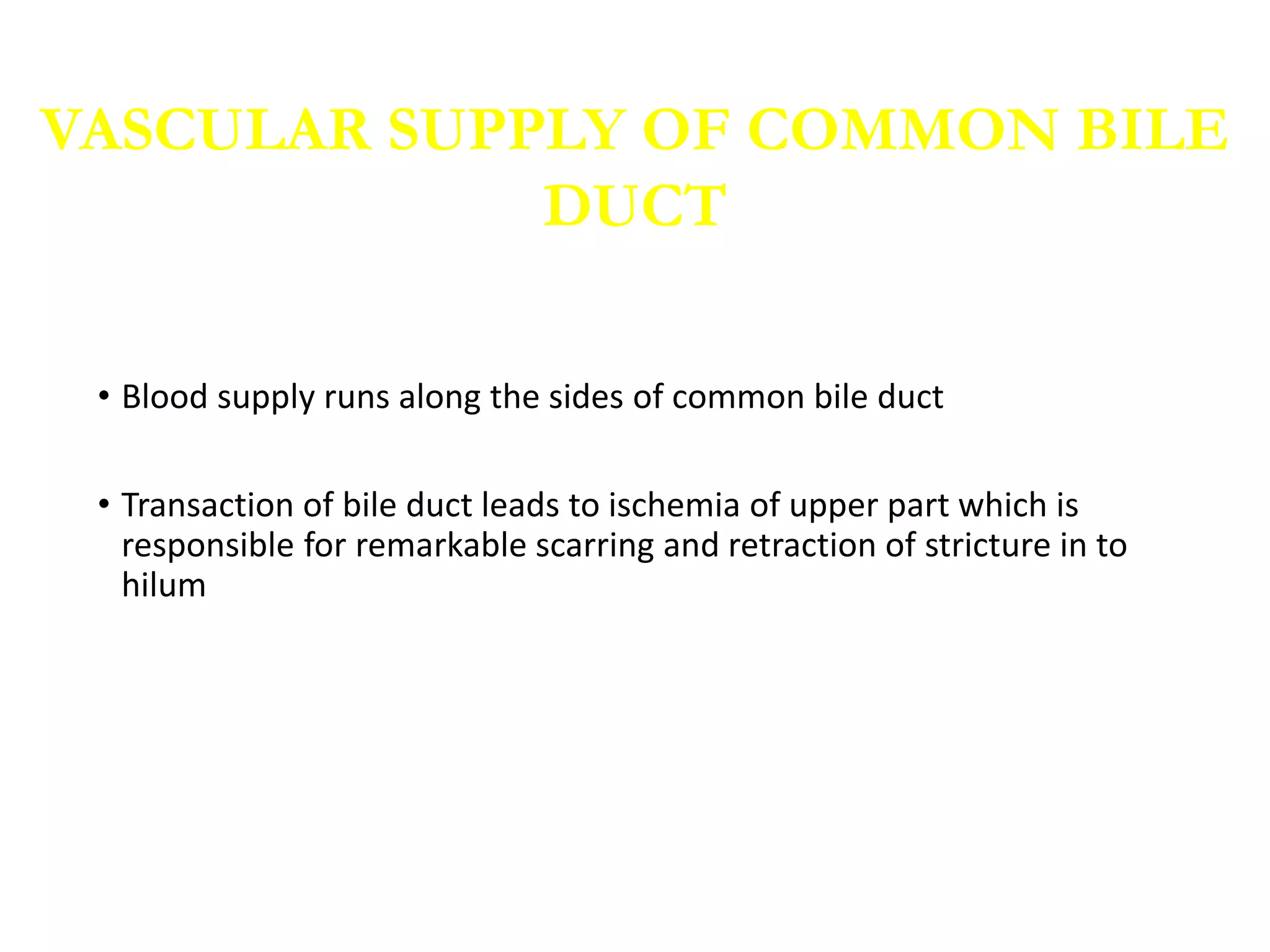
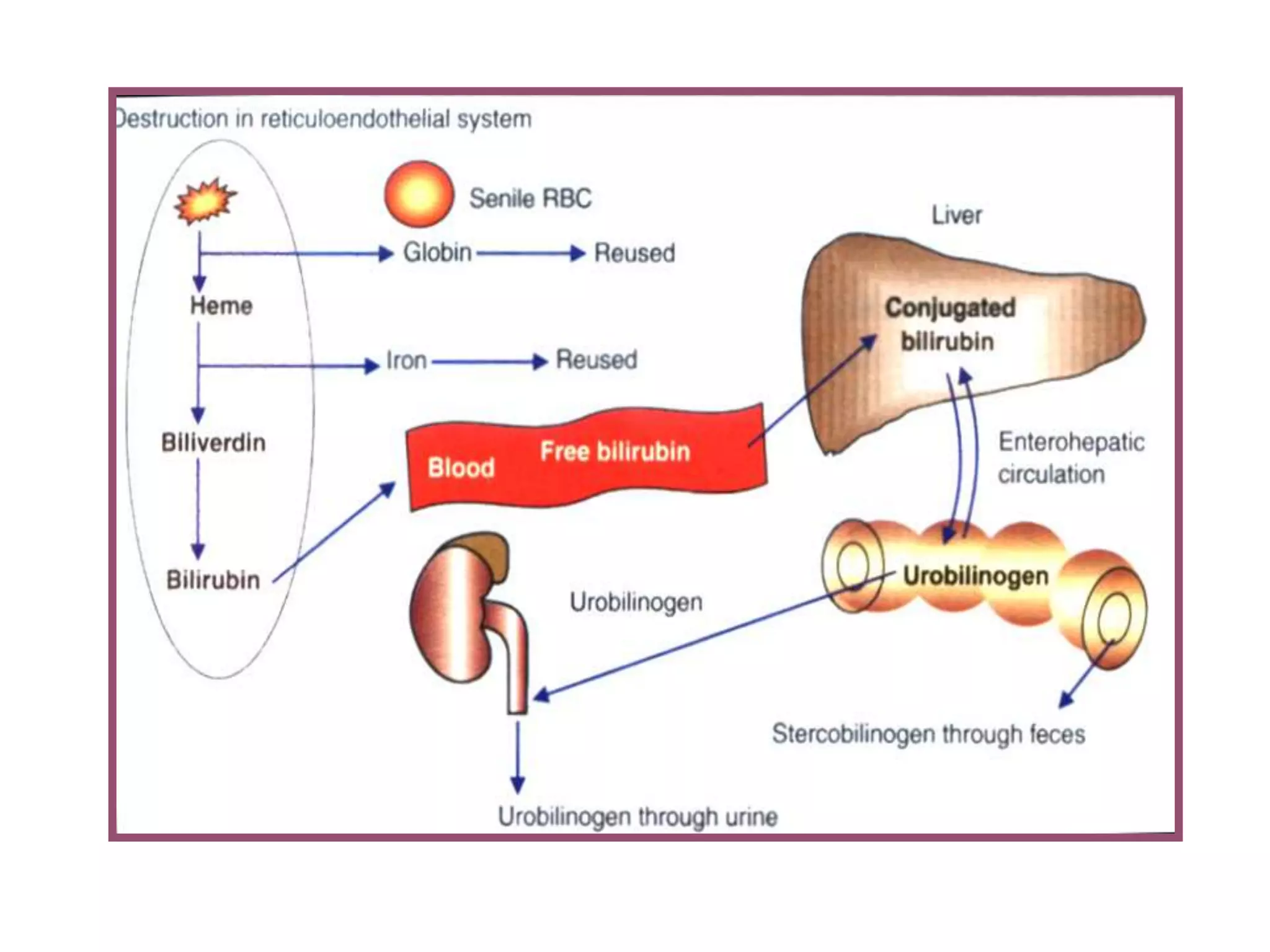
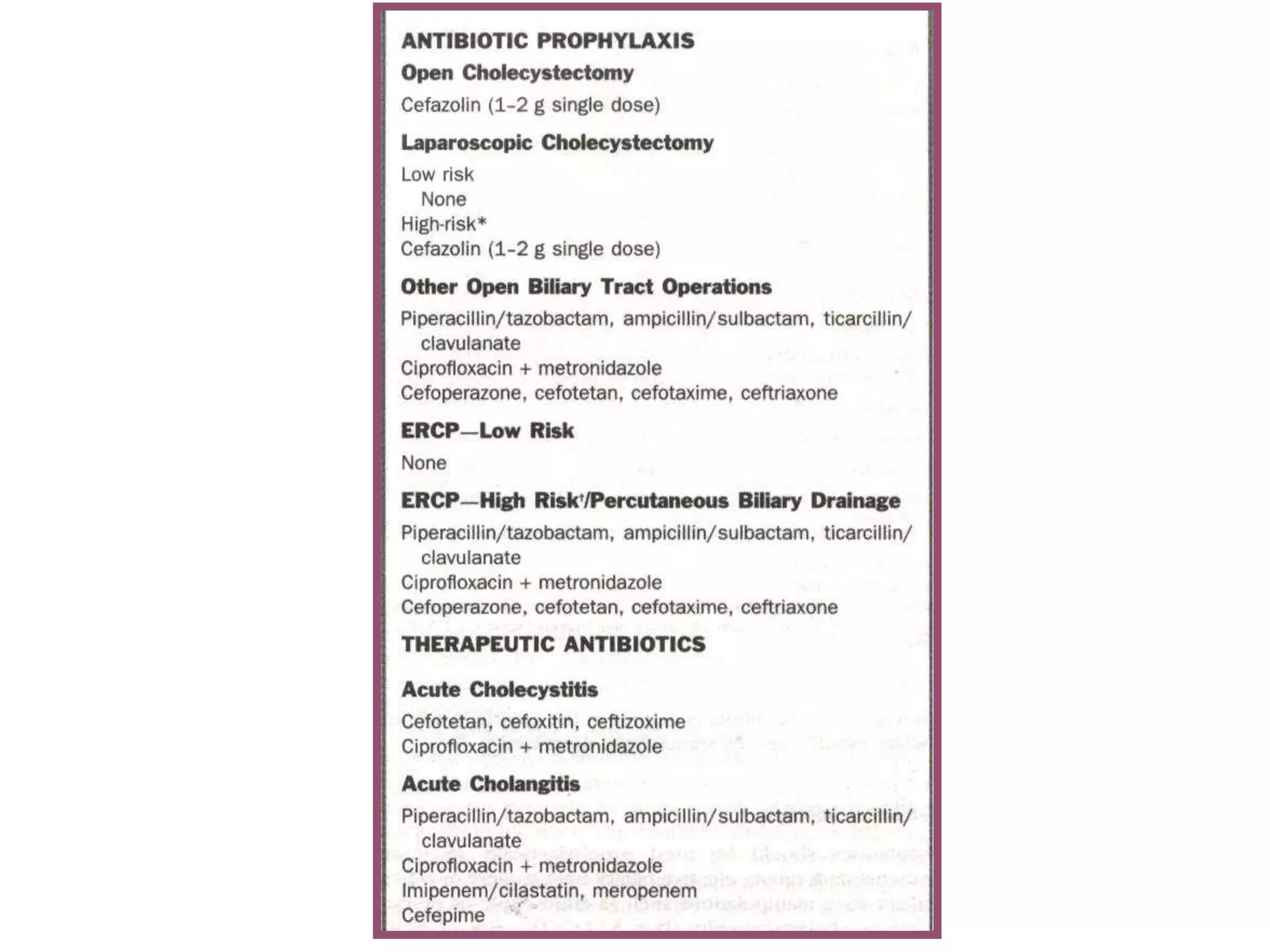
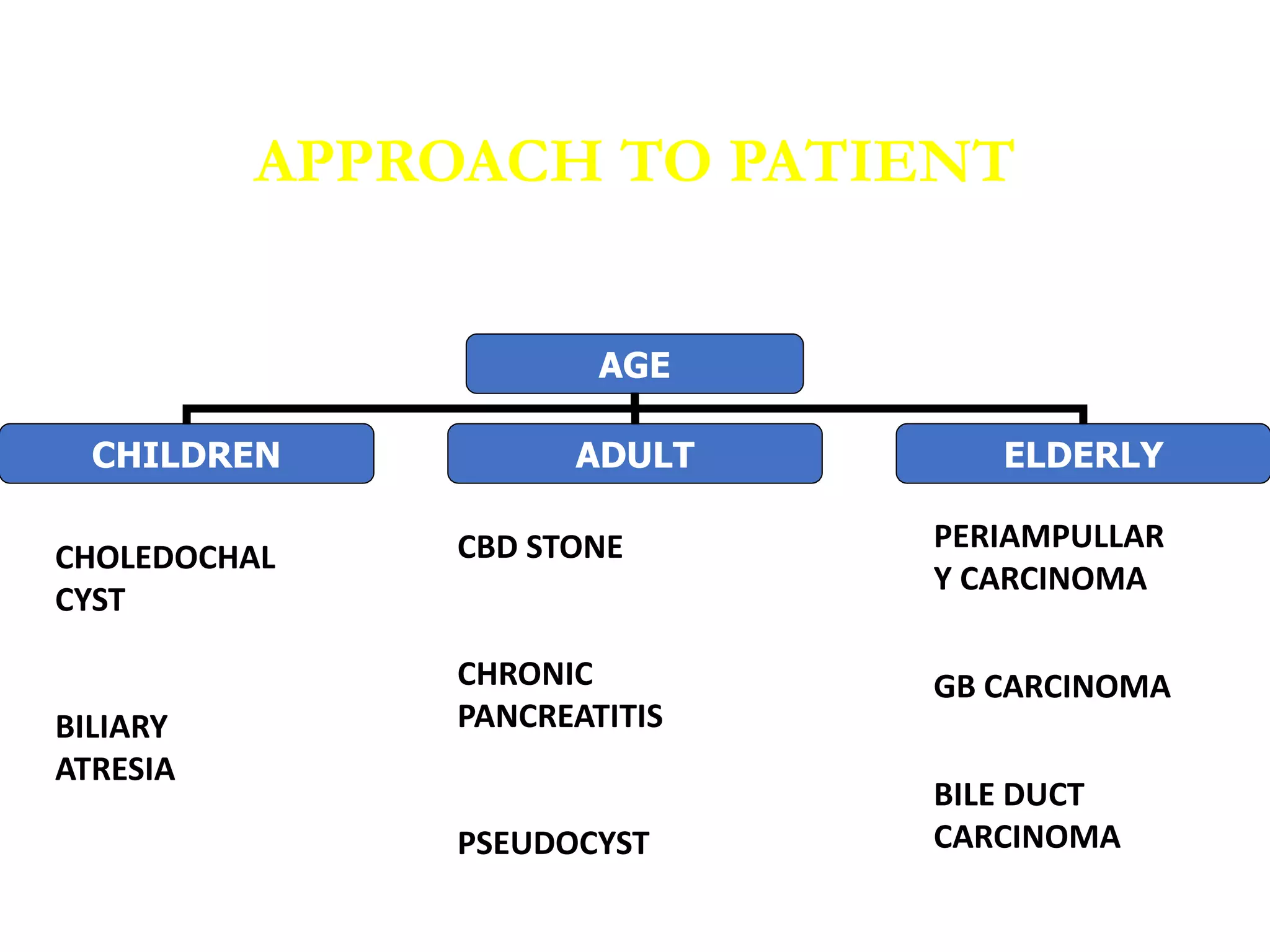
