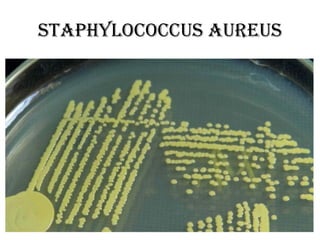
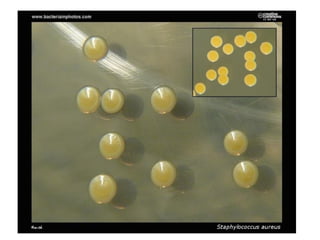
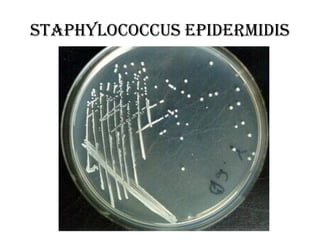
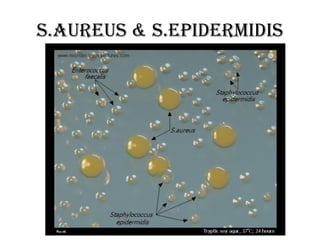
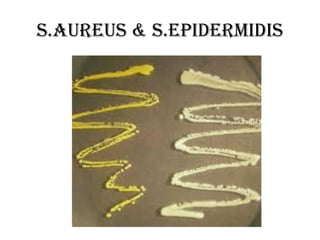
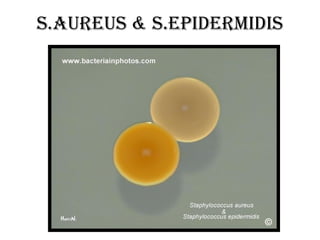
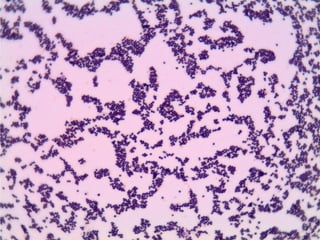
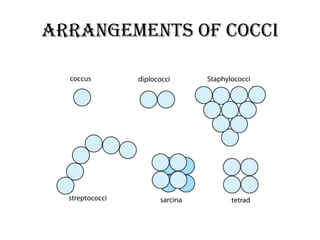
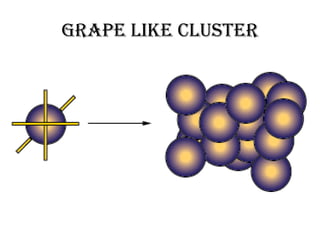
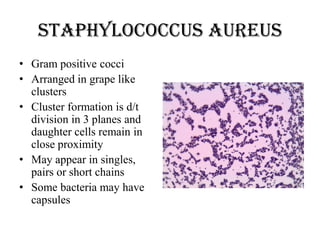
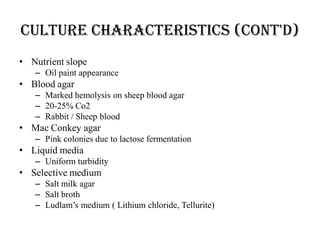
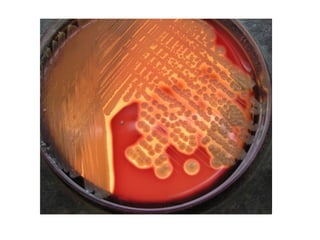
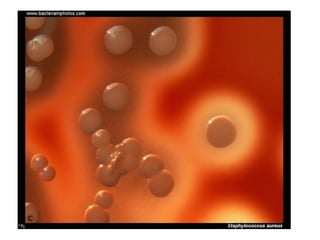
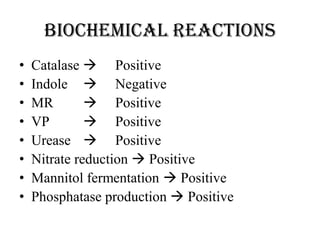
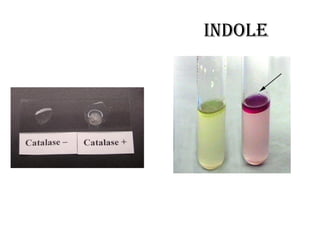
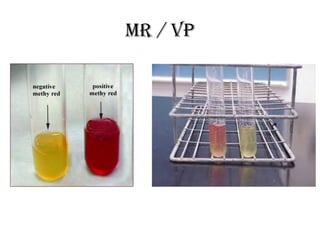
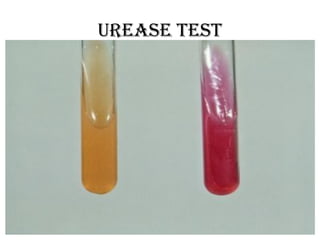
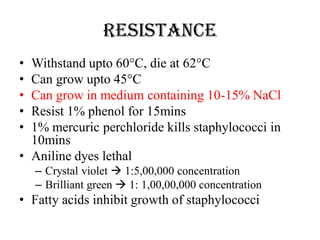
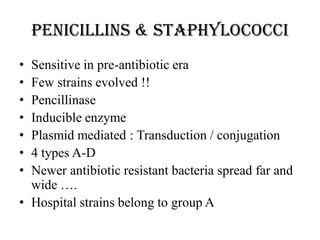
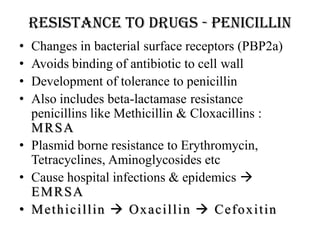
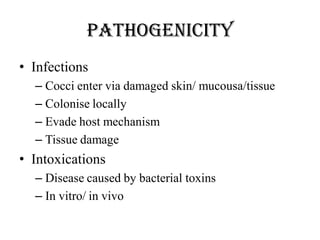
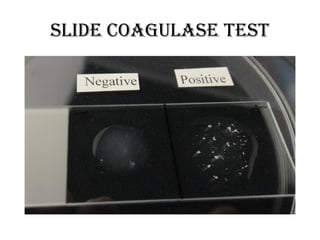
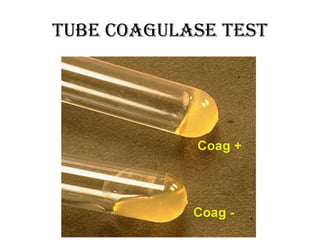
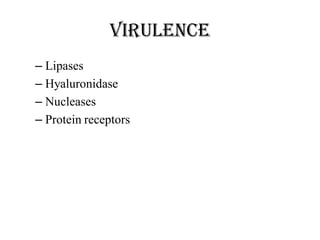
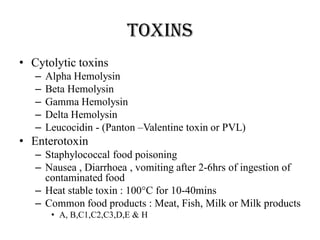
