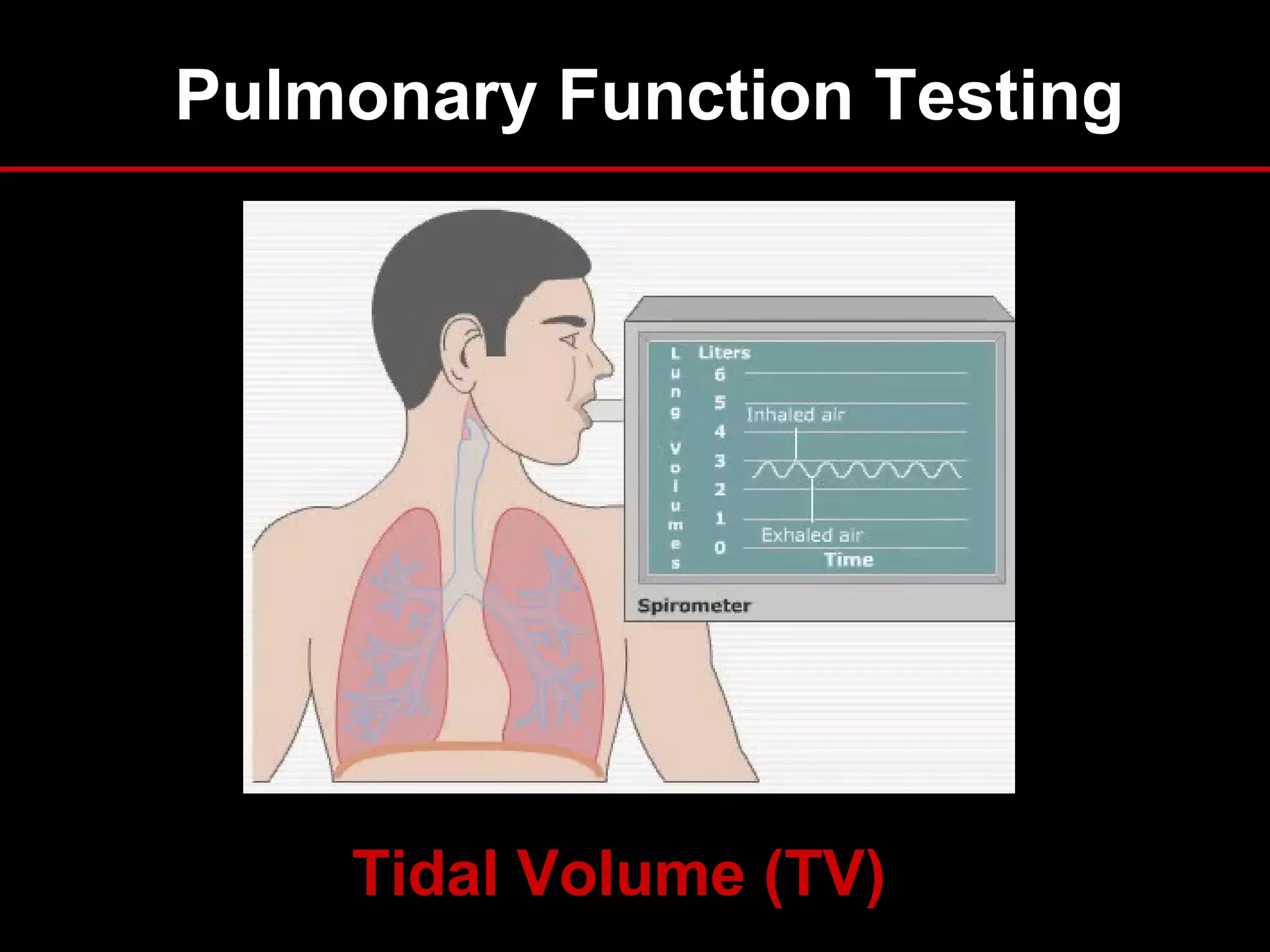
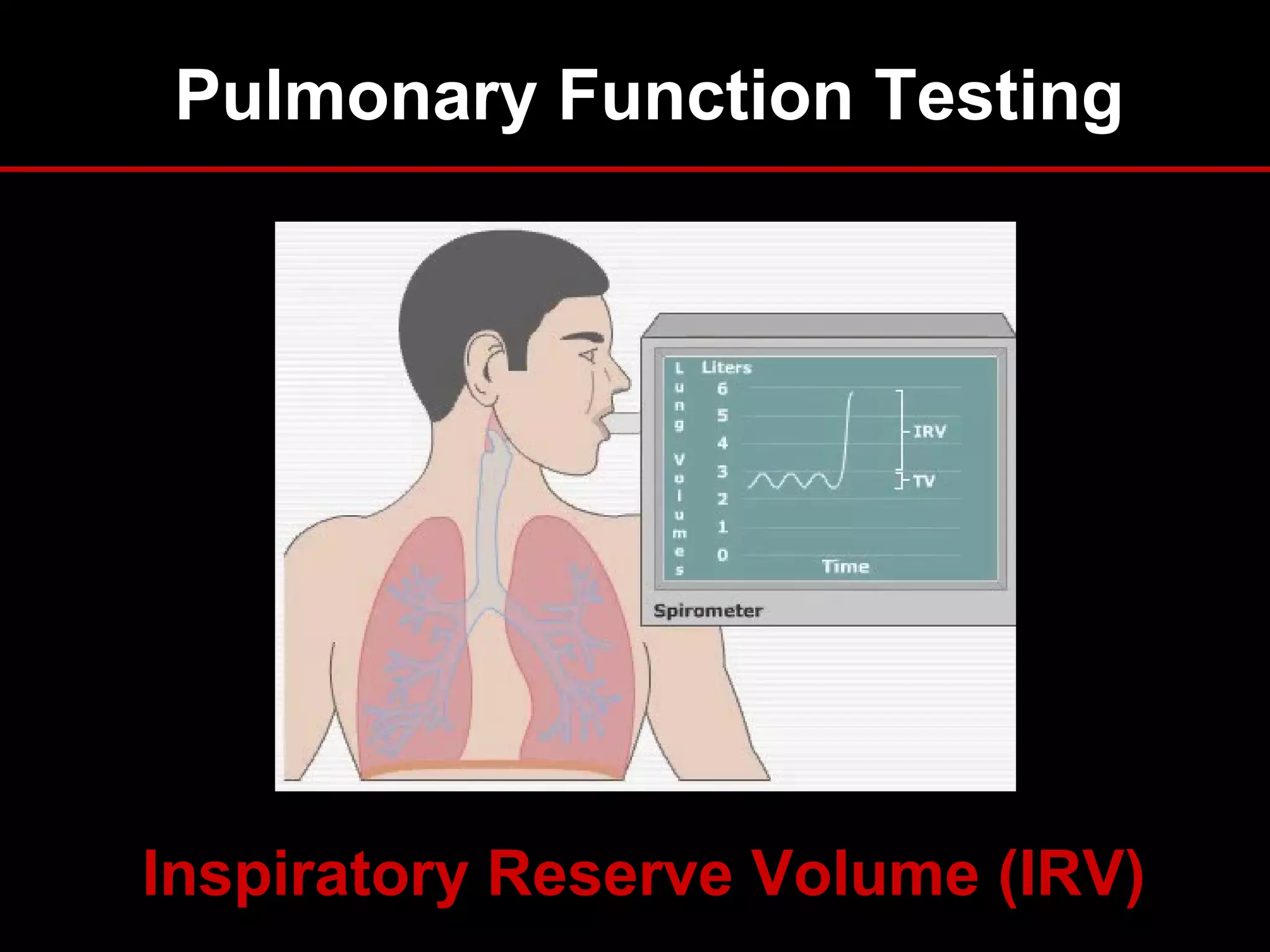
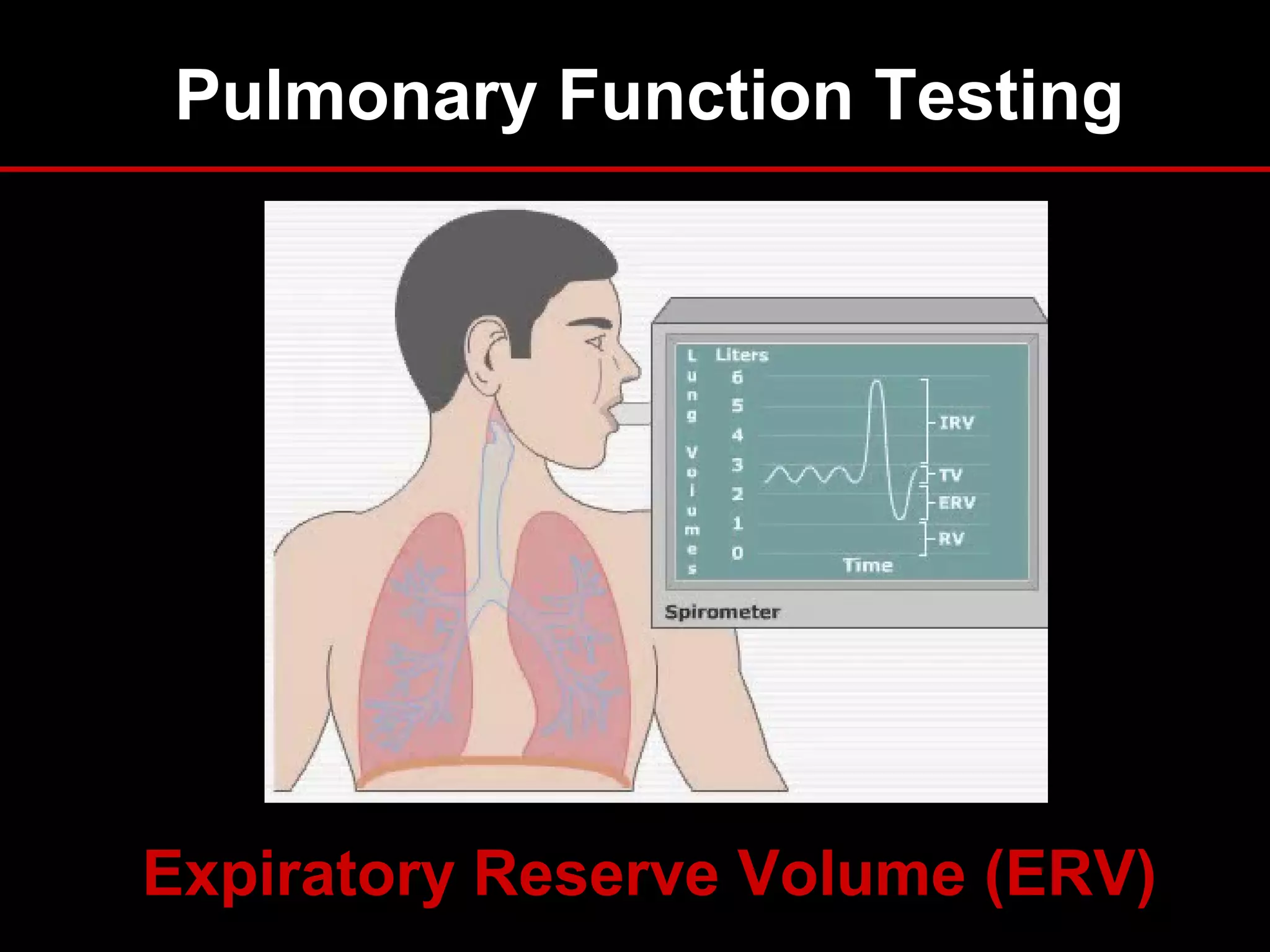
