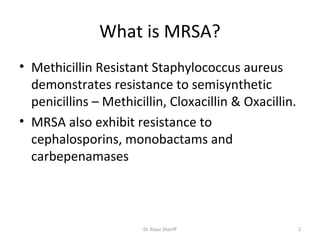
Methicillin resistant Staphylococcus aureus (MRSA) demonstrates resistance to methicillin and other beta-lactam antibiotics. There are two main types - hospital associated MRSA (HA-MRSA) which circulates in healthcare facilities, and community associated MRSA (CA-MRSA) which is found in the community without recent healthcare exposure. CA-MRSA strains first emerged in the 1990s and seem to have evolved from MSSA by acquiring small SCCmec cassettes. While usually associated with community infections, some studies have found that CA-MRSA strains can also cause healthcare-associated infections.