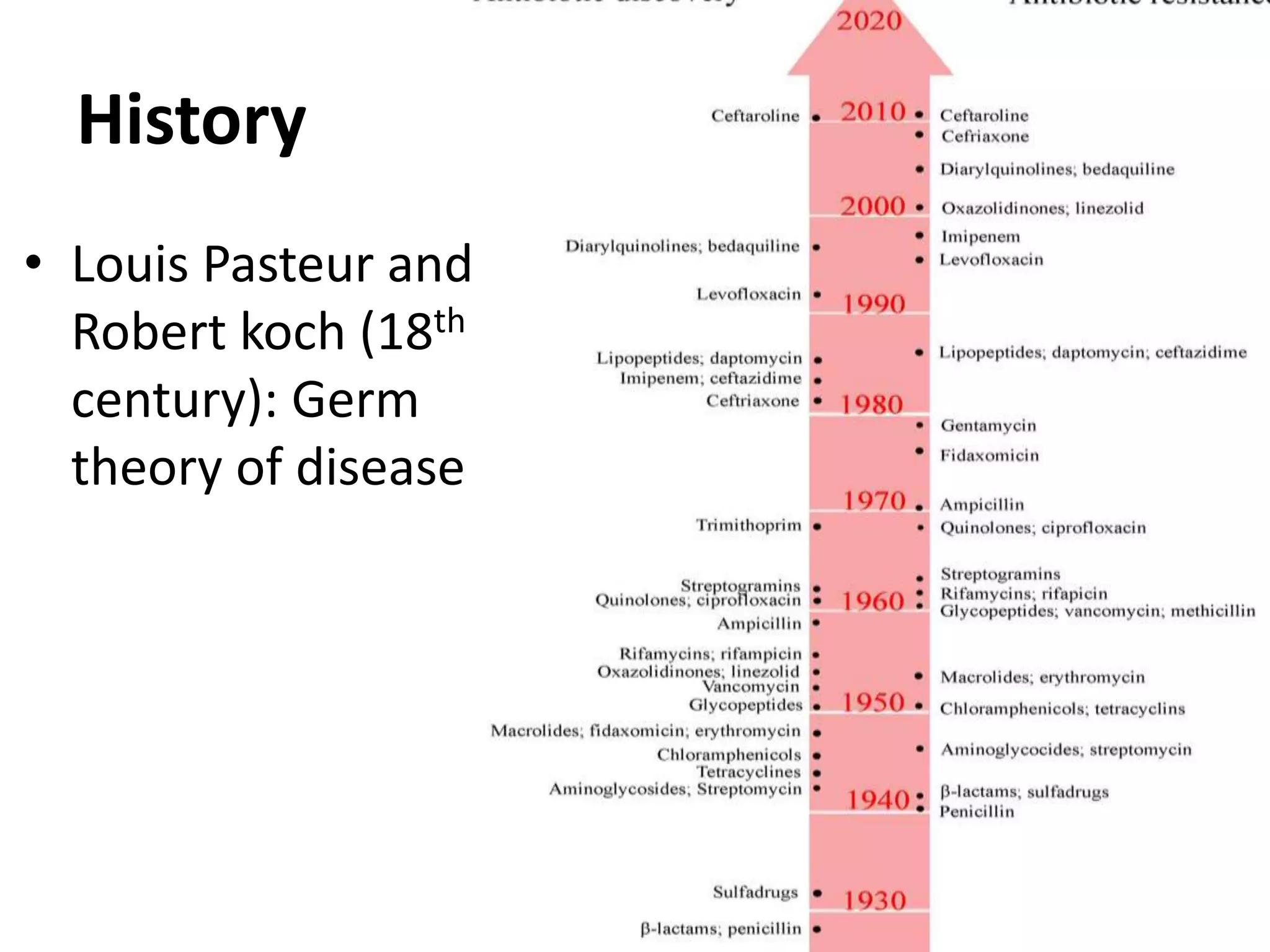
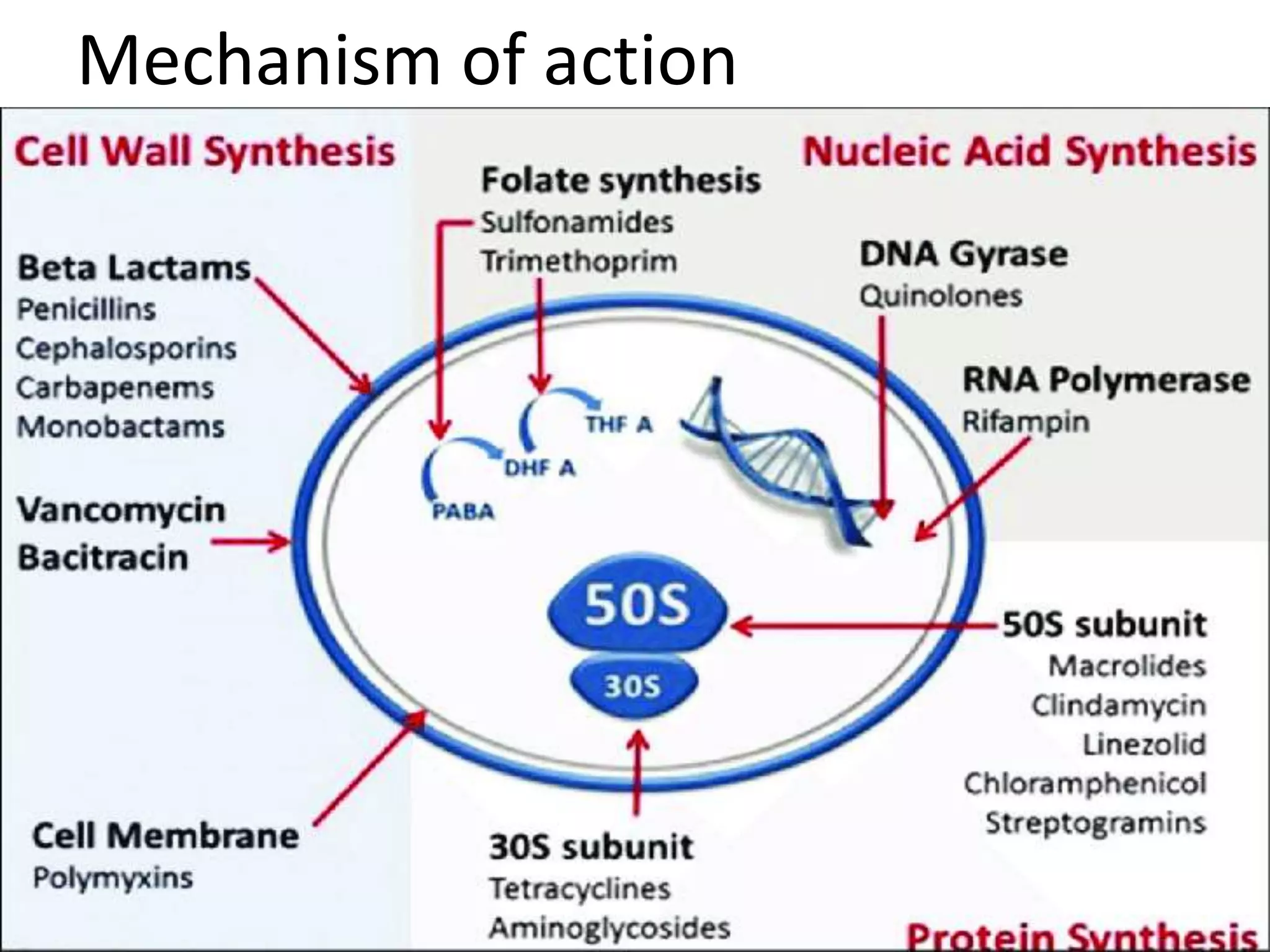
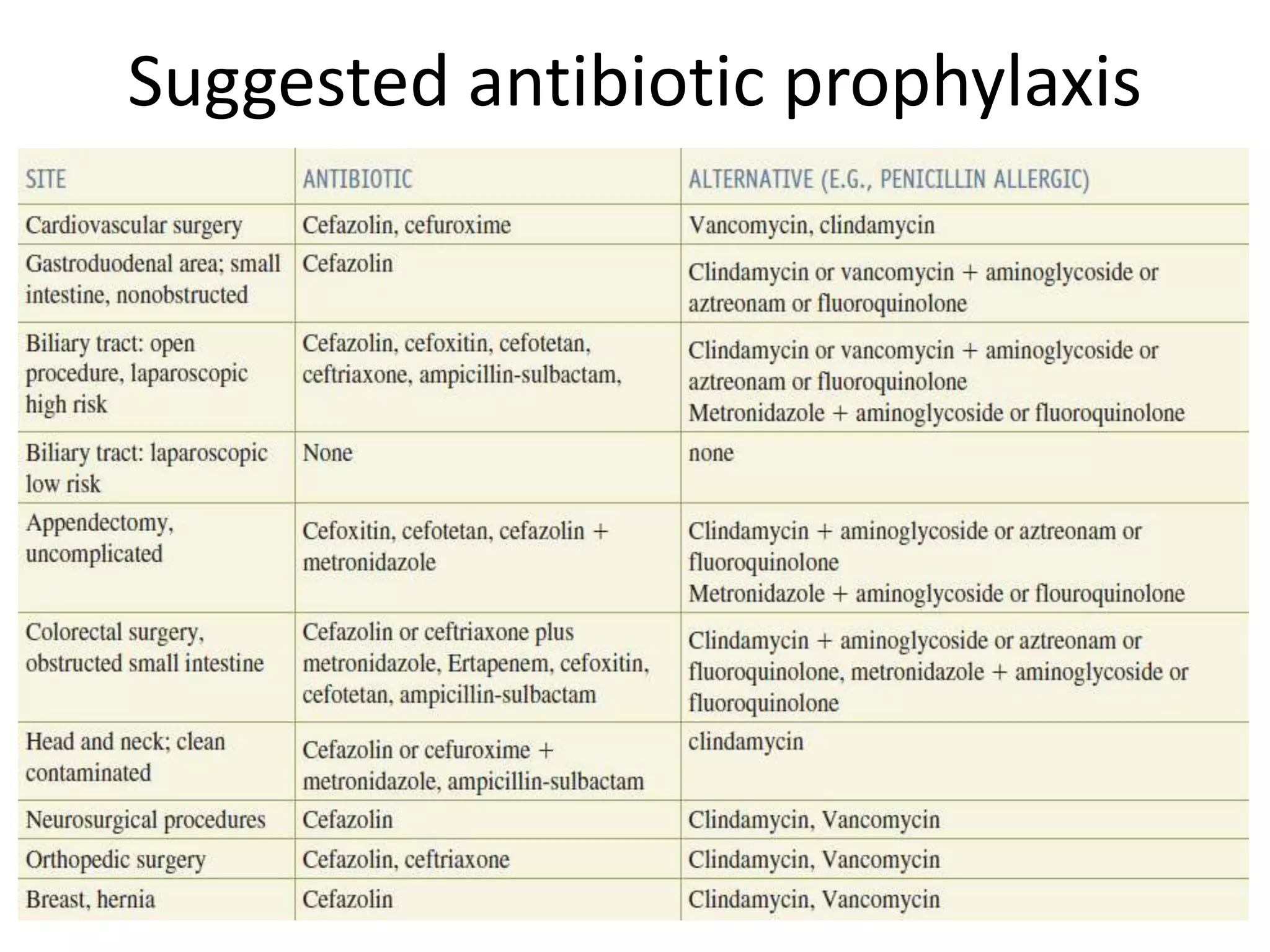
