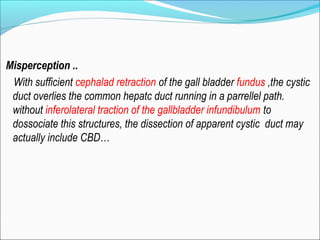
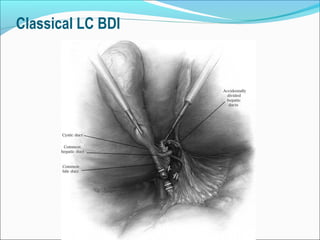
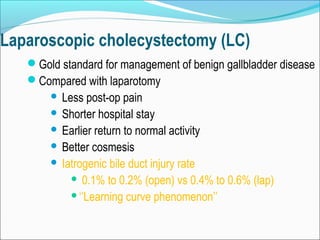
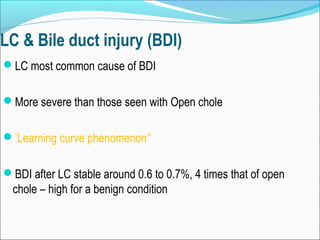
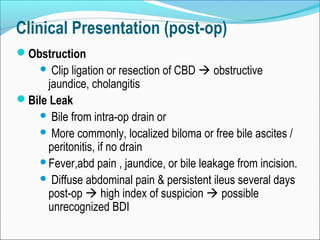
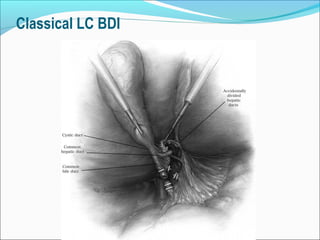
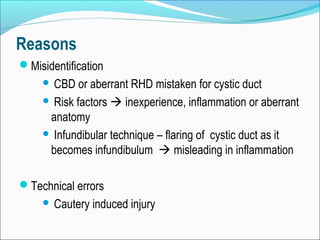
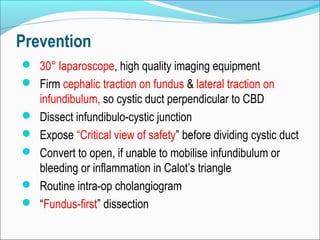
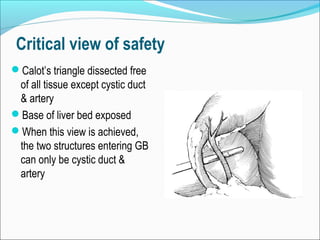
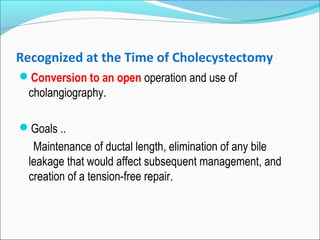
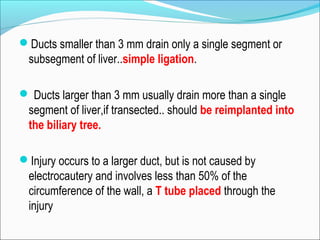
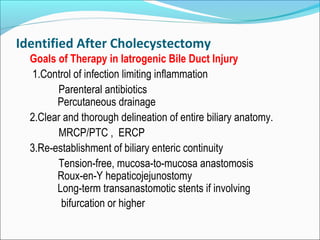
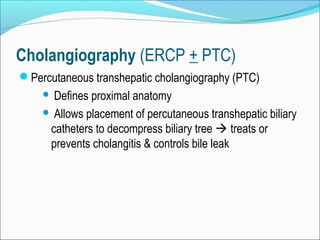
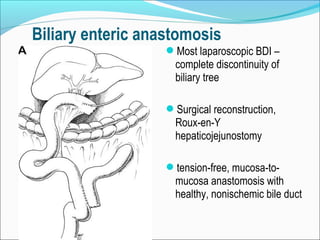
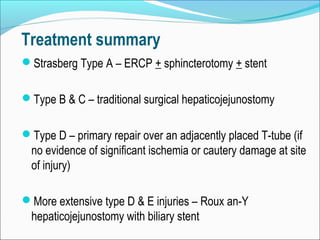
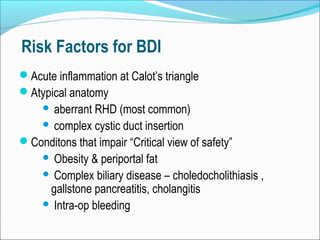
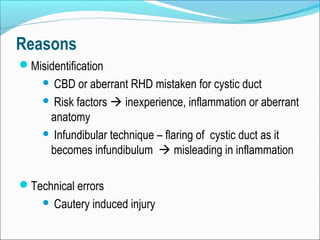
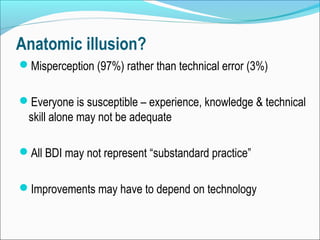
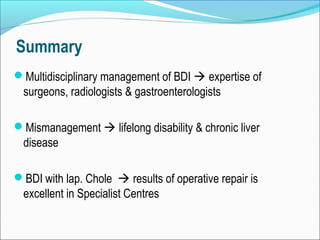
Bile duct injury is a rare but potentially devastating complication of cholecystectomy that can result in biliary peritonitis, sepsis, and cirrhosis. It is most commonly caused by misidentification of structures during laparoscopic cholecystectomy. Management involves controlling infection, delineating biliary anatomy, and reestablishing biliary drainage, usually through surgical hepaticojejunostomy. Prevention relies on identification of anatomical variations, achieving a "critical view of safety" before duct division, and open conversion if needed. Proper management requires a multidisciplinary approach between surgeons, radiologists, and gastroenterologists.