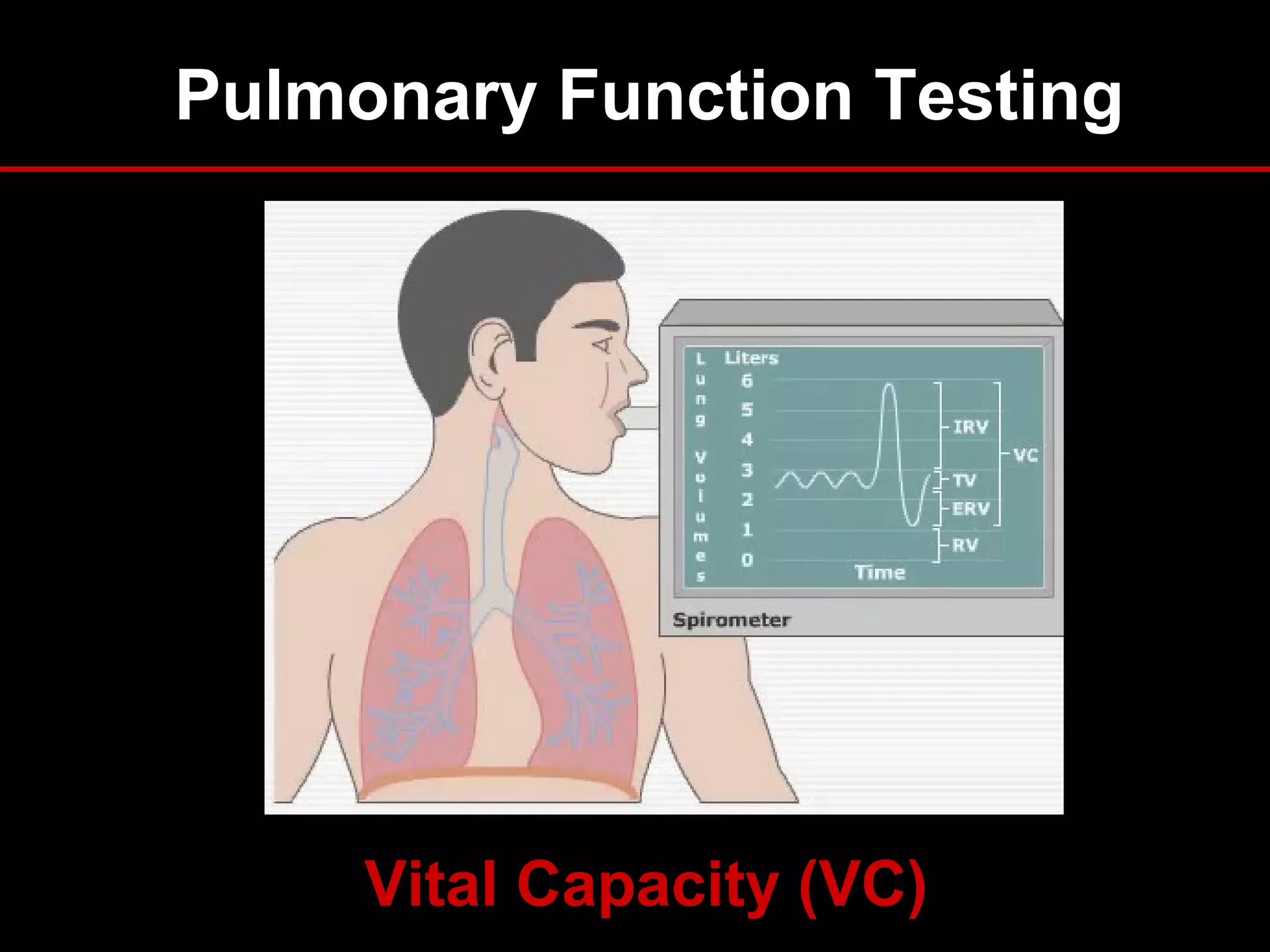
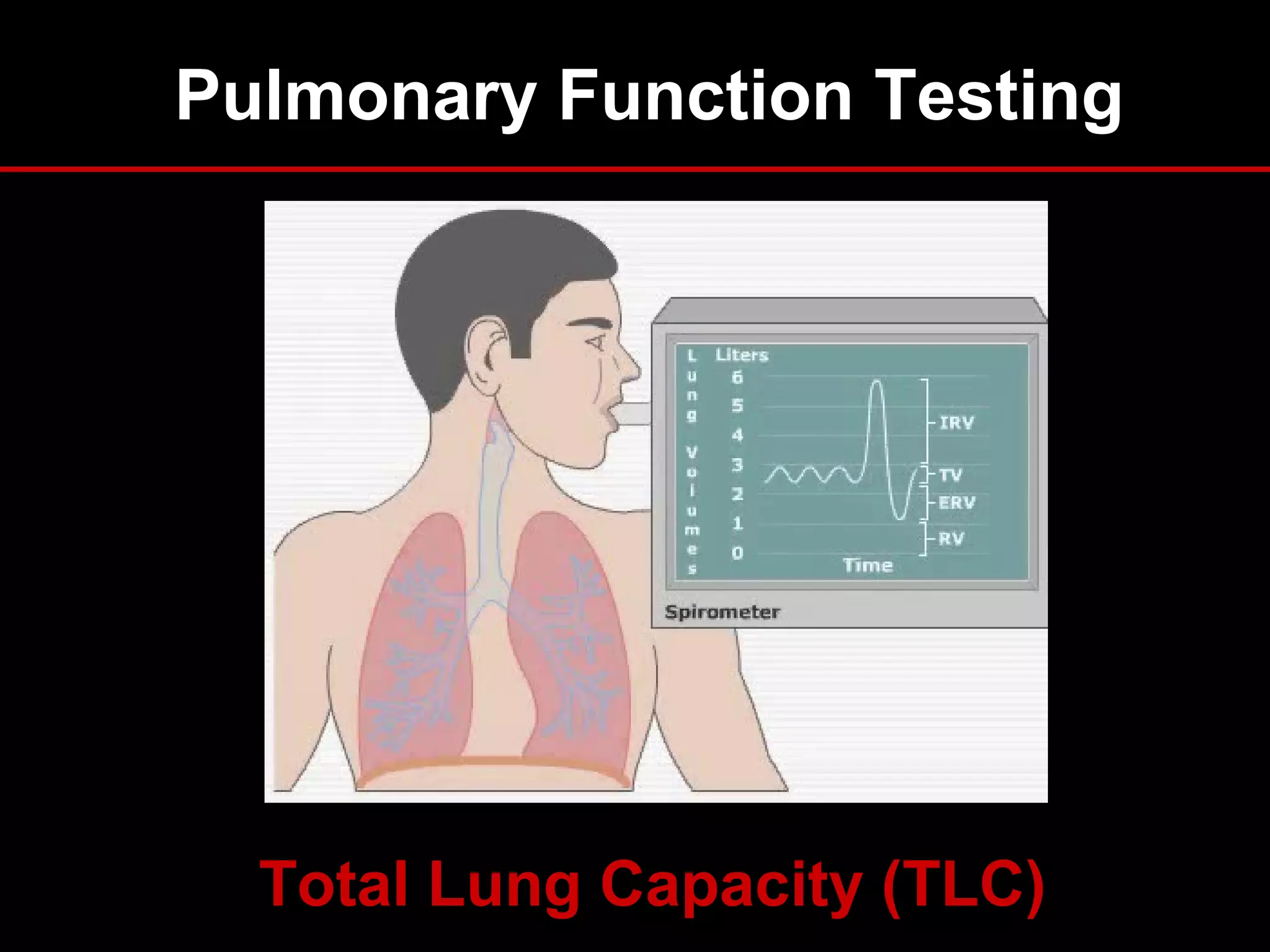
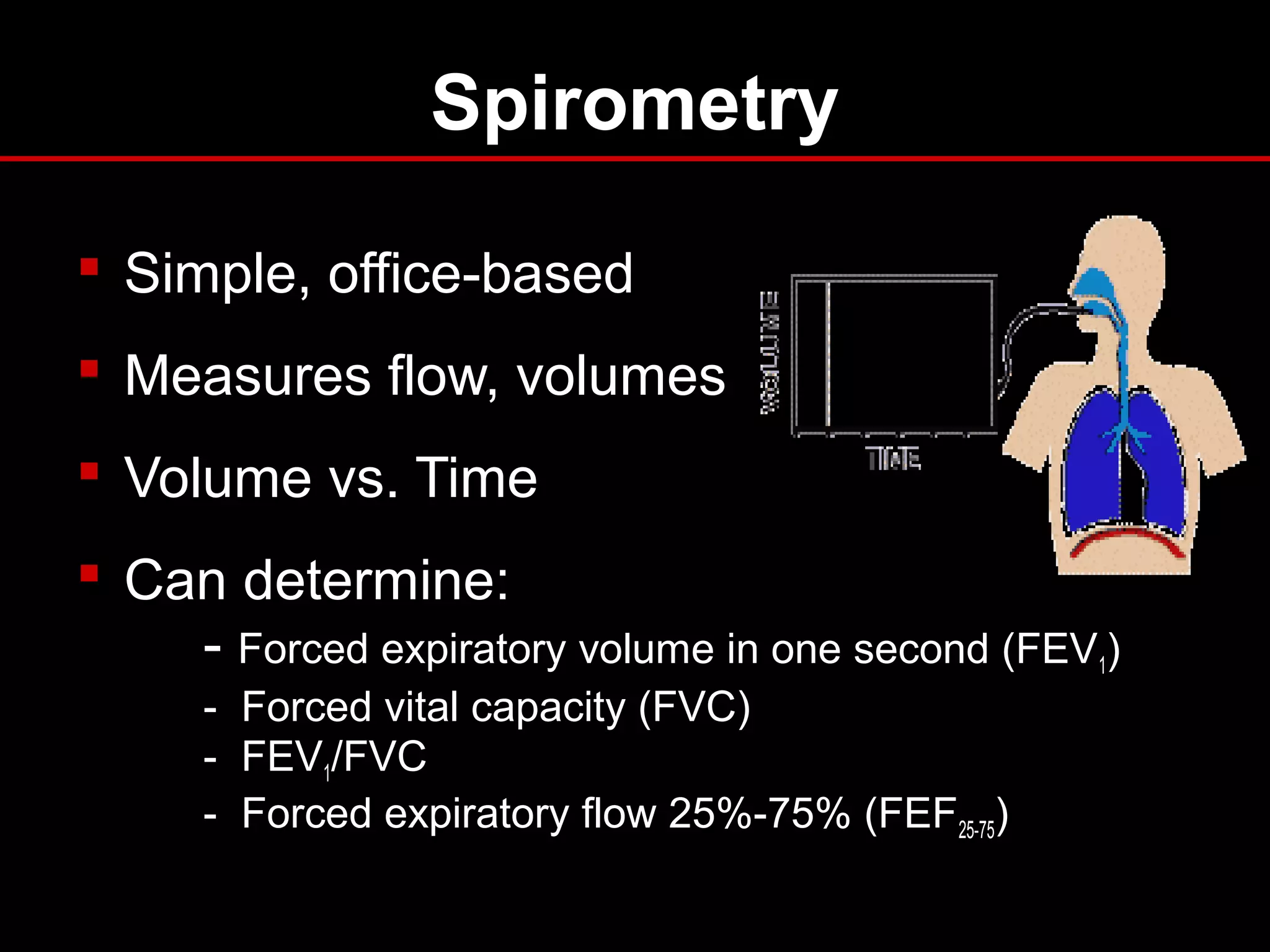
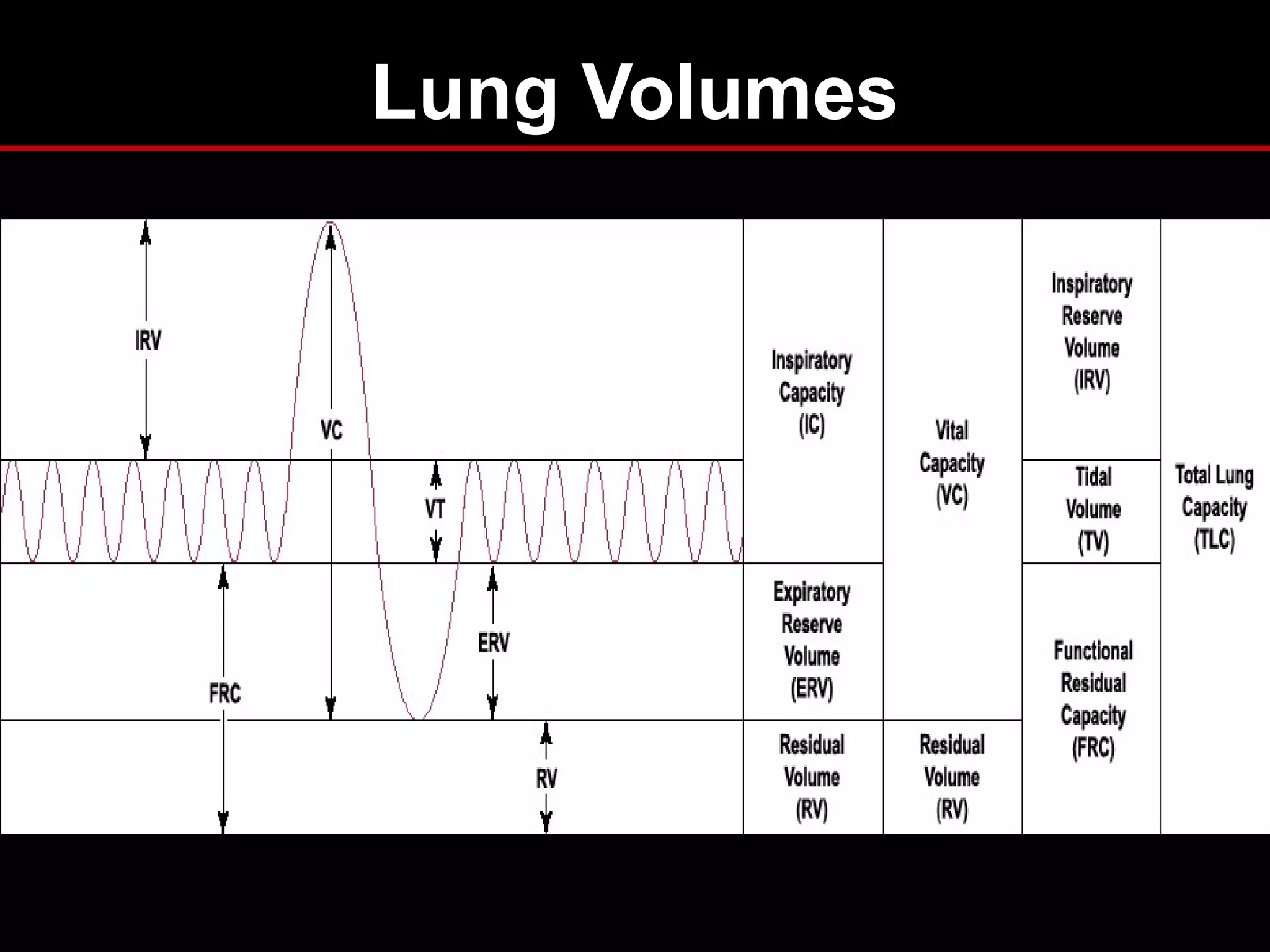
