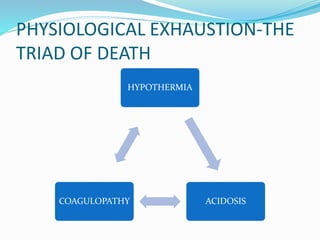
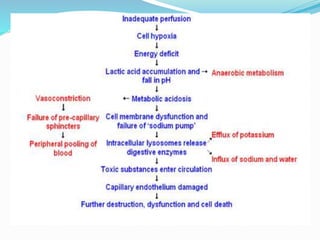
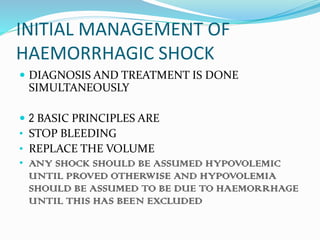
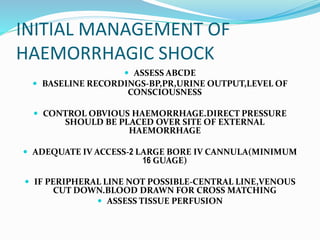
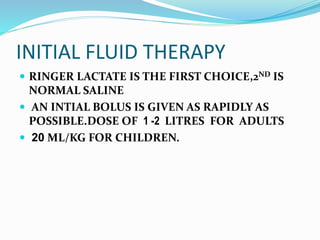
Shock is a circulatory system abnormality resulting in inadequate oxygen perfusion and tissue oxygenation. The physiological triad of death in shock is hypothermia, acidosis, and coagulopathy. In hypoperfusion states, cellular anaerobic metabolism leads to lactic acidosis and decreased coagulation protease function, causing coagulopathy and further hemorrhage. Underperfused muscle cannot generate heat, leading to hypothermia, which further impairs coagulation and causes a downward spiral to physiological exhaustion and death. There are various types of shock including hypovolemic, cardiogenic, obstructive, and distributive shock. Initial management of hemorrhagic shock involves stopping bleeding, restoring volume with
![SEPTIC SHOCK
Severe sepsis with cardiovascular organ dysfunction,
i.e. hypotension (systolic blood pressure [SBP] < 5th
centile
non-specific systemic inflammatory response to
infection,trauma, burns, surgery etc.
Characterized by abnormalities in 2 or more of the
following • body temperature• heart rate• respiratory
function
• peripheral leucocyte count](https://image.slidesharecdn.com/shock-140504010055-phpapp01/85/Shock-33-320.jpg)