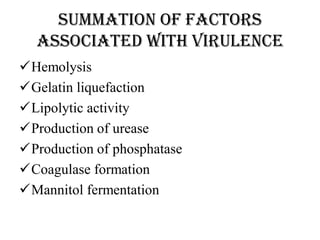
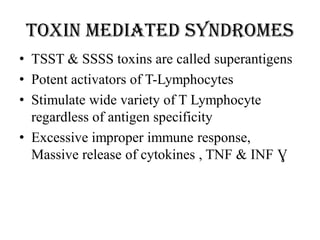
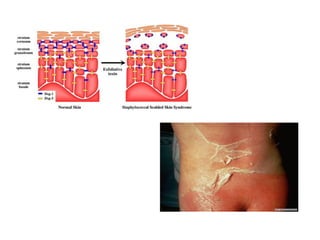
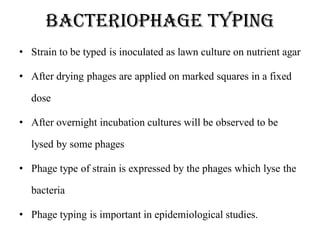
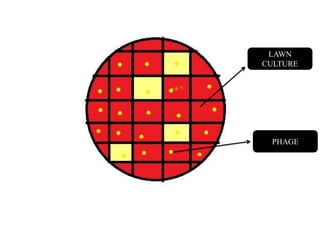
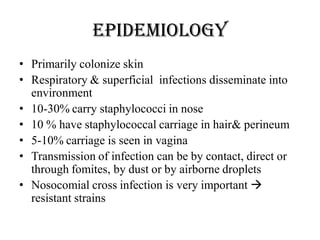
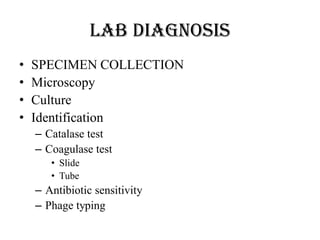
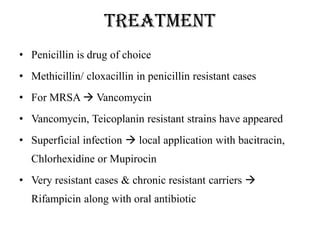
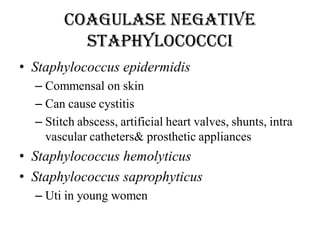
The document provides an in-depth overview of the Staphylococcus genus, highlighting its characteristics, pathogenicity, and the related infections caused by various species such as Staphylococcus aureus and Staphylococcus epidermidis. It discusses their culture characteristics, resistance to antibiotics, virulence factors, and the clinical significance of staphylococcal diseases ranging from skin infections to systemic conditions. Additionally, the document addresses the methods of laboratory diagnosis and treatment options for staphylococcal infections, emphasizing the rise of antibiotic resistance in hospital strains.