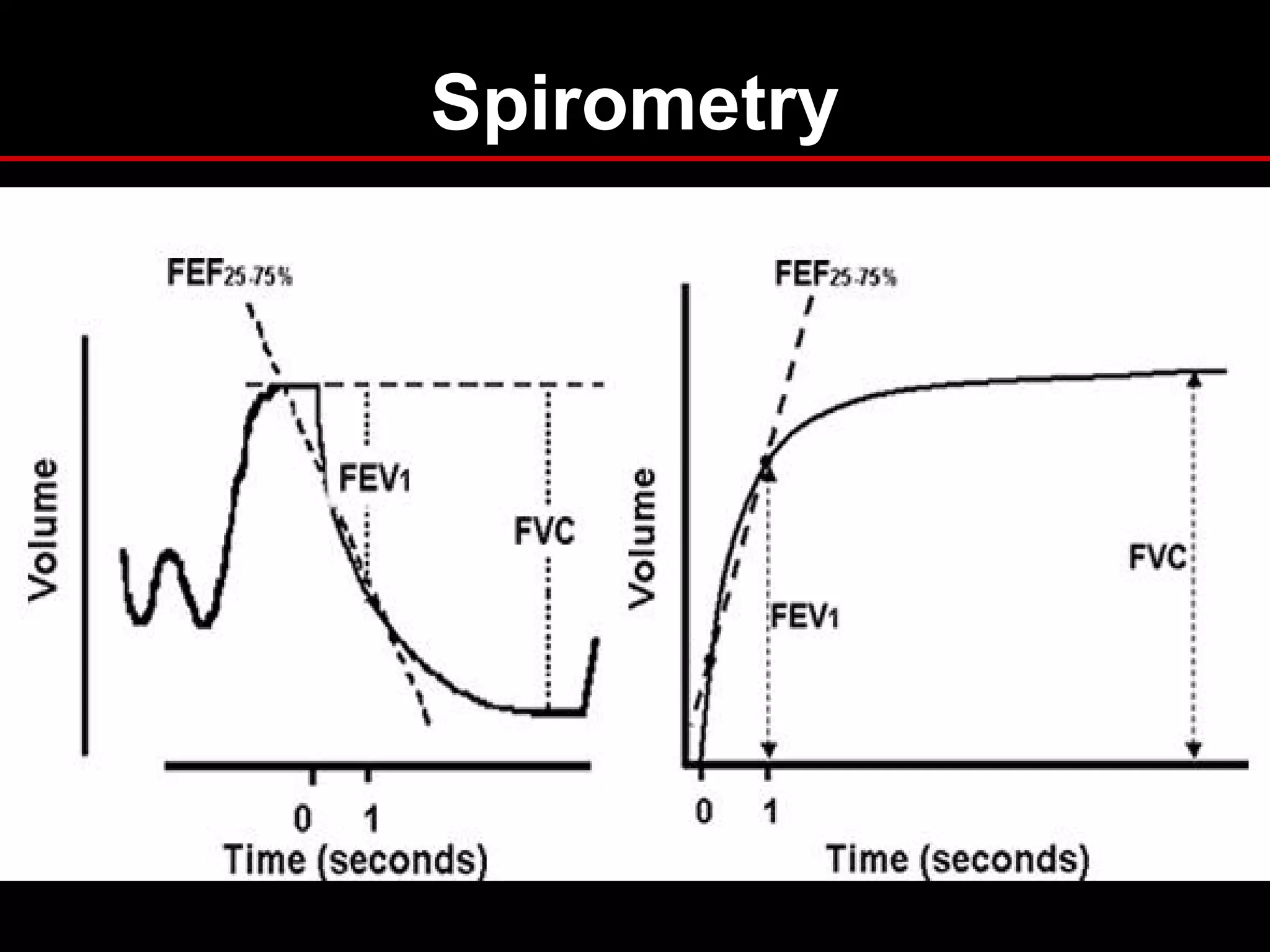
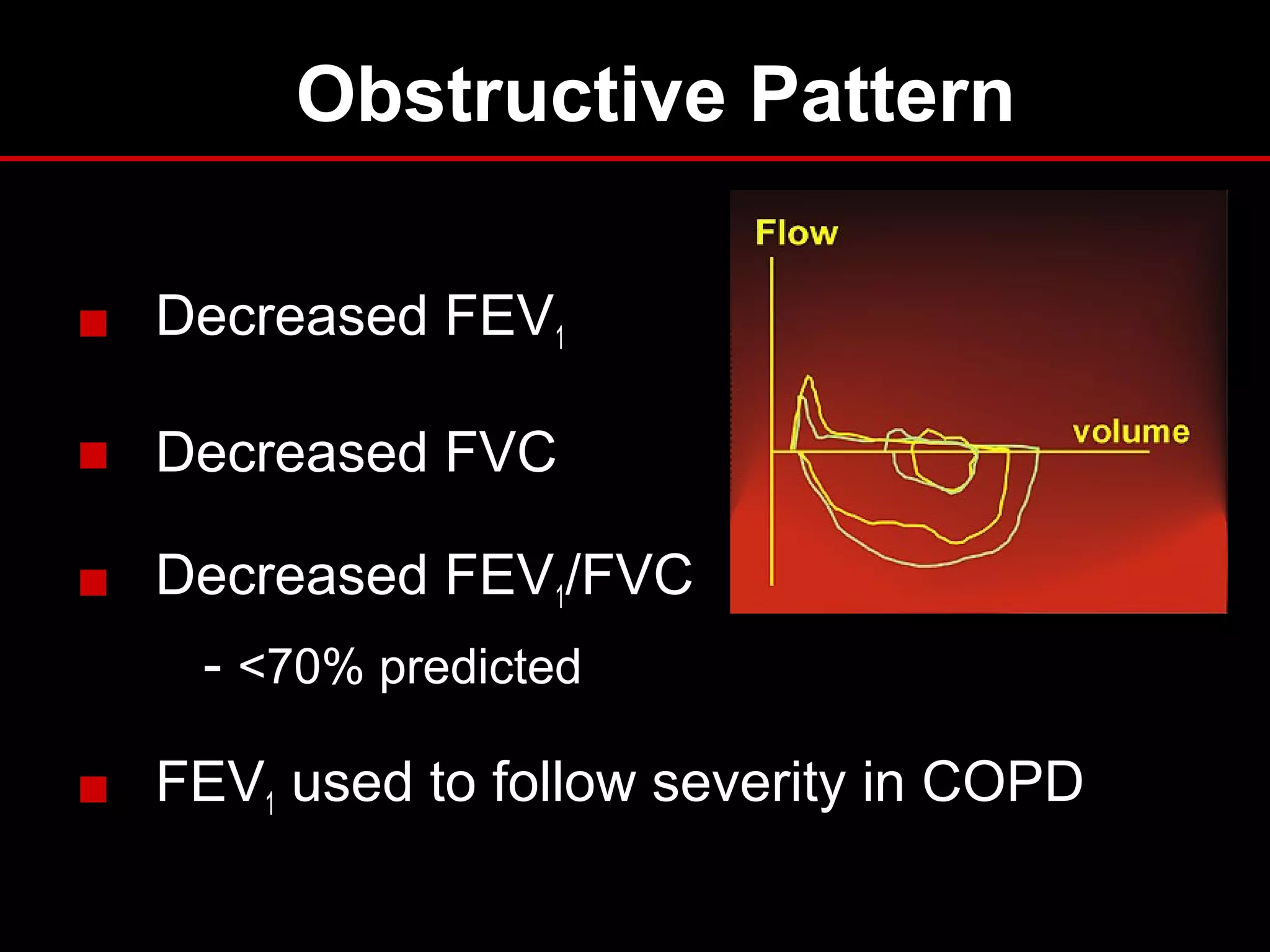
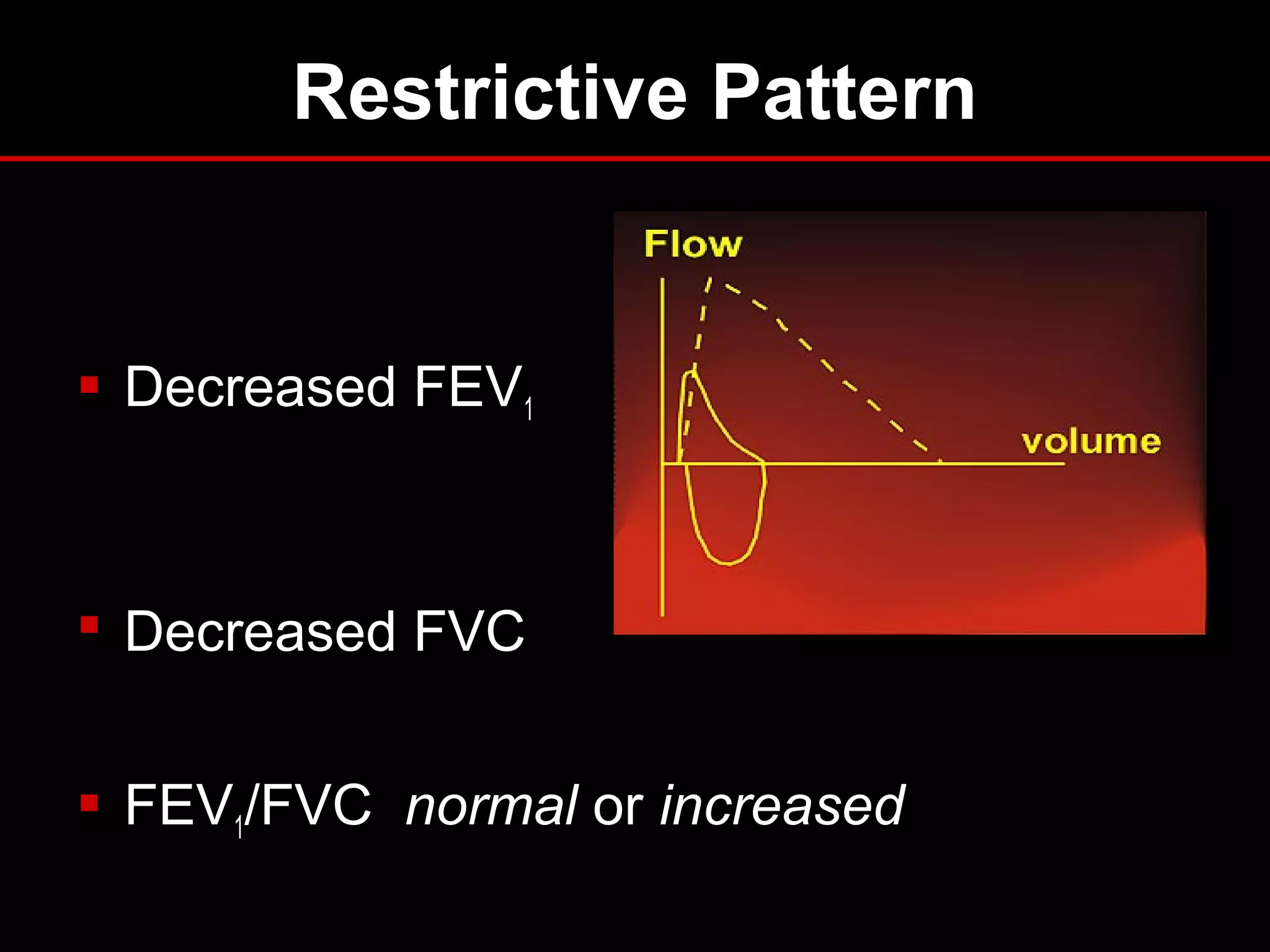
