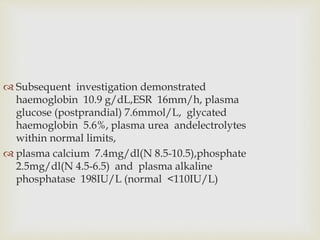
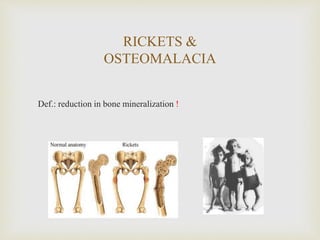
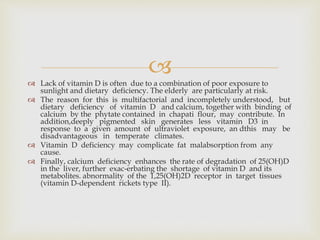
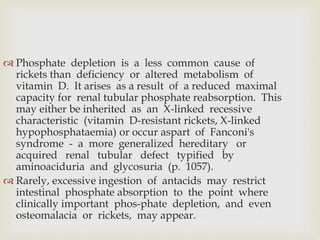
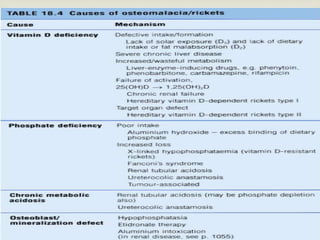
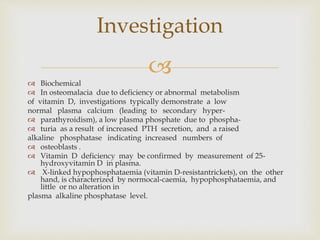
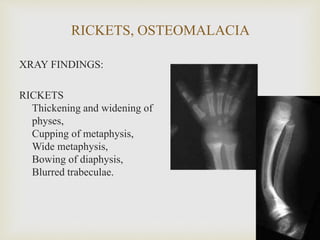
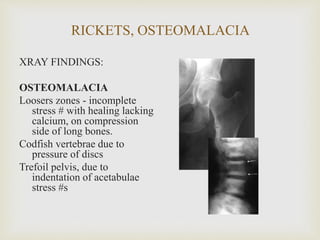
A 40-year-old male presented with 4 months of generalized muscle discomfort, particularly in the shoulders, without relief. Examination showed mild weakness in arms and legs but normal reflexes. Tests revealed low calcium and phosphate levels and high alkaline phosphatase, suggestive of osteomalacia. Osteomalacia is a condition characterized by reduced bone mineralization due to vitamin D deficiency, phosphate depletion, or metabolic acidosis. This patient's presentation and test results indicate osteomalacia likely due to vitamin D deficiency.