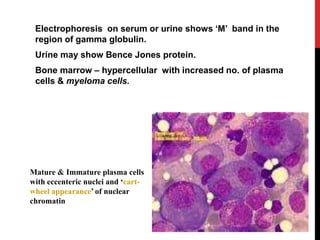
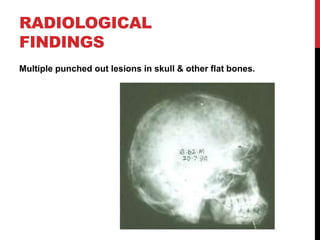
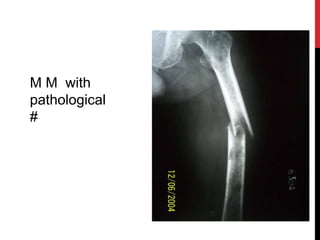
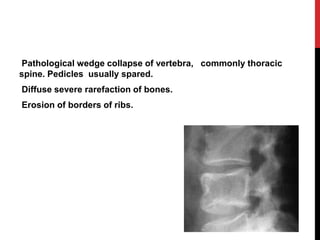
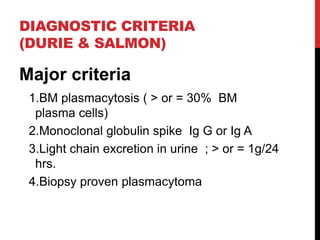
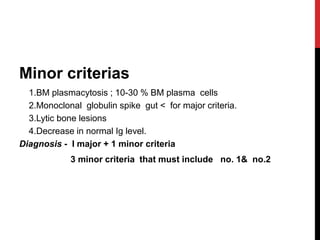
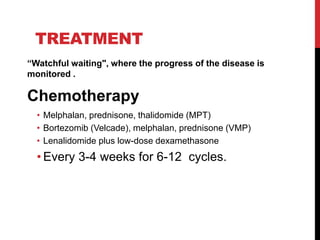
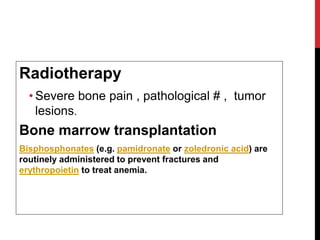
Multiple myeloma is a malignant clonal proliferation of plasma cells in the bone marrow that causes lytic bone lesions. It most commonly affects people aged 50-60 and is more common in men. Symptoms include bone pain, pathological fractures, fatigue, and susceptibility to infection. Investigations show anemia, elevated proteins, monoclonal band, and bone marrow plasmacytosis. Treatment involves chemotherapy, radiotherapy, stem cell transplant, and bisphosphonates to manage complications and extend survival to 2-3 years.