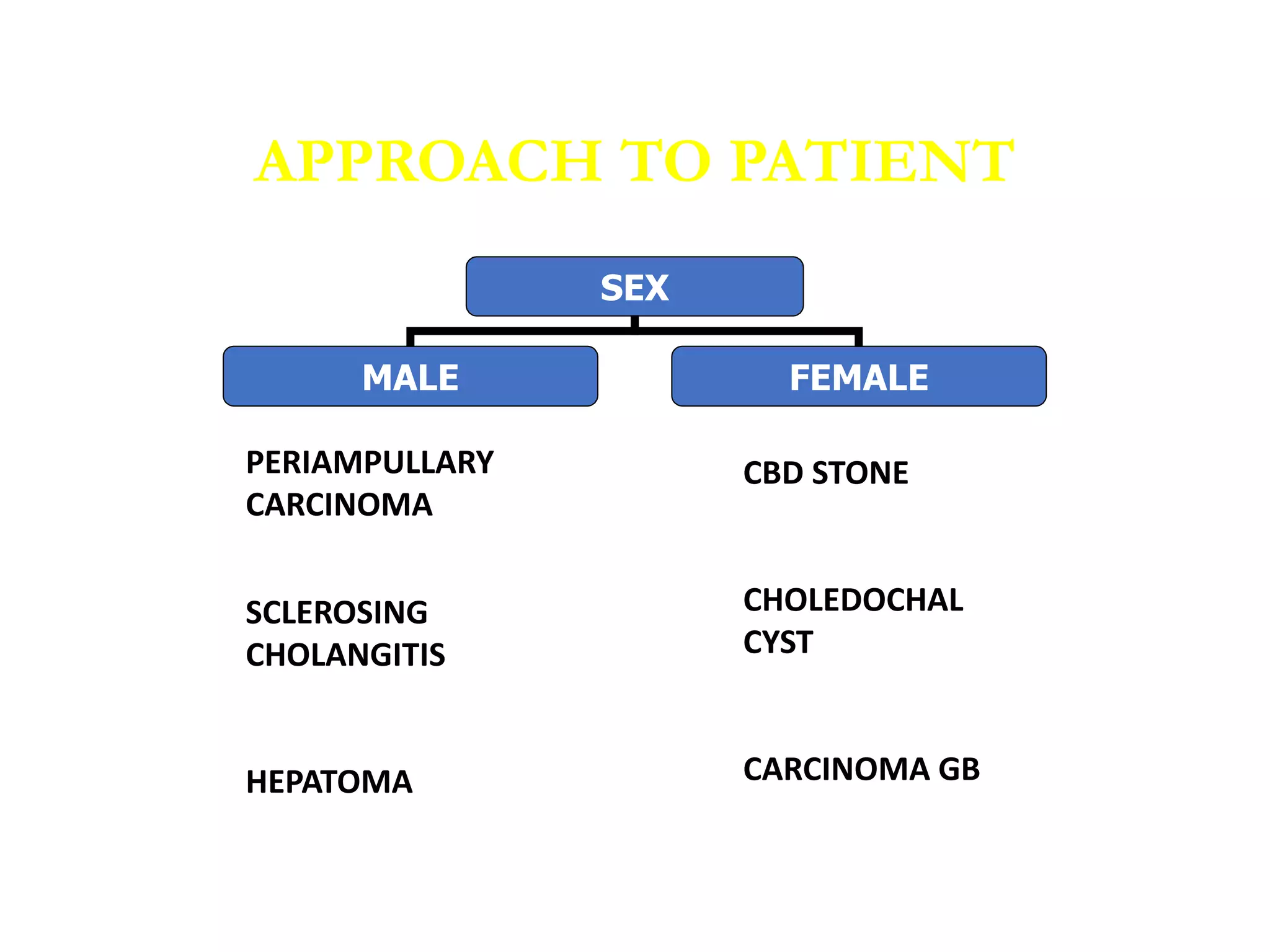
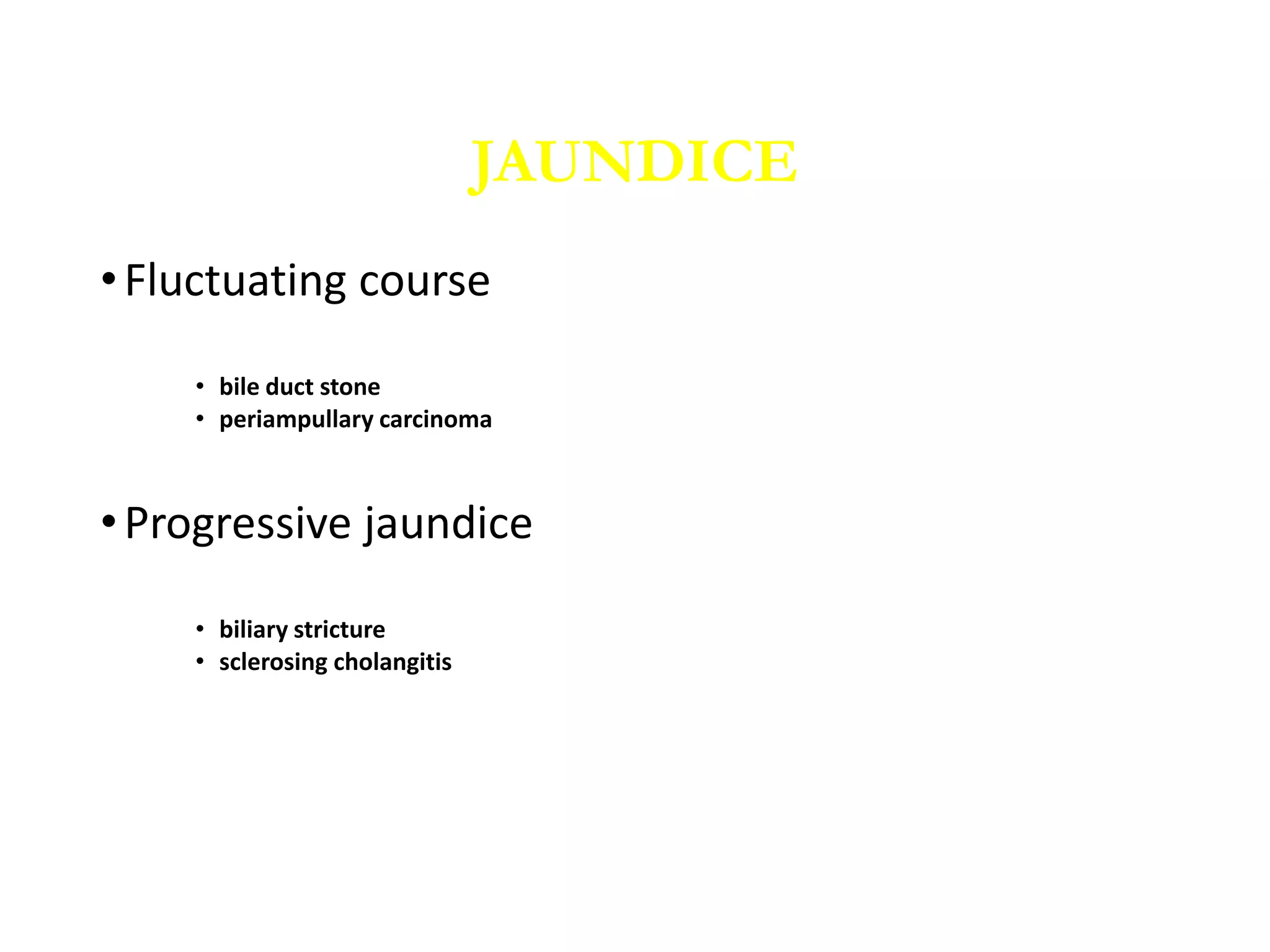
This document provides information on obstructive jaundice, including its definition, relevant anatomy, physiology, pathophysiology, causes, clinical presentation, and approach to patients. Obstructive jaundice is caused by cholestasis or obstruction of the biliary tree, leading to conjugated hyperbilirubinemia. The biliary tree has significant anatomical variations that surgeons must be aware of. Clinical features may include jaundice, abdominal pain, weight loss, fever, and more, depending on the underlying cause which can include gallstones, tumors, strictures, or other conditions. A thorough history and physical exam is important to evaluate obstructive jaundice.