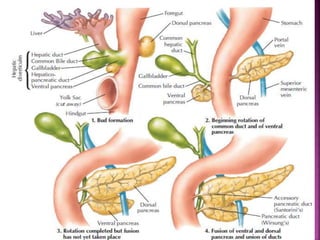
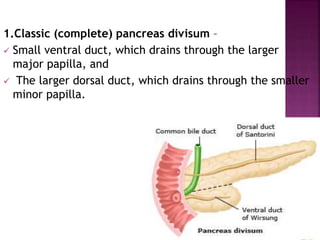
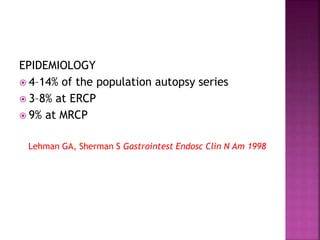
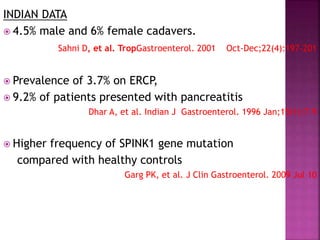
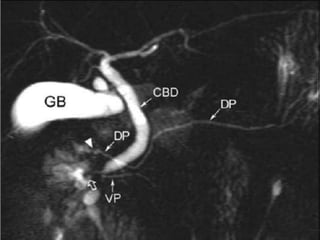
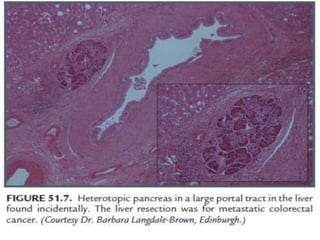
The document summarizes several pancreatic duct anomalies including pancreas divisum, annular pancreas, and ectopic pancreas. It describes the embryological development and classification of each anomaly. For pancreas divisum, it discusses diagnosis using ERCP, MRCP, or EUS and treatment options like endoscopic sphincterotomy or stenting of the dorsal duct. For annular pancreas, it describes the classification and presentations in infants versus adults. Surgical bypass is the preferred treatment. Ectopic pancreas most commonly involves the gastric antrum and is often asymptomatic.