Carcinoma gall bladder
- 2. Objectives: • Epidemiology • Etiology • Pathology and pathogenesis • Clinical presentation • diagnosis • Treatment • Prognosis
- 3. Epidemiology • 6500 cases annually (USA) • 5th most common cause of GI malignancy (USA) • Incidence increases with age • 2-6 times more common in female
- 4. Ca GB - distribution
- 5. Risk factors • Cholelithiasis – 75-98% of all patient with Ca GB – Cholesterols type stones • Old age • Female • Anomalous pancreaticobiliary duct junction • Typhoid carriers- chronic inflammation • Others- IBD
- 6. • The risk of developing gallbladder carcinoma increases directly with increasing gallstone size • Relative Risk =2.4 with stone size 2- 2.9cm diameter • Relative risk 10.1 with >3cm diameter stones
- 7. Lahmar A, Abid SB, Arfa MN, Bayar R, Khalfallah MT, Mzabi-Regaya S. Metachronous cancer of gallbladder and pancreas with pancreatobiliary maljunction. World Journal of Gastrointestinal Surgery. 2010;2(4):143-146. doi:10.4240/wjgs.v2.i4.143. • Anomalous pancreaticobiliary duct junction • with an incidence of 3.2% in patients undergoing ERCP or operative Cholangiopancreatography
- 8. • Refluxed proteolytic pancreatic enzymes are activated in the biliary tract and may induce biliary tract carcinoma • The reflux of bile may activate pancreatic enzymes which may cause chronic inflammation and metaplastic epithelial change in the pancreatic duct and pancreatic cancer may eventually develop
- 9. Etiology • Gall stones and chronic inflammation • 3.3 to 3% among patients with GSD • Porcelain GB (10-25%) • Helicobacter bilis and Helicobacter pylori (about six fold higher risk) • Chemicals methyldopa,oral contraceptives, isoniazid, and occupational exposure in the rubber
- 10. Anatomic consideration • The location of the primary tumor within the gallbladder and the proximity of the portal vein, hepatic artery, and bile duct are all important factors in the surgical management of this tumor
- 11. • The gallbladder is attached to segments IVb and V of the liver and these segments are involved early in tumors of the fundus and body of the gallbladder- limited segmental resection often possible
- 12. • Tumors of the infundibulum or cystic duct readily obstruct the common bile duct and may involve the portal vein. • As with cholangiocarcinoma the tumor may be unresectable early in its course-- tumor of this region require extended liver resections due to proximity to portal pedicles
- 13. Pathology • GB epithelium progresses from dysplasia to carcinoma in situ to invasive carcinoma • Area of dysplasia and carcinoma in situ is often missed in routine cholecystectomy specimens as there are no associated gross characteristics that would target an area for histological sections • Carcinoma in situ may appear within the Rokitansky aschoff sinuses and often mistaken for invasive carcinoma
- 14. • Rate of progression of precursor lesions to invasive carcinoma has estimated around 15 years
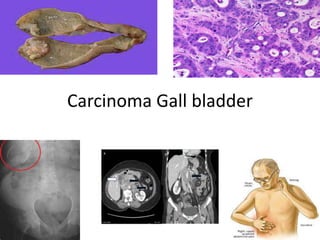
- 15. Gross
- 16. Gross morphology • Difficult to diffrentiate grossly from chronic cholecystitis at early stages and are often found incidentally on pathologic sections • 60% - fundus • 30% body • 10% neck
- 17. • Tumor arising from neck and hartmanns pouch may infiltrate the cystic duct and common bile duct make it clinically indistinguishable form hilar bile ducts tumor
- 18. 1. Infiltrative- m/c 2. Nodular 3. Combined nodular- infiltrative- m/c 4. Papillary 5. Combined papillary- infiltrative
- 19. • Infiltrative tumors cause thickening and indurations of GB wall and extending to entire GB • Spreads in the subserosal plane which is the same as the surgical plane used for routine cholecystectomy if tumor unrecognized during surgery leads to regional dissemination • Becomes more advanced if infiltrates liver
- 20. • Nodular type – Early invasion through GB wall into liver or neighboring structures – Easier to control surgically than infiltrative whose margins are less defined
- 21. • Papillary ca – exhibit a polypoid or cauliflower like appearance – Better prognosis – May be larger filling the lumen but with minimal invasion
- 22. • Histopathological grading – G1- well differentiated – G3- undifferentiated – Majority of patient present with G3 poorly differentiated tumors
- 23. Tumor bilogy • Multiple genetic changes • P53 and k-ras gene mutation
- 24. Pattern of spread • Along peritoneal cavity • Along needle biopsy sites • Laparoscopic port sites
- 25. • direct extension to liver and other adjacent organs – Gall bladder has thin wall, narrow lamina propia, and single muscle layer – Once penetrates to thin muscle layer has access to major lymphatic and vascular channels
- 26. • tumor penetration into or through the muscularis has prognostic implications because the lymphatic drainage of the gallbladder lies in the layer between the muscle and the serosa. • Also, most simple cholecystectomies for gallstone leave the serosa on the liver side because the subserosal plane is the easiest for dissection. • Thus, simple cholecystectomies performed for unsuspected gallbladder cancer is likely to leave a positive margin for any tumor that penetrates the muscle layer
- 27. • Autospy • 94.4% lymphatic mets • 64.% hematogenous dissemination • Hematogenous form small veins extensding directly from gall bladder to portal venous system of GB fossa leading to segment IV and V of liver or via larger veins to portal venous branch of segment V and VIII