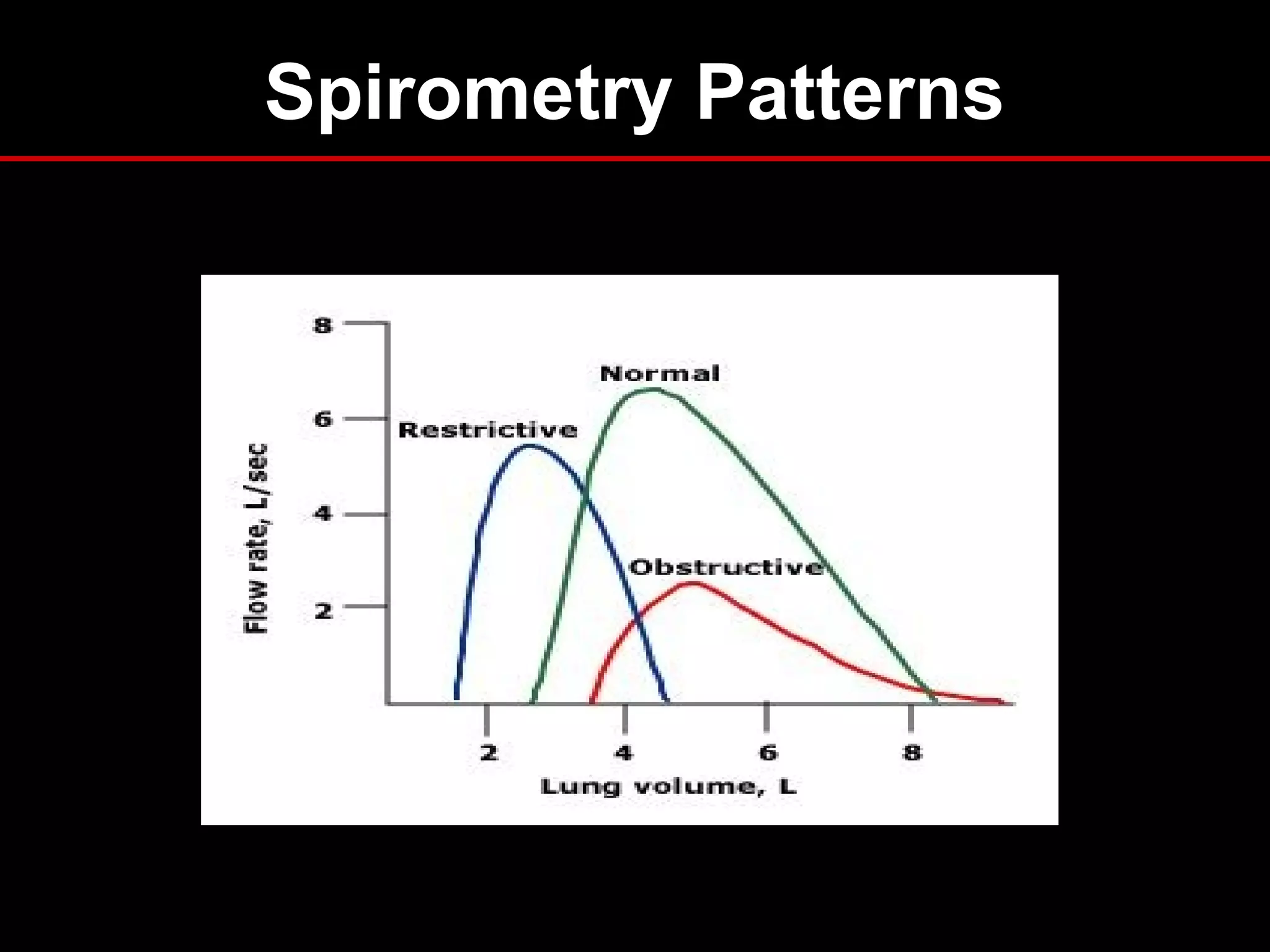
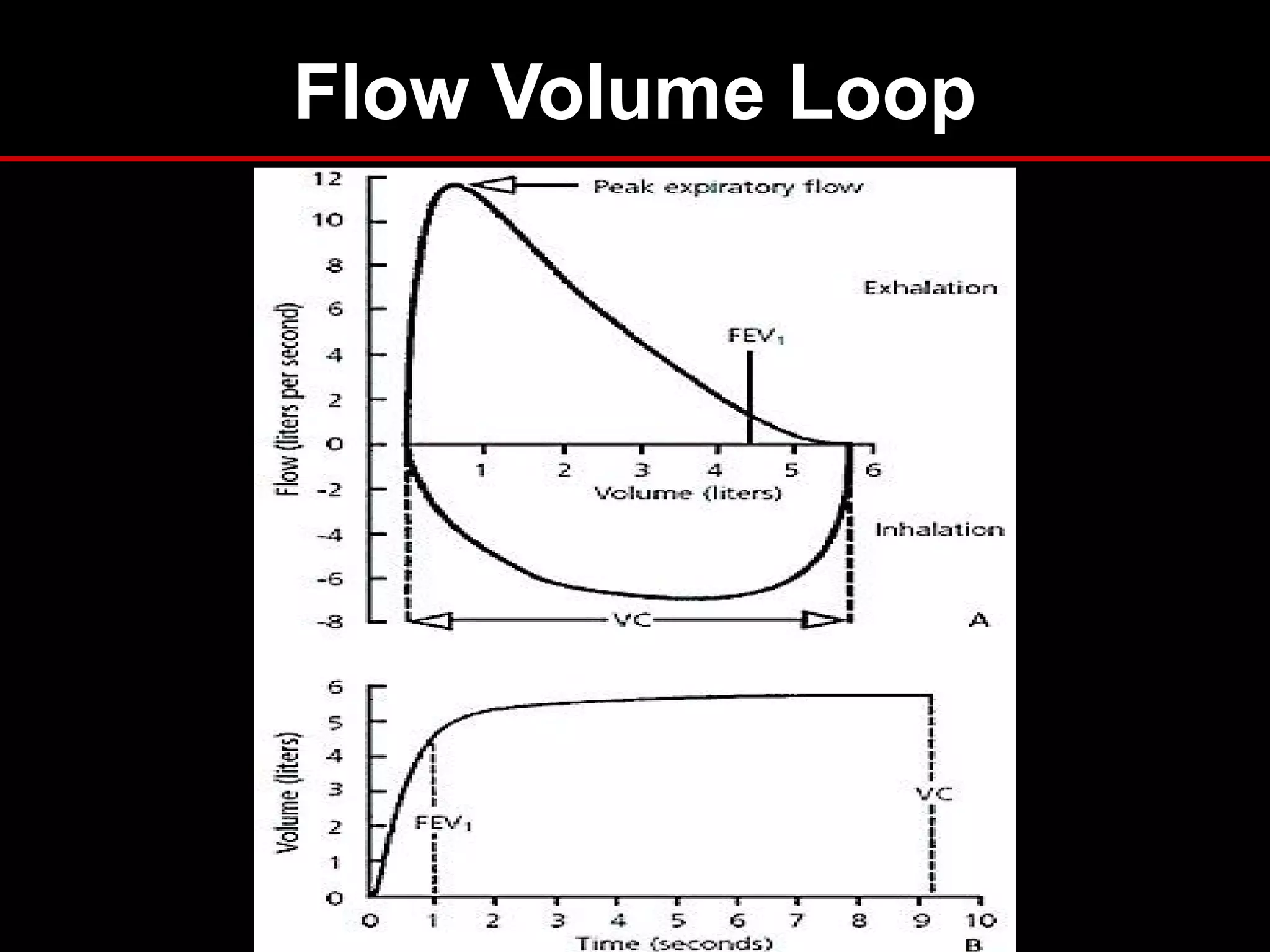
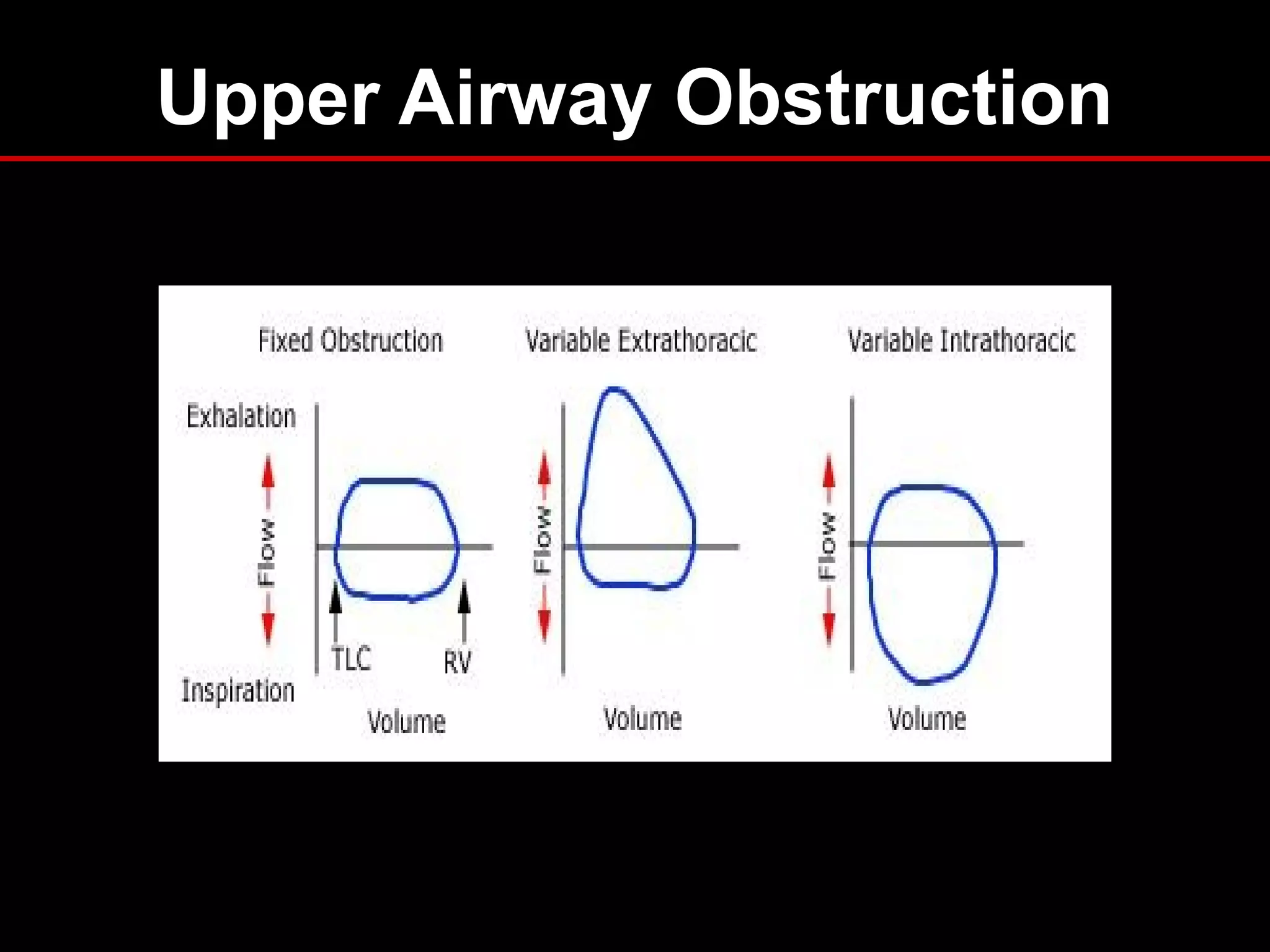
