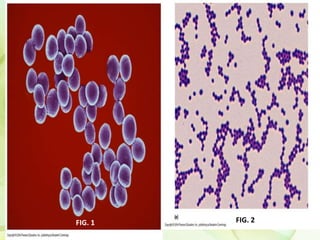
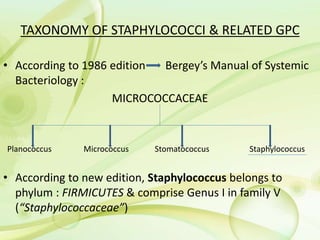
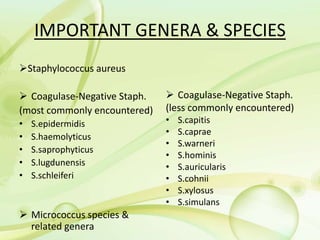
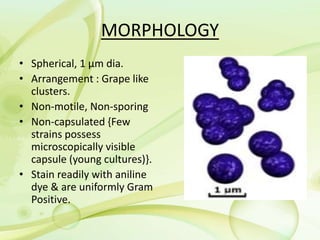
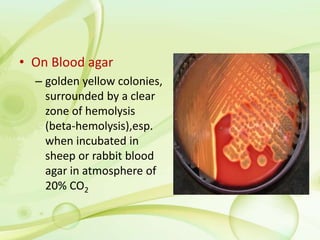
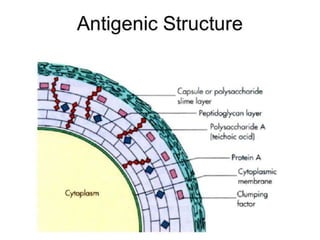
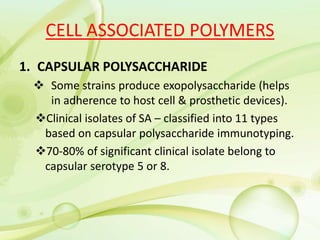
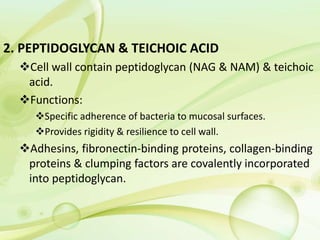
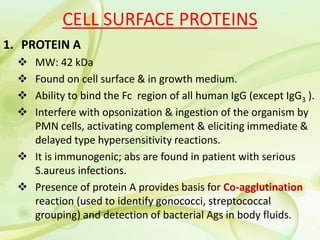
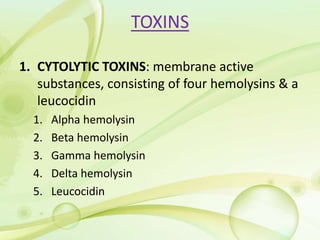
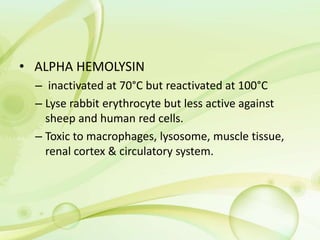
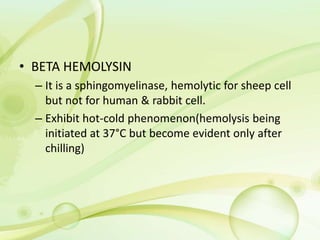
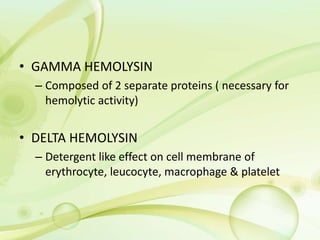
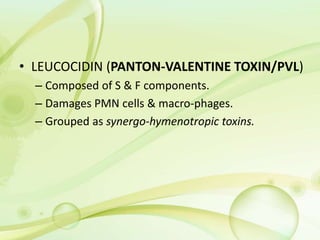
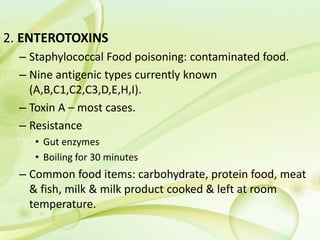
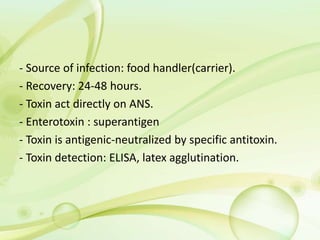
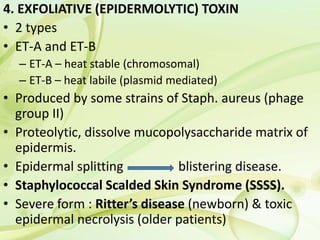
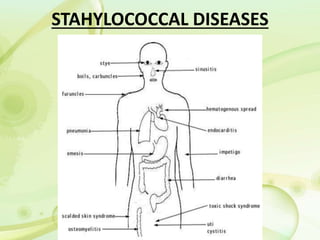
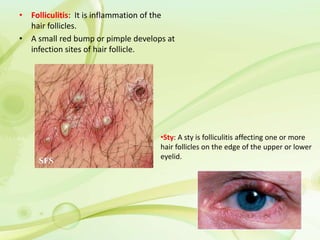
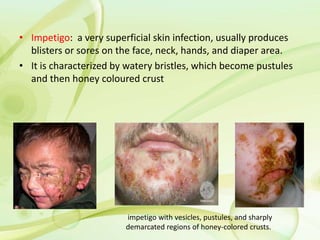
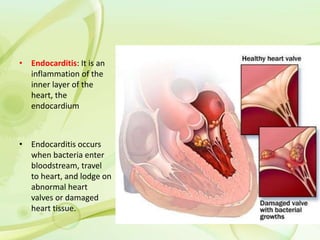
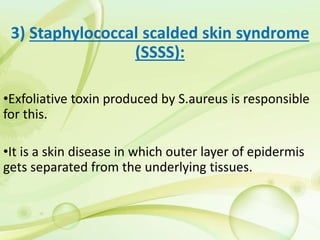
Staphylococcus is a genus of gram-positive bacteria that can cause a variety of infections and diseases in humans and other animals. Staphylococcus aureus is one of the most important species due to its ability to cause serious infections such as pneumonia, meningitis, endocarditis, toxic shock syndrome, and food poisoning. It produces several virulence factors like coagulase, hemolysins, enterotoxins and exotoxins that enable it to evade host defenses and cause tissue damage. Common diseases include skin and soft tissue infections like impetigo, folliculitis, boils; respiratory infections; food poisoning caused by enterotoxins; and toxic shock syndrome caused by toxic