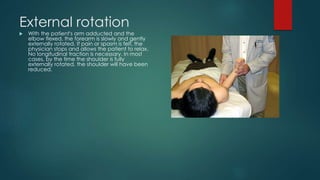
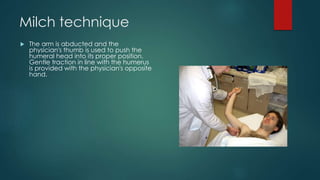
Shoulder dislocations have been documented as far back as ancient Egypt. The most common type is anterior dislocation, which accounts for 60% of cases. Reduction techniques described include external rotation, scapular manipulation, Milch, Stimson, traction-countertraction, and Spaso. Post-reduction, most patients are immobilized for 3 weeks if under 30 or begin mobilization after 1 week if over 30. Recurrent dislocation is a major complication, seen in 50-90% of patients under 20.