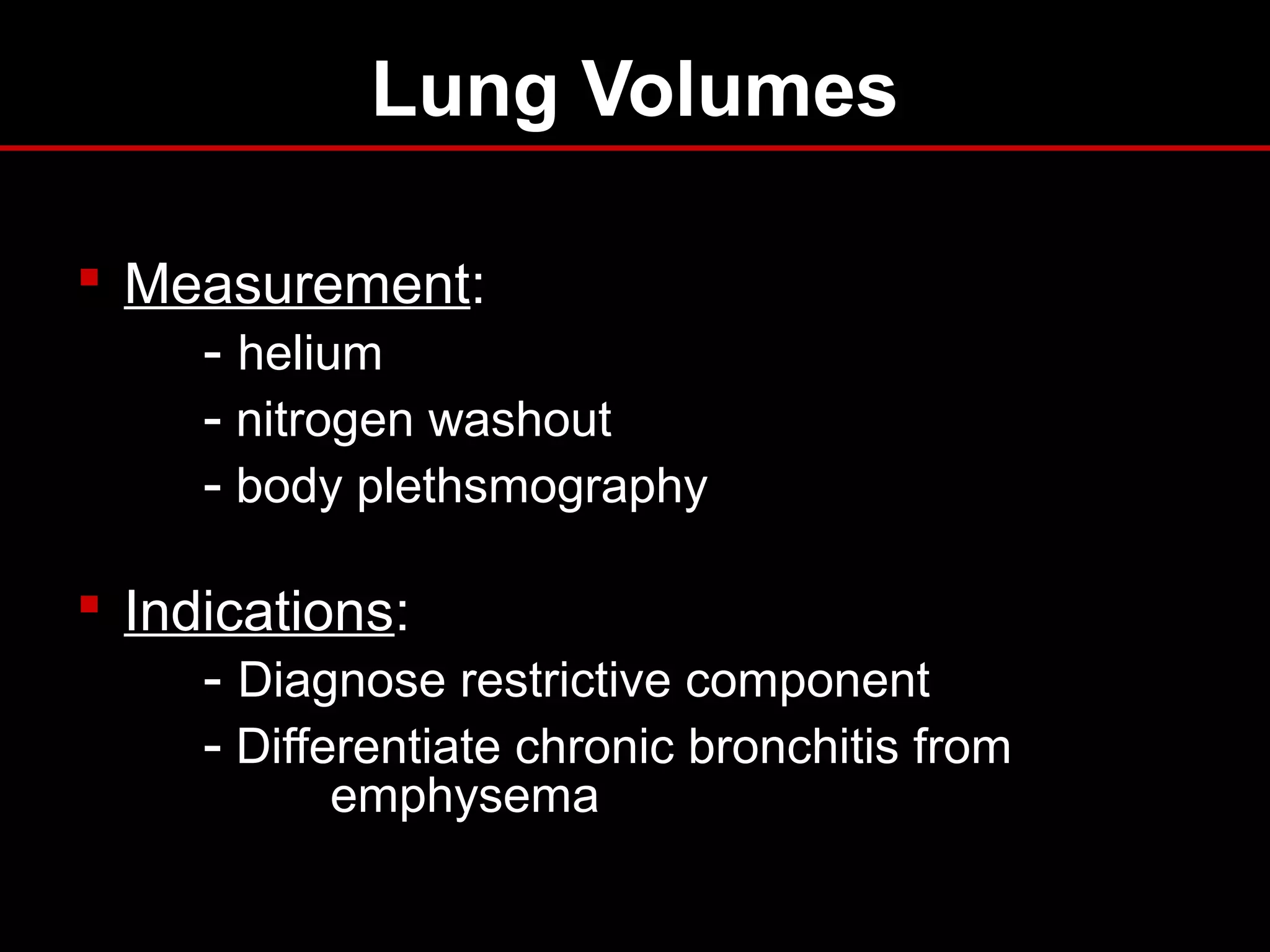
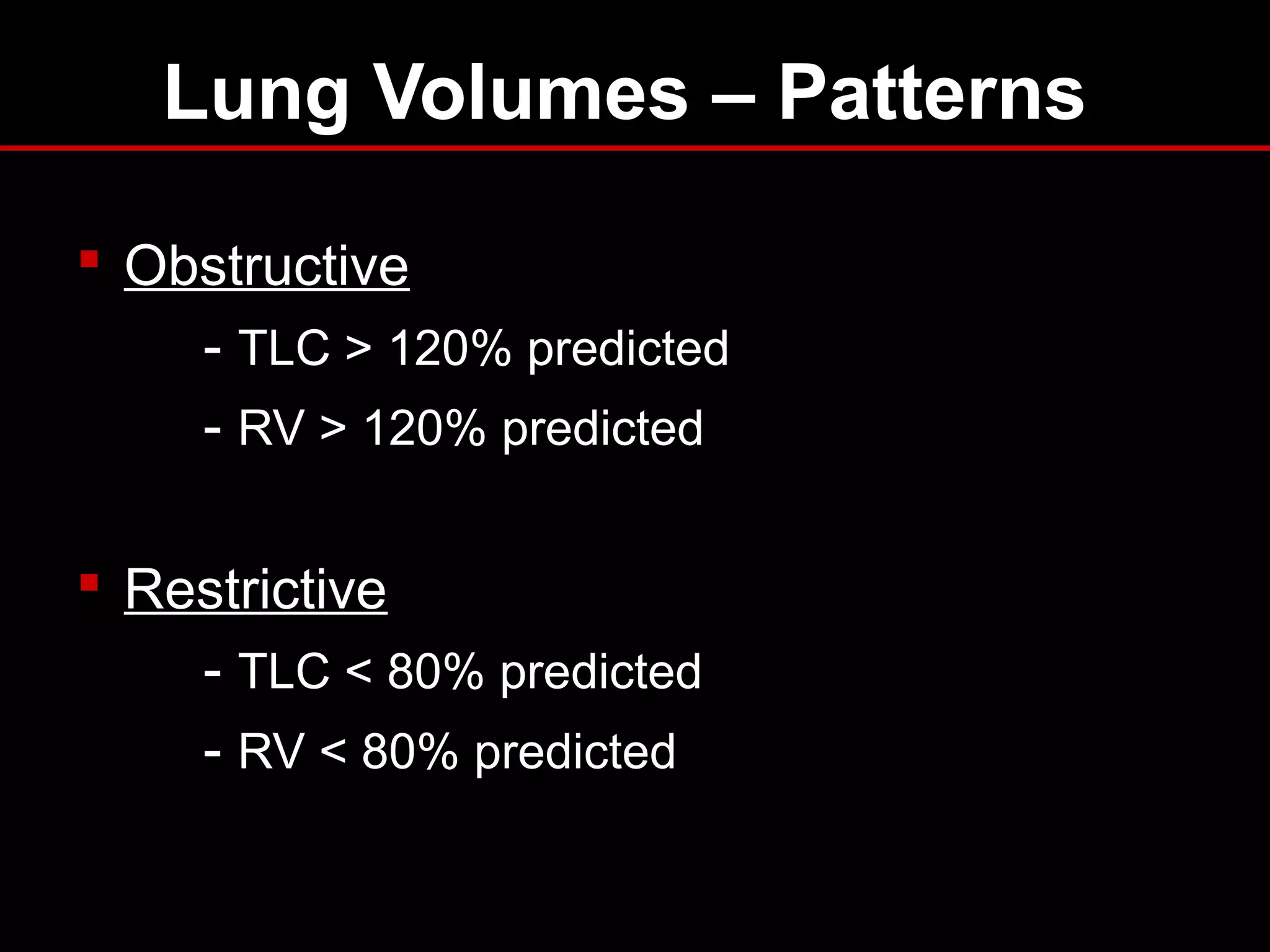
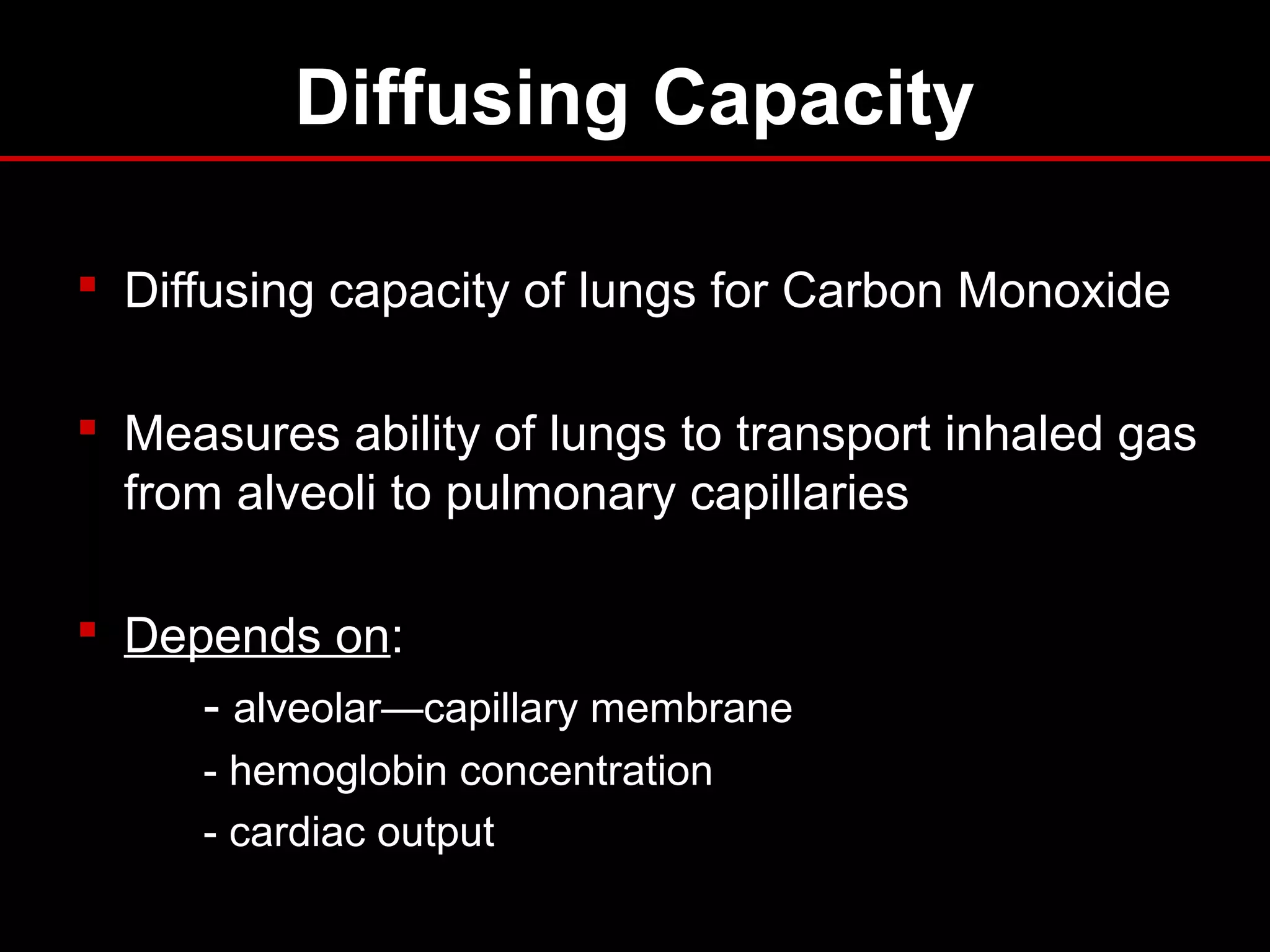
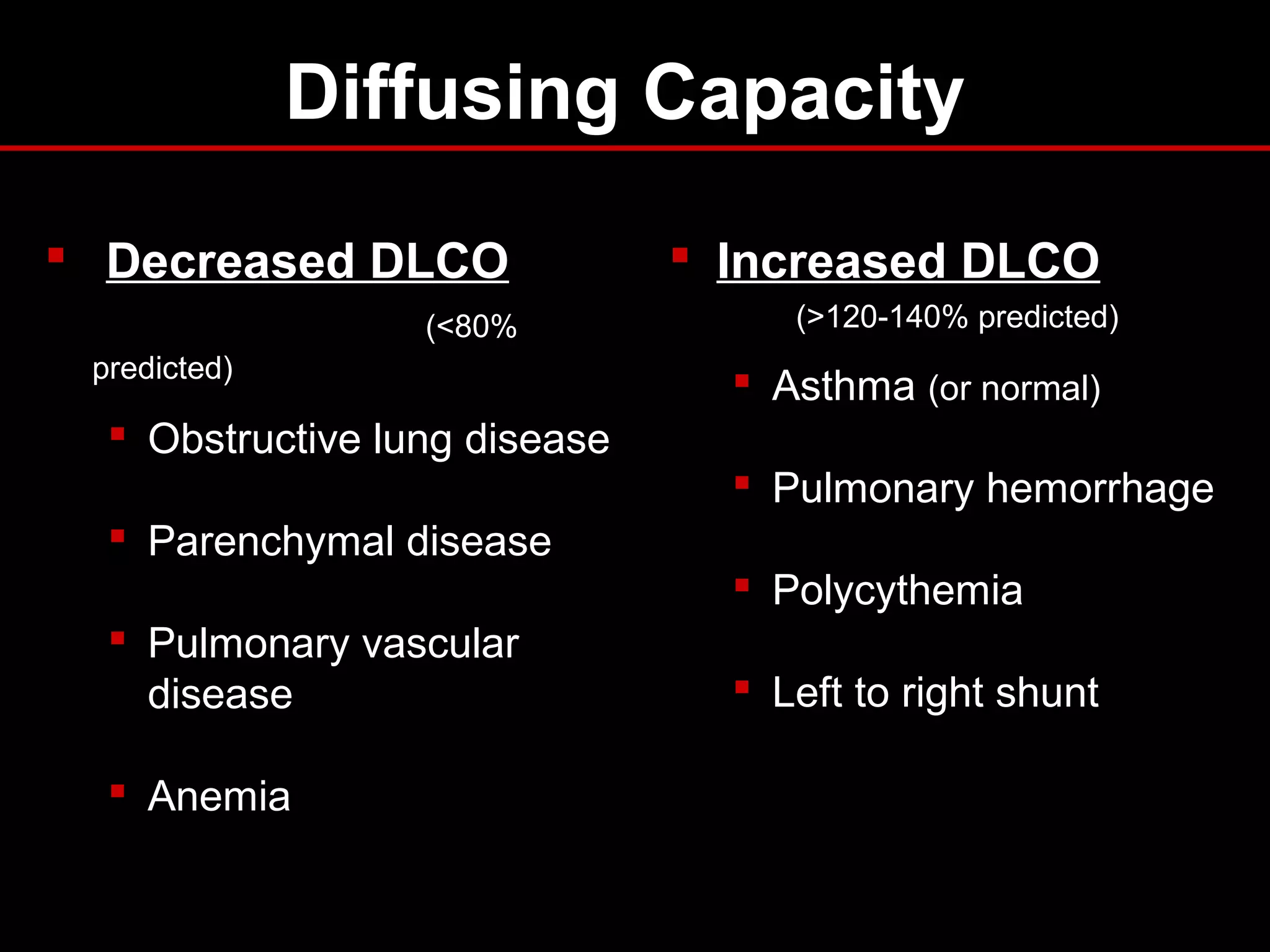