- 30. 1-pericholedochal, nodes along the common bile duct 2- cystic duct, node(s) along the cystic duct 3-retroportal, nodes posterior to the portal vein and cephalad to the uncinate process 4-posterior superior pancreaticoduodenal, nodes on the posterosuperior aspect of the head of the pancreas
- 31. 5-hepatic artery, nodes along the common or proper hepatic artery 6-right celiac, nodes located right of the celiac axis and posterior to the common hepatic artery 7-hilar, nodes within the porta hepatis
- 32. Radiologic investigation Discontinious GB mucosa Echogenic mucosa Submucosal echolucency Inhomogenous mass replacing all or part of GB Diffuse thickening of GB wall Lypmh nodes- a soft tissue mass with AP diameter of atleast 10mm showing ring like heterogenous enhancement ( 89% accuracy) Positive LN may alter surgeons decisions to operate or change operative approach
- 33. MRCP • More detail information than CT sccan and Usg • Angiography – Portal vein and hepatic artery encasement avoids unneccesay laparotomy • EUS – Peripancreatic and periportal adenotpathy – Needle bipdy can be performed
- 34. • Endoscopic and percutaneous cholangiographs – GB cancer with obstructive jaundice- direct invasion or compression of CHD or by pericholedochal LN – Intraheptic bile ducts obstruction. High ALP – Planning of palliative managemt of Gall bladder carcinoma – Also indicated in atypical cases with vague sypmtoms and abnormal lft where other imaging modalities have not yeilded diagnosis – Stricturing, distortion or nonfiling of bile ducts draining segment IV and V with no effects on other segmental ducts
- 35. • Biliary colic or chronic cholecystitis, elderly patients with atypical symptoms, suspicious lab findings ( anemia, hypoalbunemnia or abnormal LFT) • USG- mnass, abnormal mucosal finnding, or segmental duct dilatation • CT scan • Lab or radiologic investigation shows evidence for ductal obstructionMRCP, ERCP or PTC • Advanced mass encroaching on the porta hepatis duplex USG or arteriography
- 36. Preop pathologic diagnosis • Suscpicious mass- pre op biopsy contoversial • Cholec( ystectomy as diagnositic biopsy unaccesptale • ERCP and bile cytology (73% sensitivity) • Percutaneous FNAC- mass not considered for surgical resection ( 88% accuracy) • Percutaneous core needle biospy if FNAC fails as high chance of needle tract seeding
- 37. staging 1. Modified Nevin system ( Donohue et.a l 1990, Nevin et. al 1976) 2. Japanese Biliary Surgical Society system (Onoyama et al 1995) 3. AJCC/UICC TNM staging system ( Beahrs and Myers 1983)
- 39. management • Stage O and Stage I ( Tis, T1a – Ca invades lamina propia but don’t extend to muscularis) • frequently detected on pathological examination • Imaging based staging • Watch cholecystectomy specimen to ensure negative margin
- 40. Margin postive • No evidence of residual or metastatic GB ca • But cystic duct margin positive • Rexploration with CBD excision , regional lymphadenectomy and HJ Margin negative,negative imaging • No further surgery
- 41. • Stage T1b ( cancer that invases the muscularis but don’t extend to perimusccular connective tissue • T1 b cancer treat same as T2 Ca GB
- 42. Stage II ( T2NOMO) • T2- cancer invasion into perimuscular connectivetissue of GB • regional LN mets- 28-63% • Rexploration with liver resection and regional lymphadenectomy of hepatoduodenal ligament
- 43. • Preoperative T2 suscpicious • staging • In no contraindication • Proceed for exploration with en bloc resection of GB and adjacent liver to depth of at least 2 cm with regional lymphadenectomy of hepatoduodenal ligament • Non anatomic • Anatomic segment 4b, 5 resection – less bleeding
- 44. Stage III • T3 lesions ( locally advanced cancers that perforate the GB serosa or directly invade the liver and/ or one adjacent organ and • T1-T3 lesions associated with regional LN mets
- 45. Stage III • Careful planning,individualized • Liver invasion- hepatic resection seg 4b and 5 – Trisegmentectomy if GB foss bridges both right and left hepatic lobes – Enbloc resection of hepatic flexure of colon – Long term survival- 15-63%
- 46. Stage IV • IV A-Invasion to main portal vein, common hepatic artery, multiple extrahepatic organs • Stage IVB – N2 and or distance mets – Uresectable – Main portal vein, CHA if reseccted – confers morbidity and mortality ares
- 47. Adjuvant therapies • Adjuvant chemoradiotherapy after resection • External beam or intraoperative radiation therapy alone or in combination with 5FU- decreasse local recurrence • Data inadequate
- 48. palliation • Goal- relief pain, manifestation of biliary obstruction ( pruritis and cholangitis) and bowel obstruction • Endscopic stenting than surgical bypass in weeks to month survival • Palliative radiotherapy • Regional intra- arterial chemotherapy andchemoradiotherapy • Gemcitabine plus cisplantin
- 49. outcome Five year survival % T1N0 39 T2N0 15 T3N0 12
- 50. • T1- 85-100% • with radical resection- – T2 80-90% – T3 15-63% – T4 2-25%
- 51. • Radical resection of node positive- 60% 5 year survival
- 52. – Morbidity and mortality – Morbidity--5-54% – Mortality- 0-21% – More the extensive dissection more morbidity and mortalitiy rates
- 53. CT • GB cancer protocol • Dual phase contrast – arterial and venous
Editor's Notes
- Intralumminal mass with soft tissue enhancing
- Gb can with diffuse wall thick, hyperemic wall as cholecystitis, irregularity of wall and mucosal enhancement
- unresectable
- Focal wall thickening with enhancement, lost plane between GB and liver
