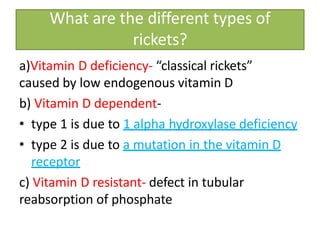
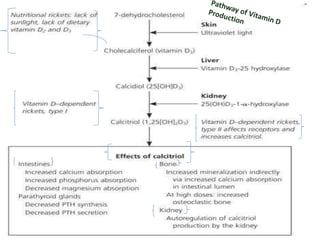
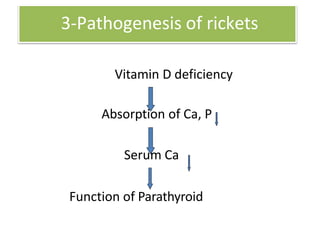
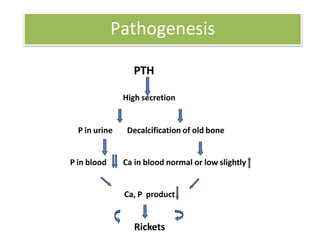
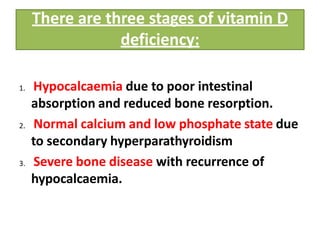
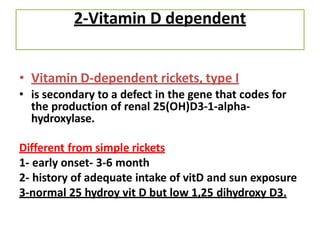
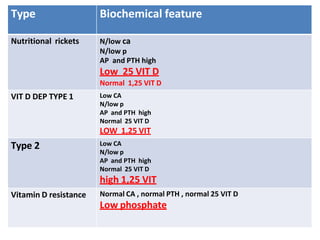
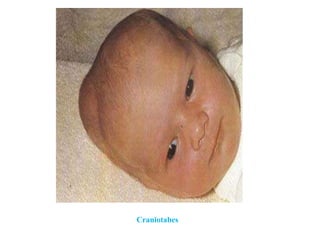
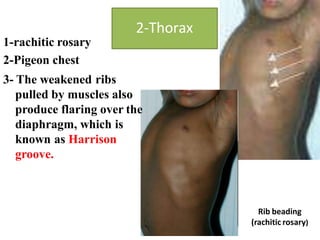
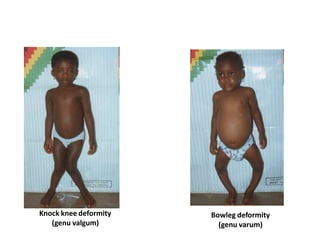
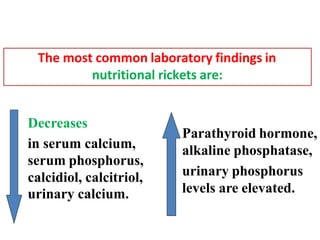
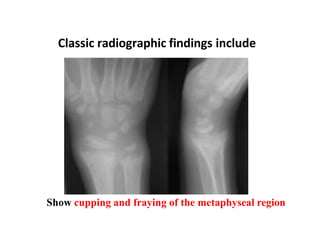
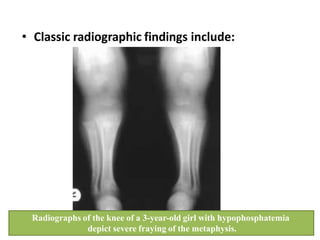
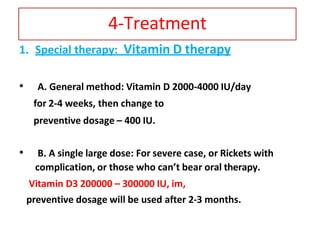
Rickets is a childhood bone disease caused by vitamin D deficiency and impaired bone mineralization. The main types are nutritional rickets from inadequate vitamin D, calcium, or phosphate intake and vitamin D-dependent rickets caused by genetic defects. Physical exam findings include bone tenderness, bowed legs, and chest deformities. Laboratory tests show low calcium, phosphate, and vitamin D levels with elevated alkaline phosphatase and parathyroid hormone. X-rays demonstrate widened growth plates and fraying of bone. Treatment involves high dose vitamin D supplementation with calcium and phosphate as needed.