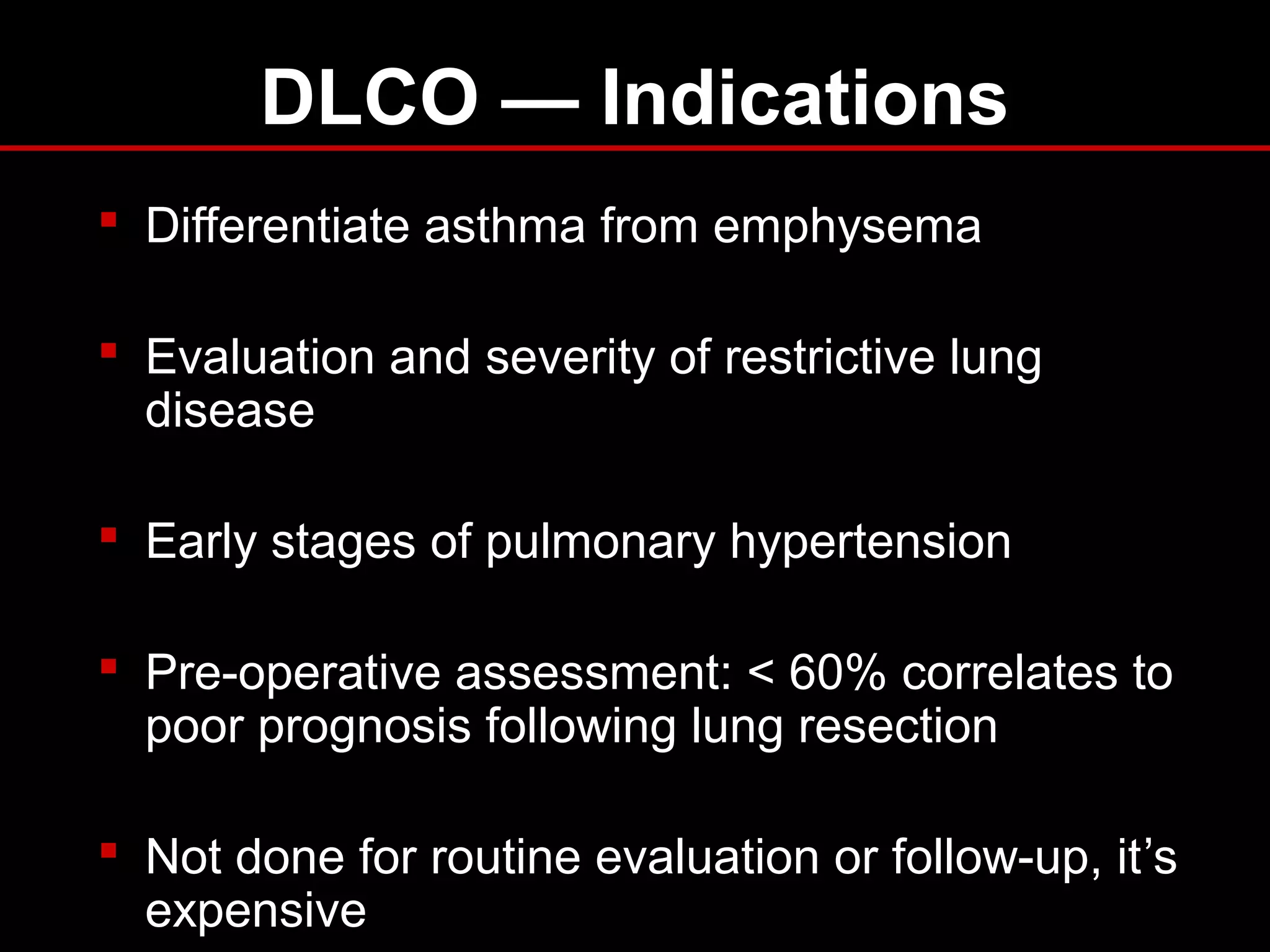
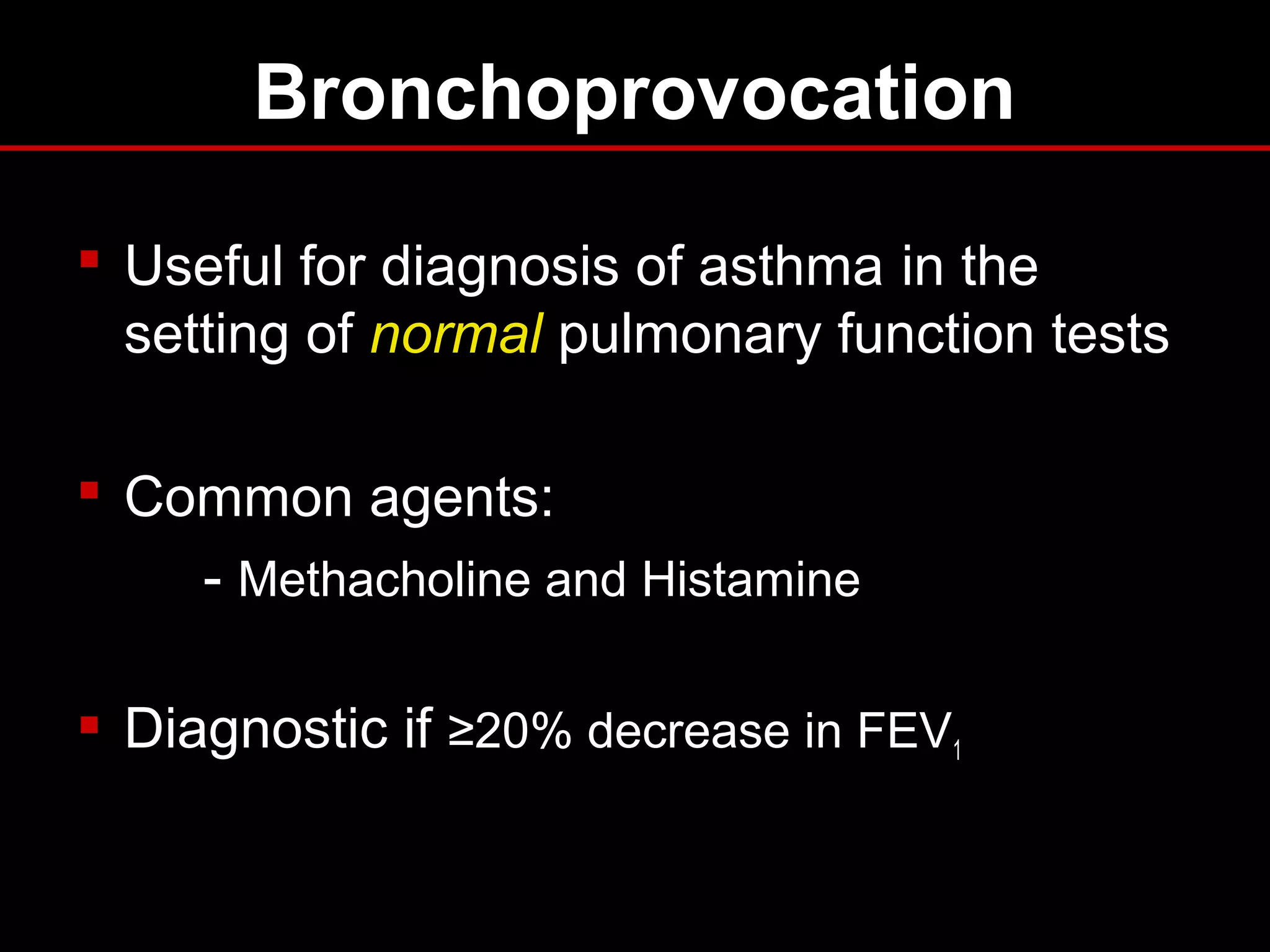
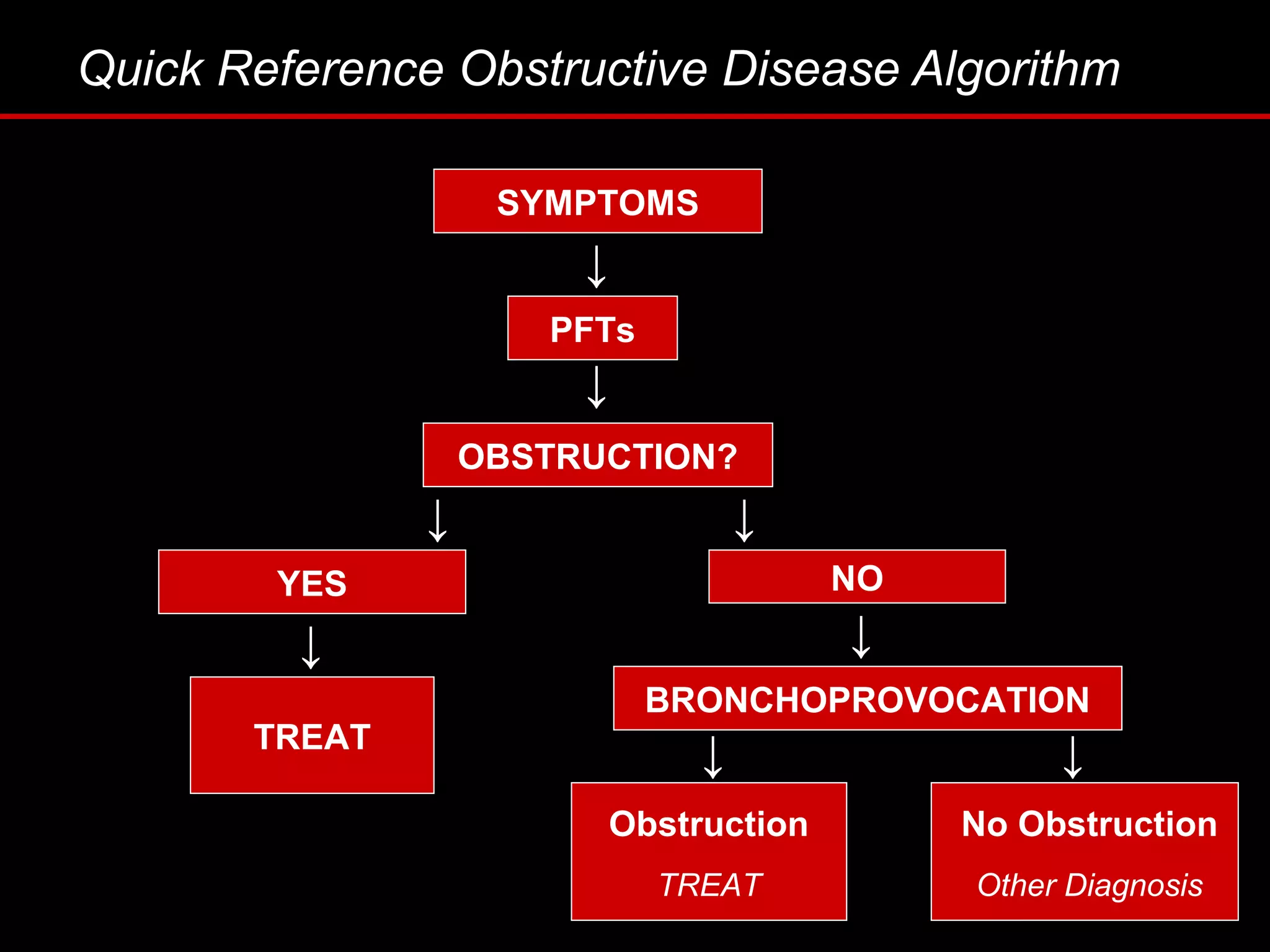