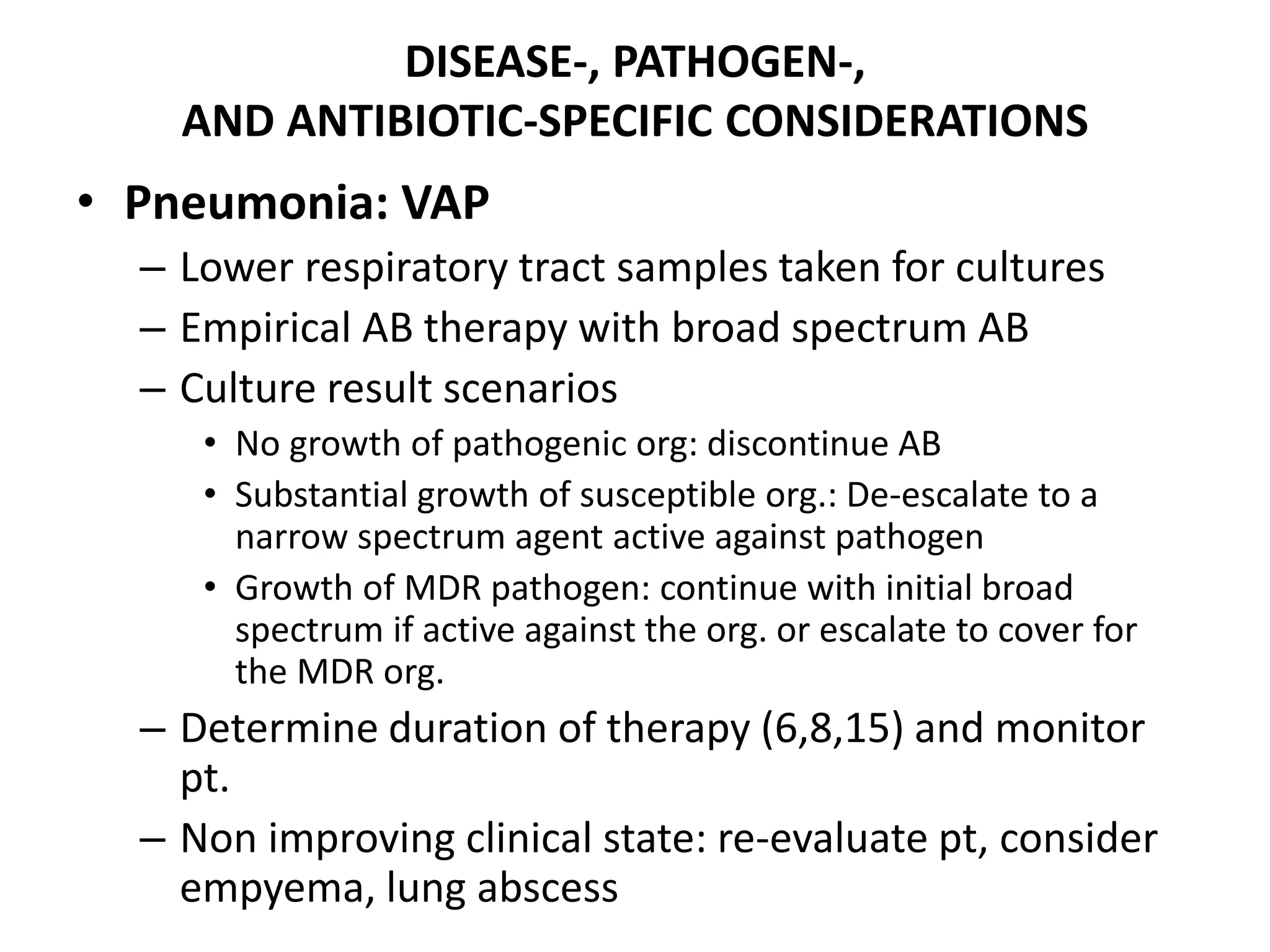
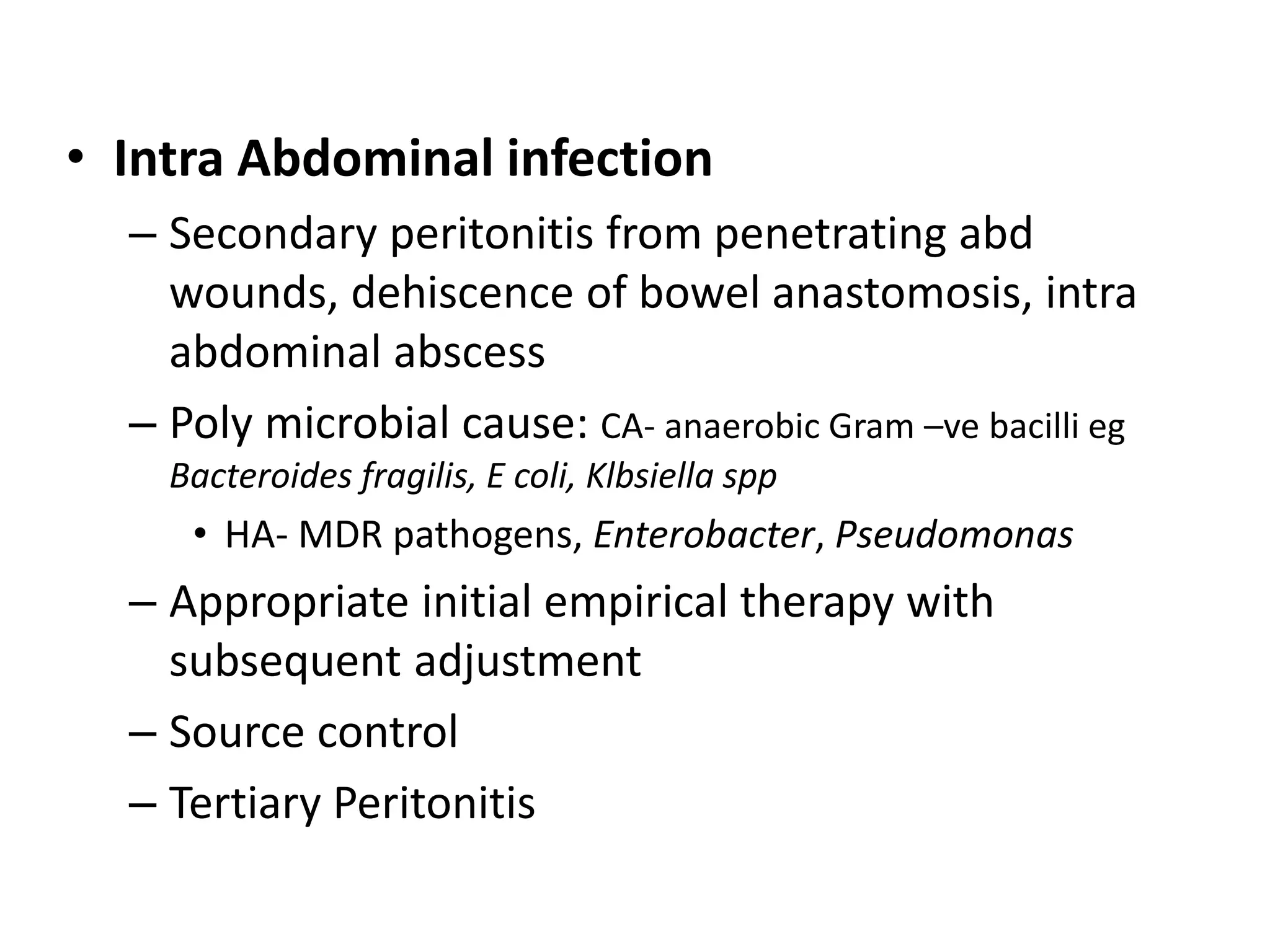
The document provides an extensive overview of the use of antibiotics in surgical settings, emphasizing their role in preventing and treating infections. It covers classifications, therapeutic applications, monitoring, abuse, resistance issues, and future trends in antibiotic usage. The importance of adhering to proper surgical techniques and guidelines to reduce complications and threats posed by antibiotic misuse is highlighted.