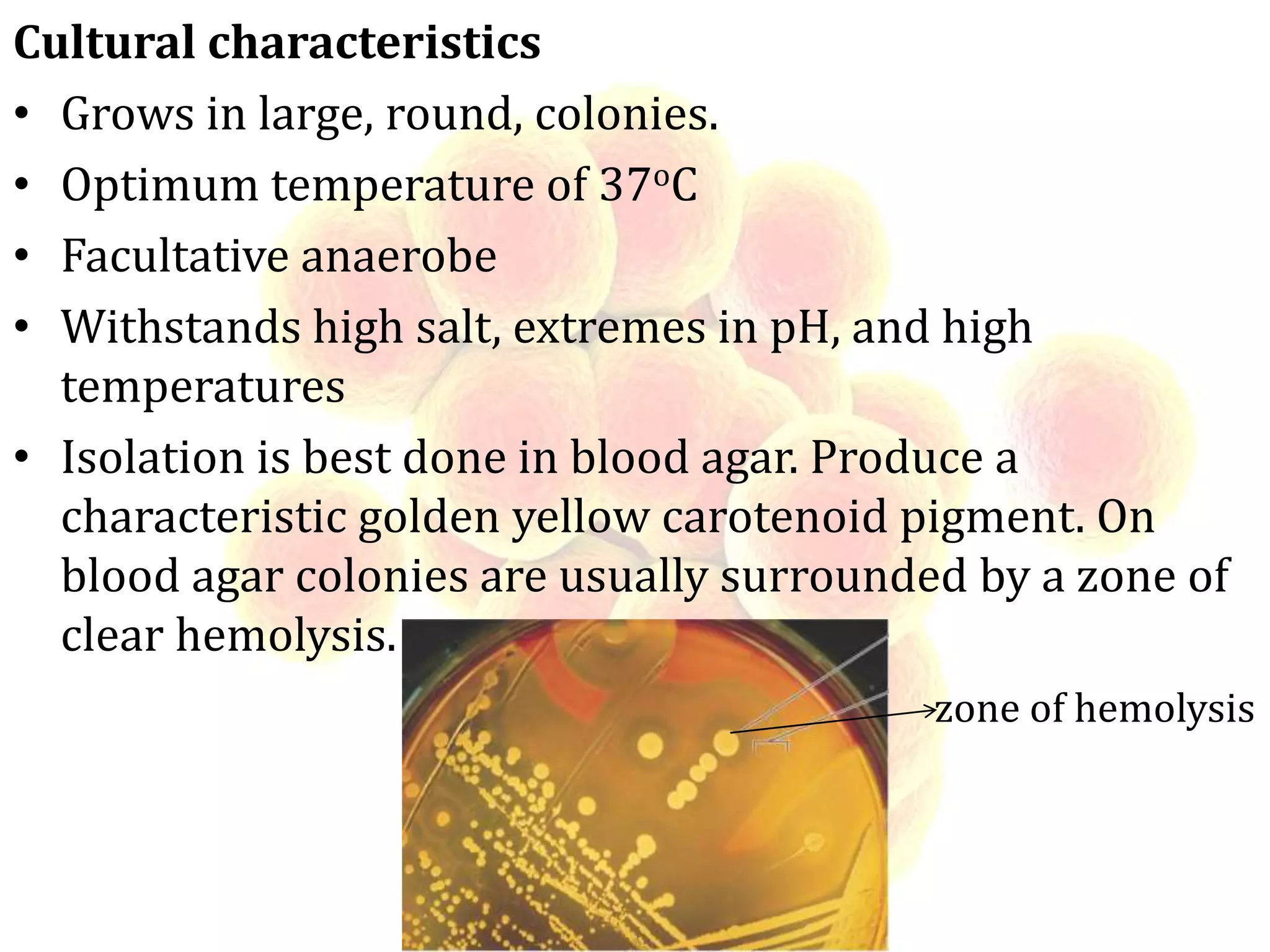
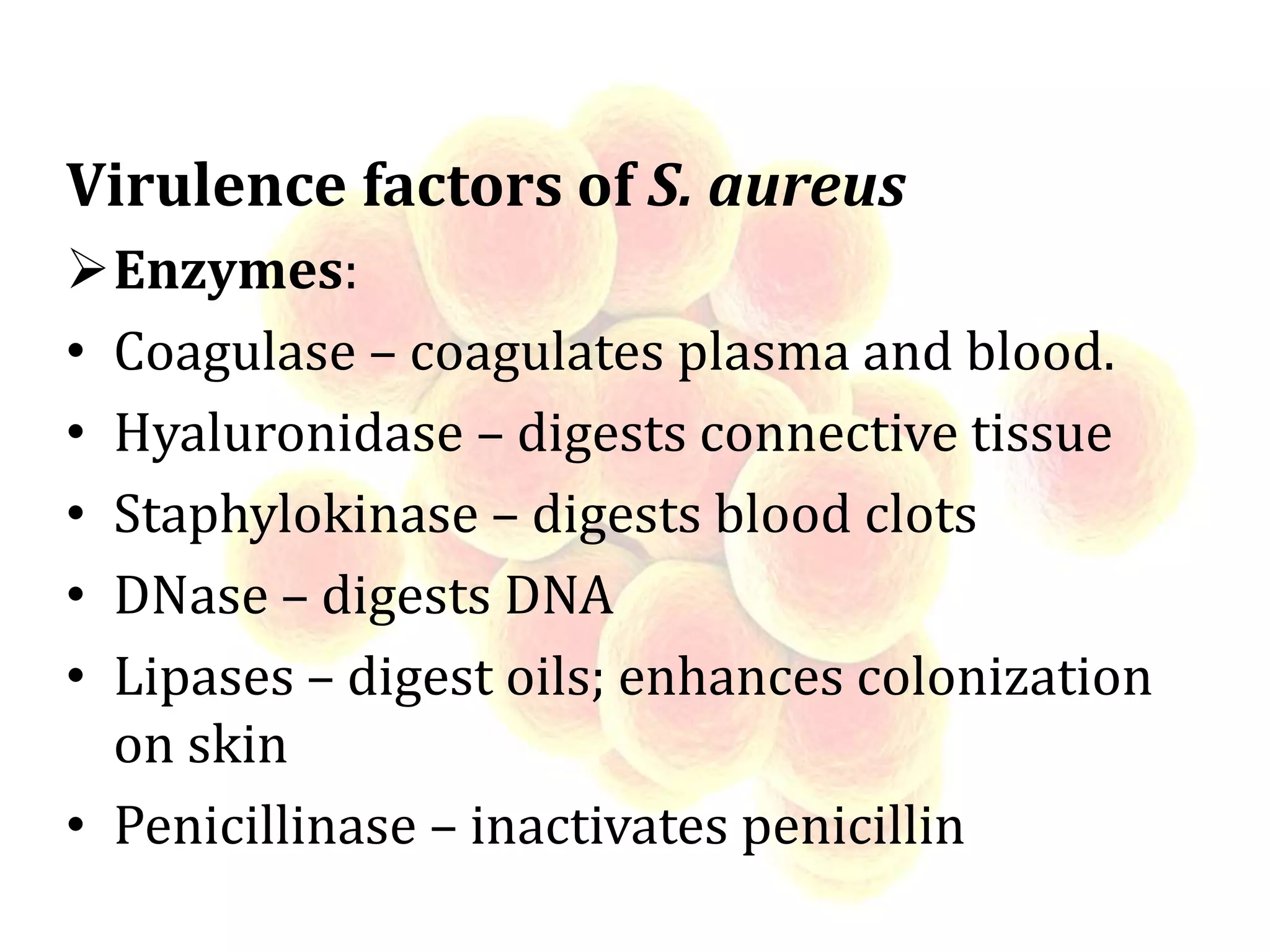
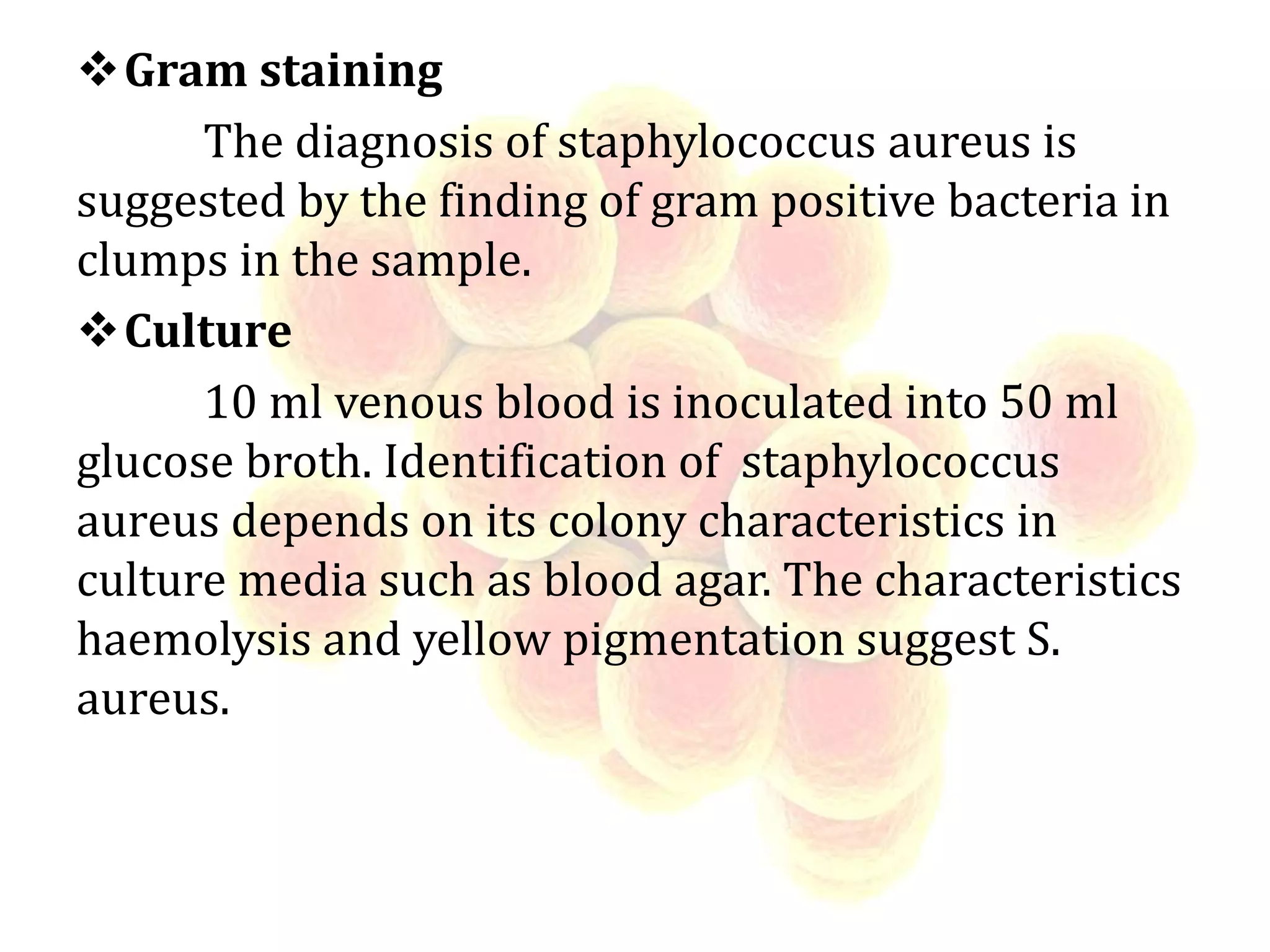
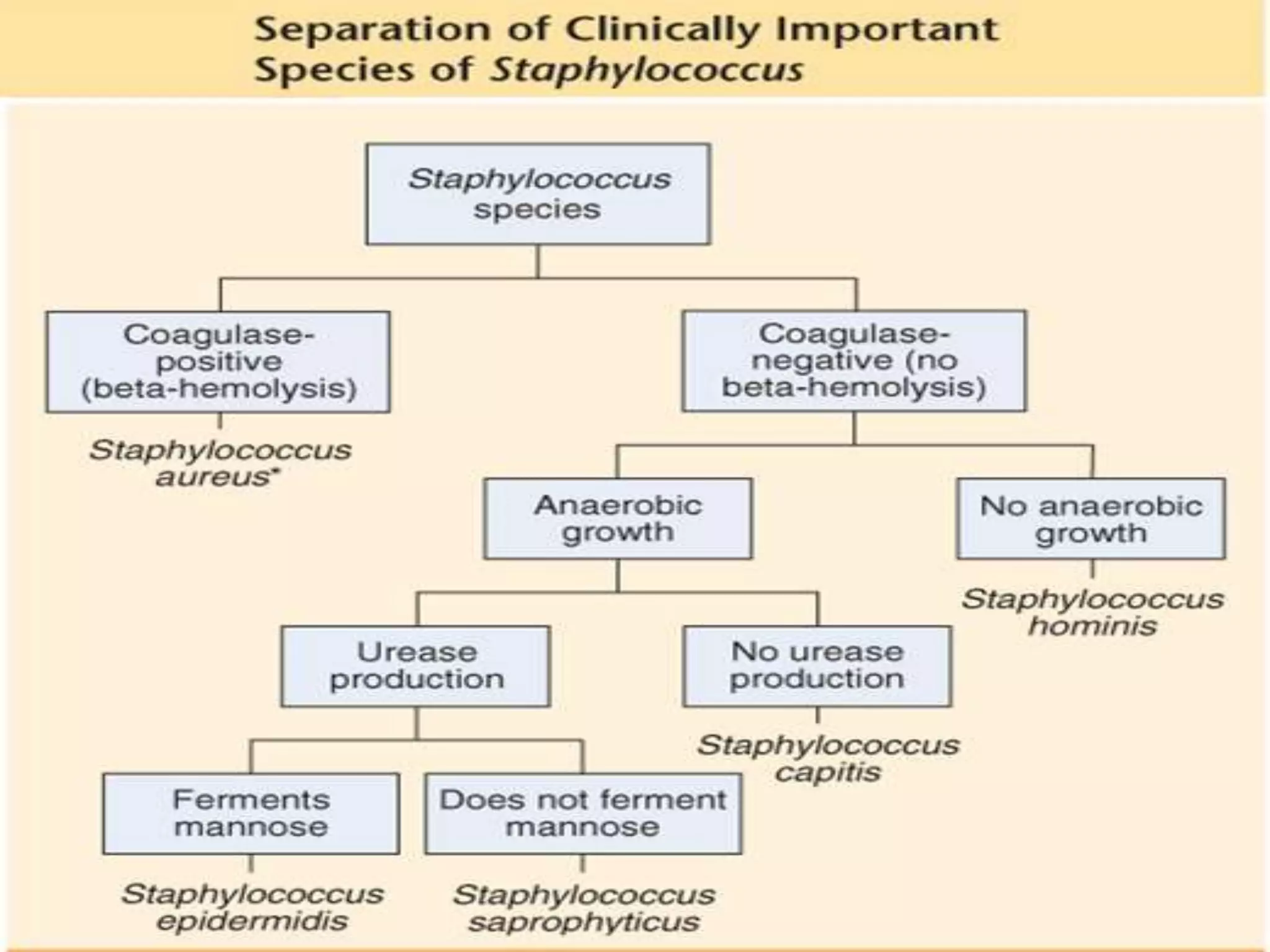
This document discusses Staphylococcus, including S. aureus. It describes the morphology and cultural characteristics of S. aureus, noting it is a gram-positive coccus that grows in clusters and produces golden yellow pigment on blood agar. S. aureus can cause a variety of infections through production of enzymes and toxins. Laboratory diagnosis involves gram staining, culturing, and coagulase testing of samples. Treatment often involves cephalosporins due to high resistance of S. aureus to penicillin.