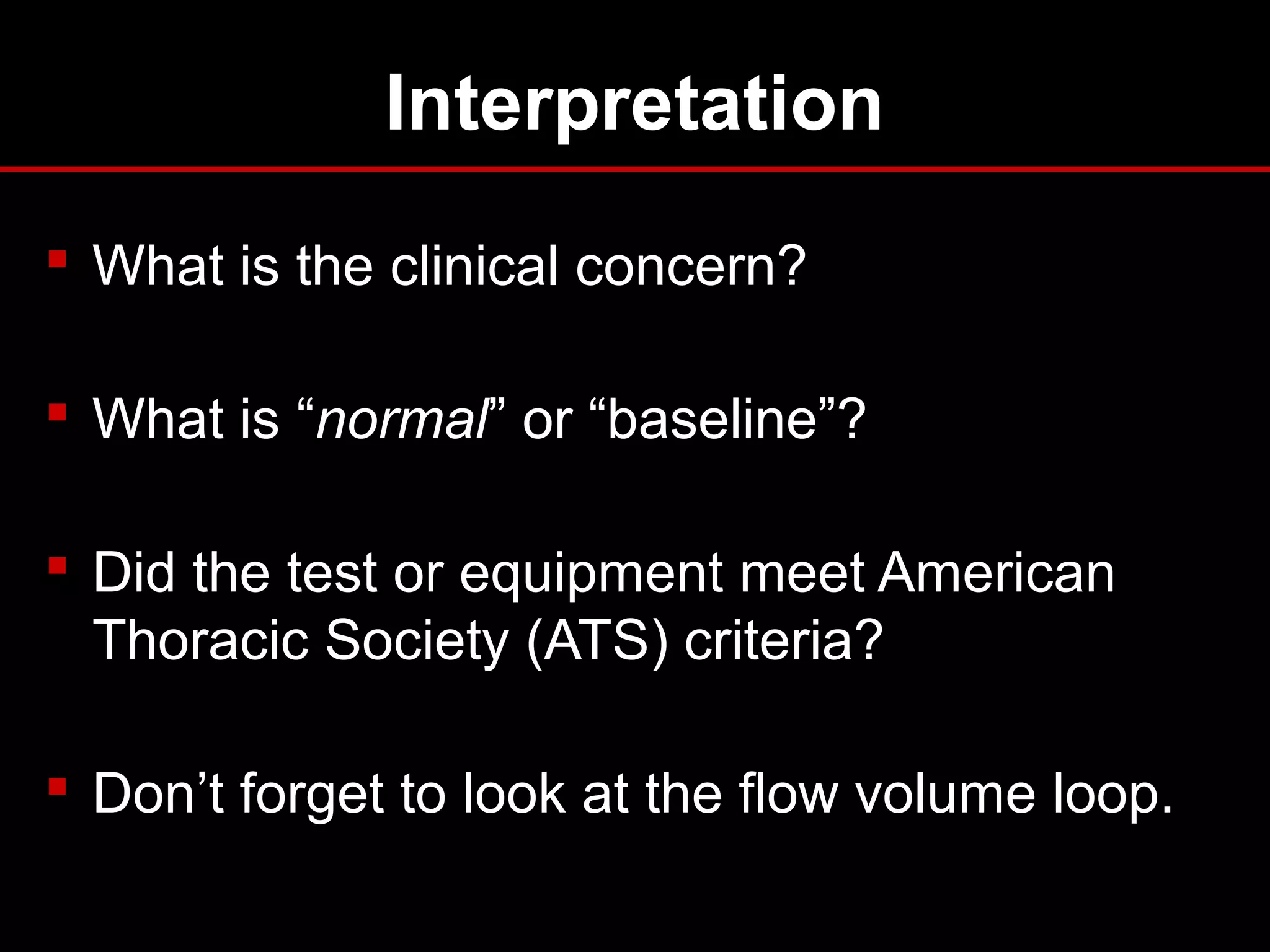
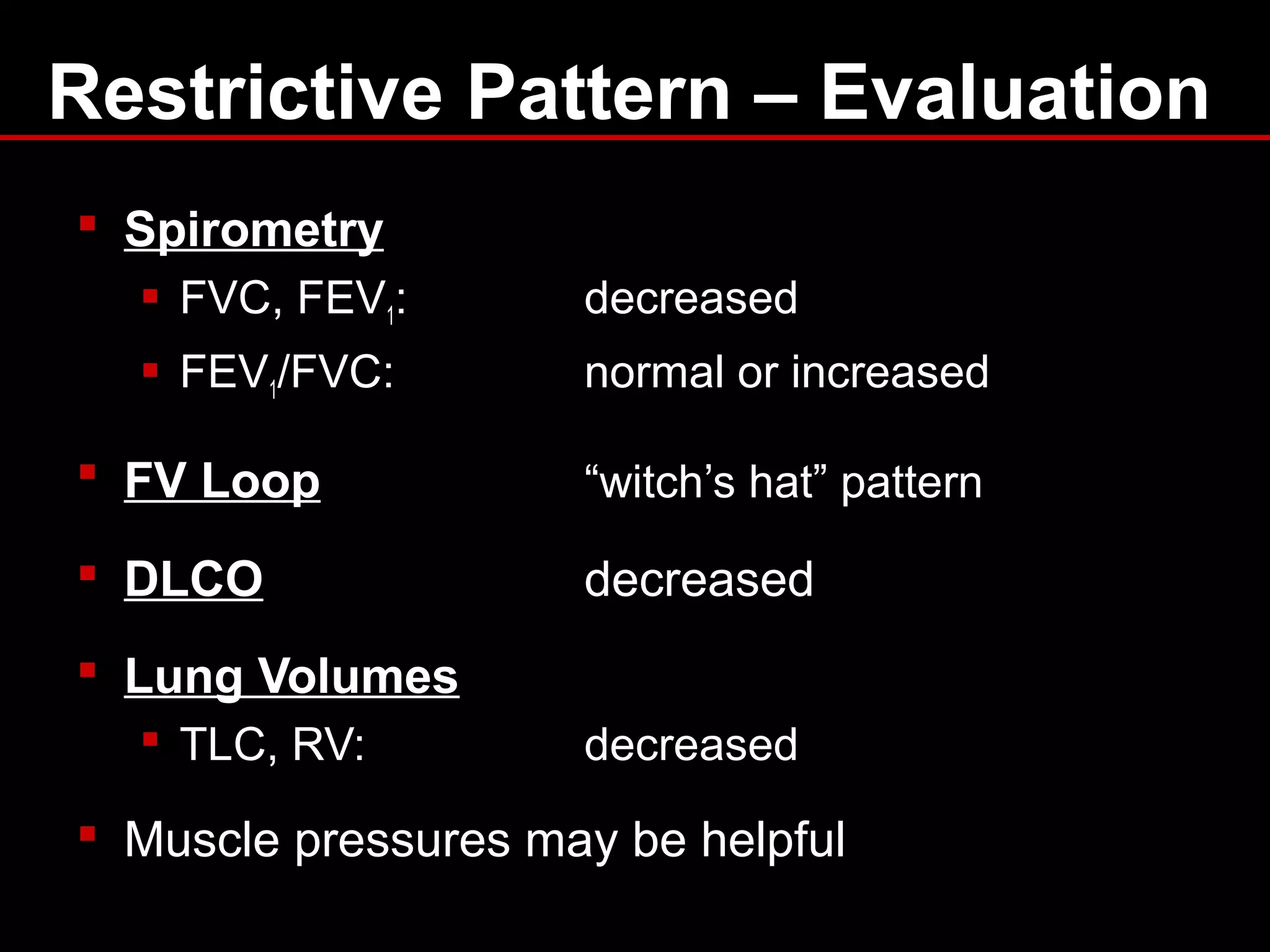
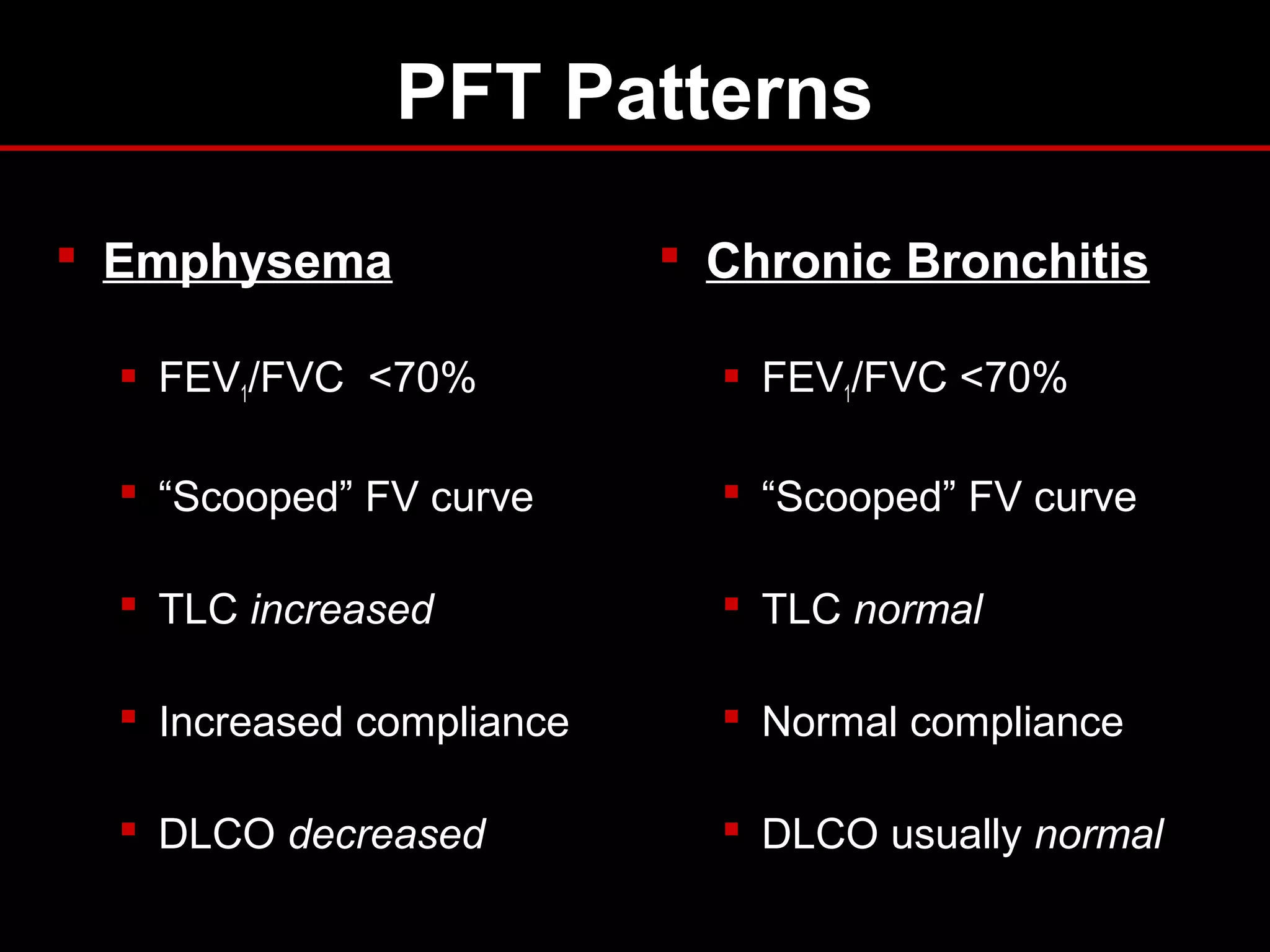
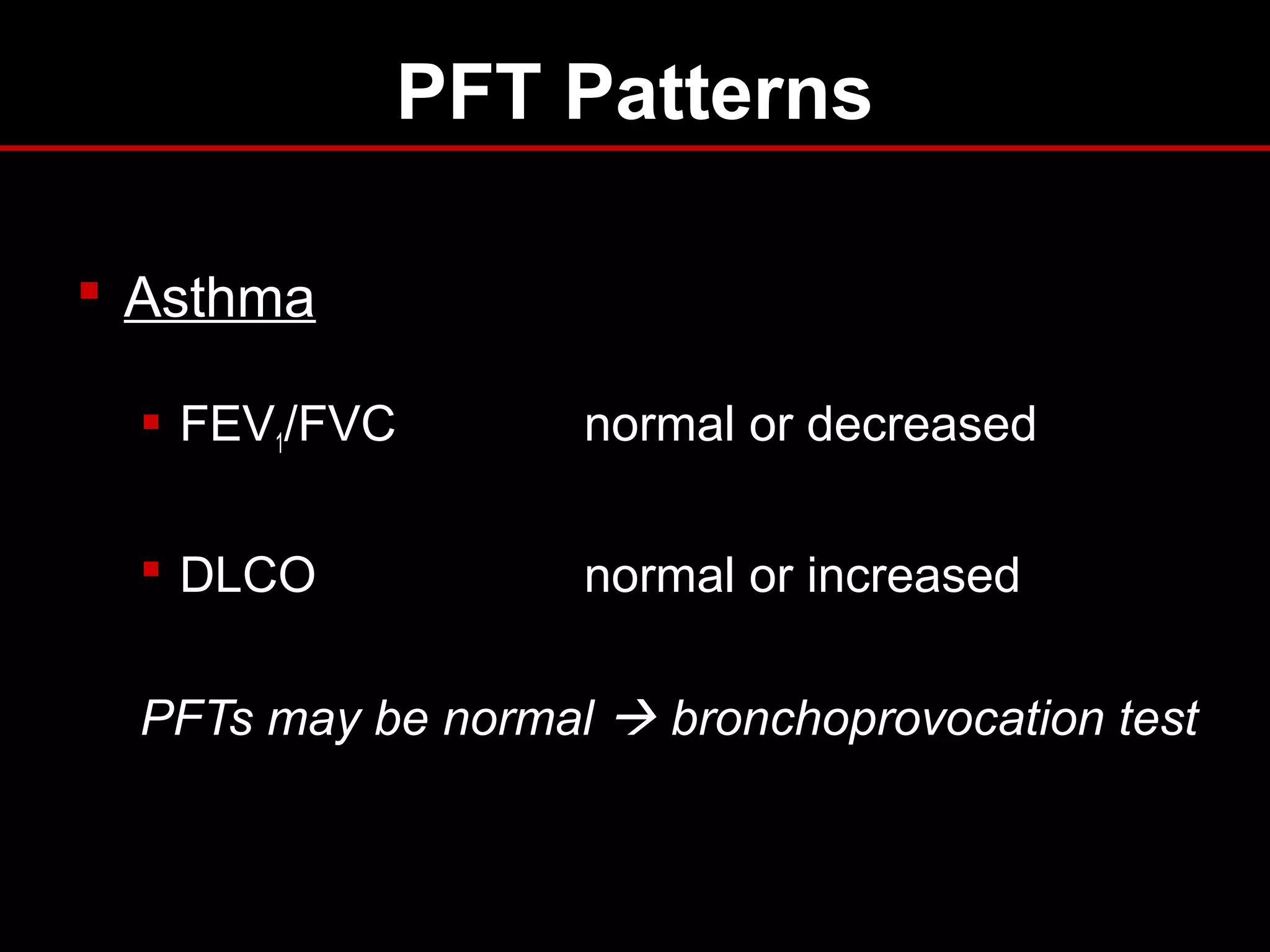
