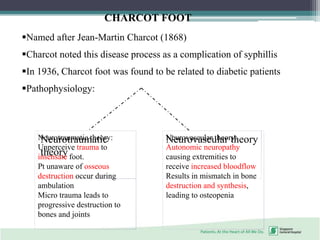
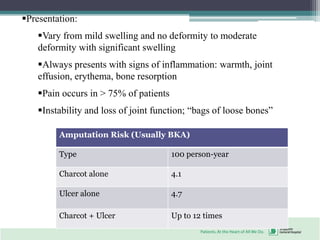
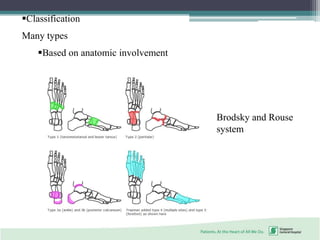
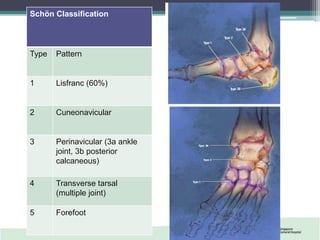
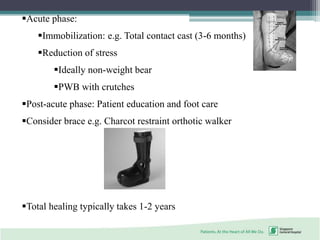
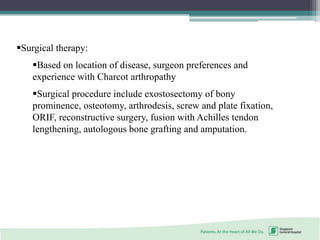
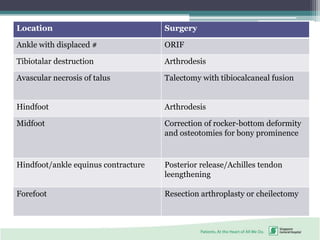
This document discusses Charcot foot, also known as neuropathic foot, which is a condition where repetitive stress causes destruction of bones and joints in the foot. It primarily affects those with nerve damage from conditions like diabetes, syphilis, tabes dorsalis, and leprosy. Charcot foot was first described by Jean-Martin Charcot in 1868. Physical findings include swelling, deformity, warmth, and bone resorption. Treatment involves immobilization in the acute phase to reduce stress, and bracing or surgery in the post-acute phase depending on the location and severity of damage. The document also briefly discusses the risks and management of diabetic foot complications.