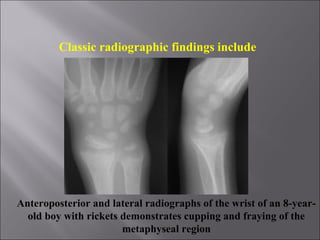
Rickets is a childhood bone disease caused by vitamin D deficiency and a lack of calcium and phosphate. It results in soft, weak bones that can lead to skeletal deformities. The disease develops when vitamin D levels are too low to absorb calcium and phosphate from the intestines, causing these minerals to be lost from the bones. Symptoms include bowed legs, soft skull, and bone pain. Diagnosis involves blood tests showing low calcium and vitamin D levels and high alkaline phosphatase. X-rays show widened growth plates and fraying and cupping of the bone. Treatment involves high dose vitamin D and calcium supplementation to strengthen the bones.