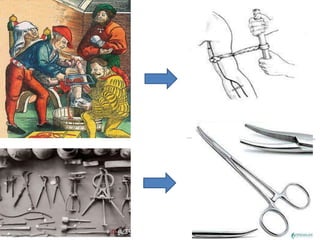
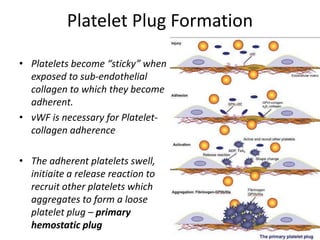
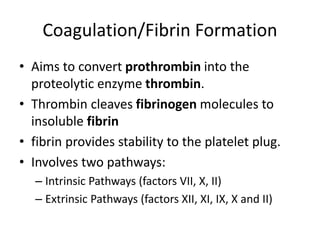
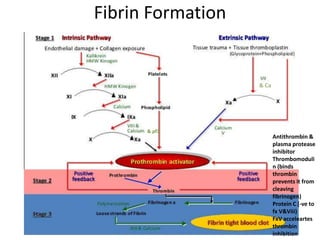
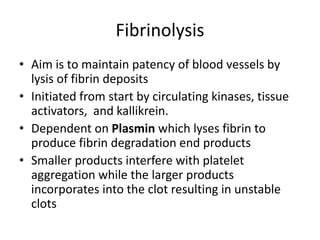
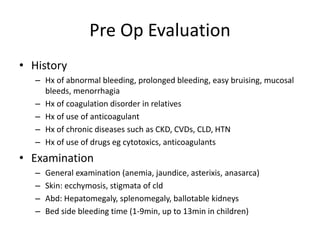
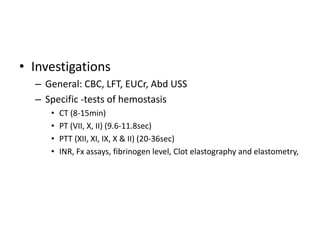
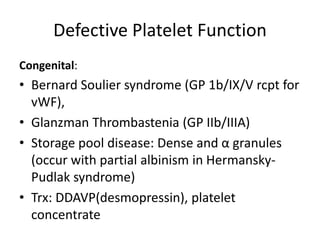
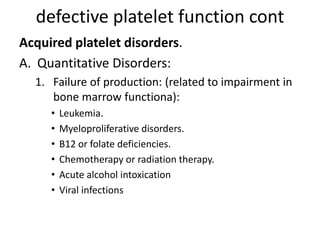
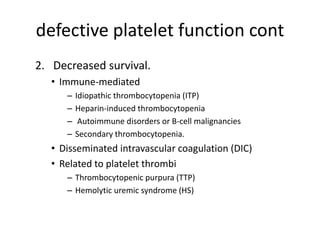
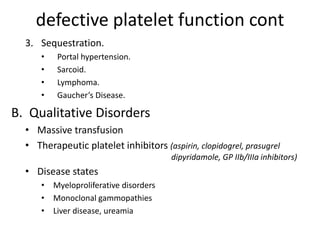
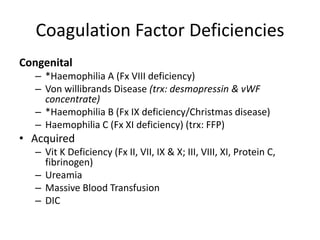
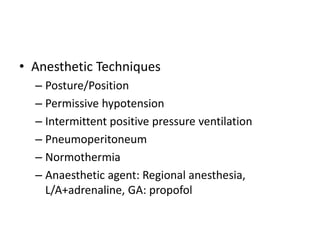
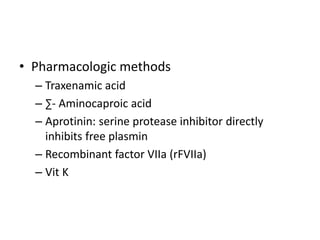
The document outlines the critical role of hemostasis in surgery, detailing its definition, significance, and underlying physiology, including vasoconstriction, platelet plug formation, and coagulation. It discusses management strategies for hemorrhage in surgical patients, covering preoperative evaluation, intraoperative techniques, and postoperative care. The importance of addressing hemostatic defects, both congenital and acquired, is emphasized to prevent complications during surgical interventions.