1. Obstructive jaundice results from obstruction of bile flow from the liver to the duodenum, causing bilirubin levels to rise above 2.5mg/dL and resulting in jaundice.
2. The top 3 causes of obstructive jaundice are choledocholithiasis, strictures, and pancreatic cancer.
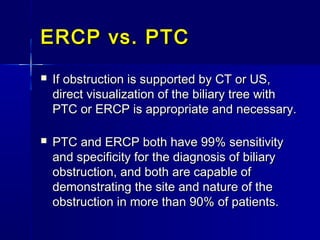
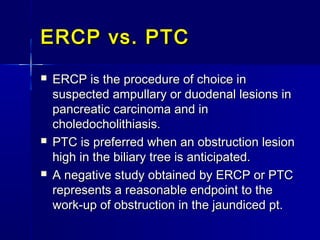
3. Evaluation involves clinical examination, blood tests of liver function and markers, ultrasound of the bile ducts, and CT or ERCP to visualize the biliary tree and determine the level and cause of obstruction.