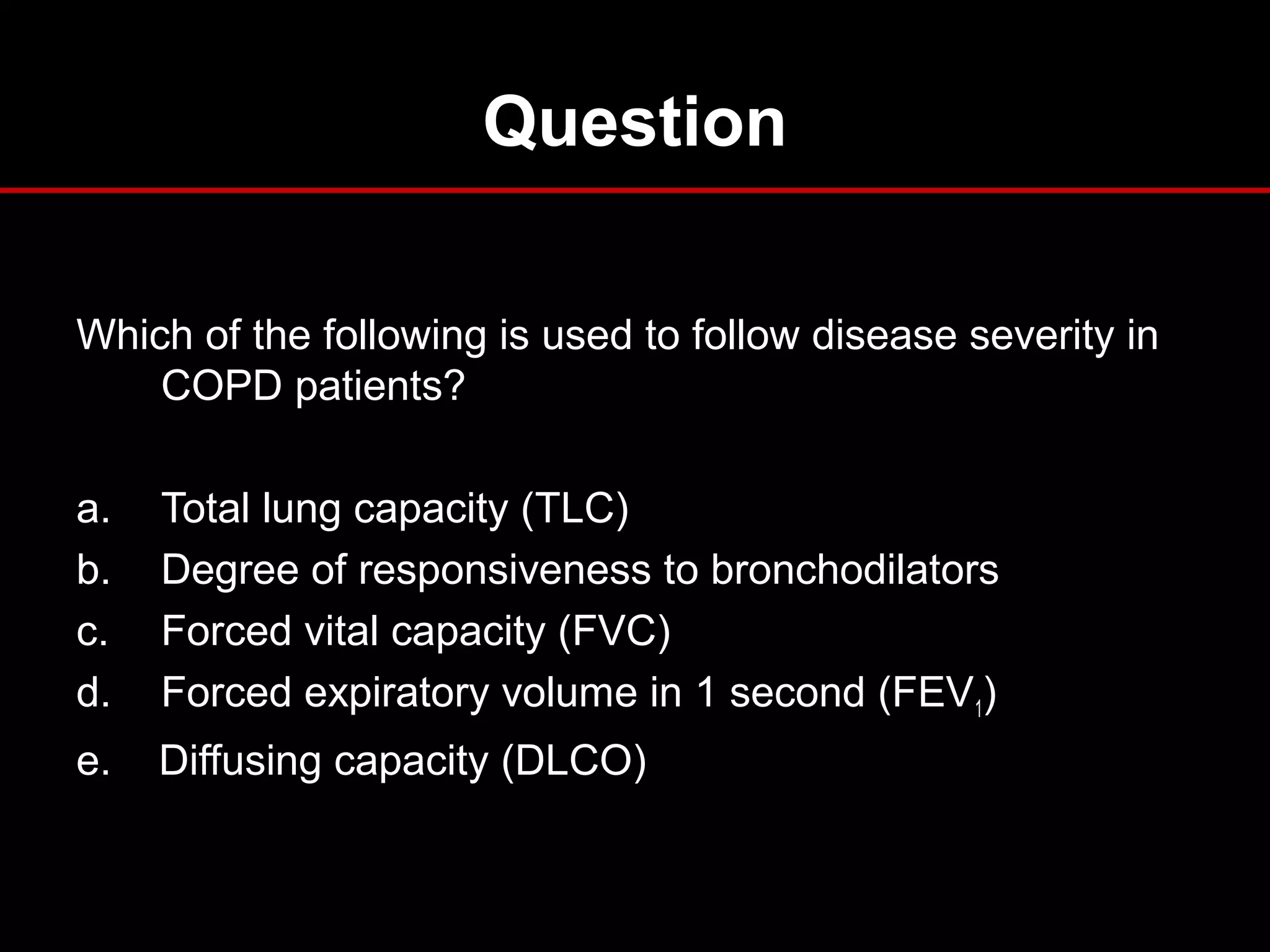
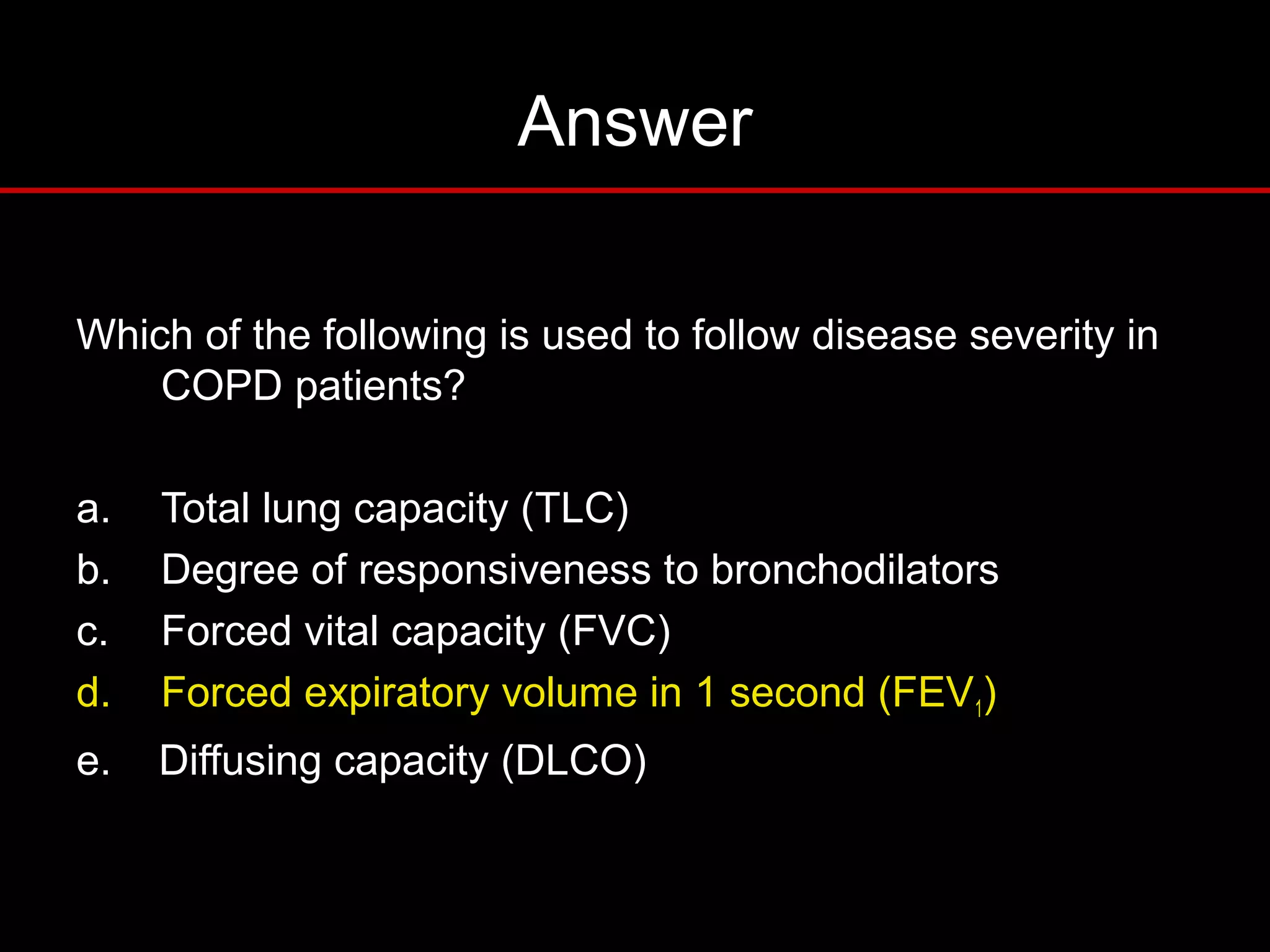
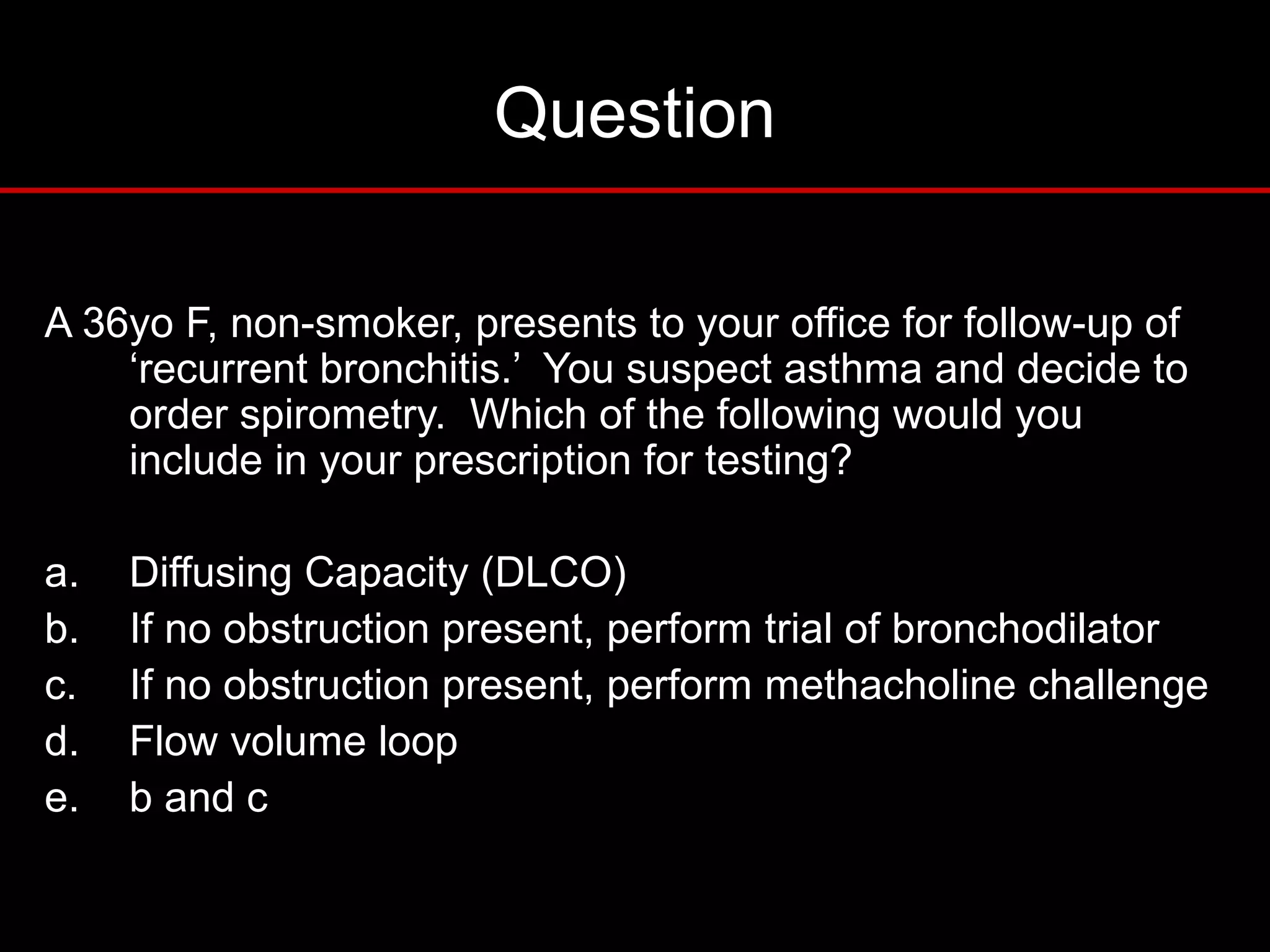
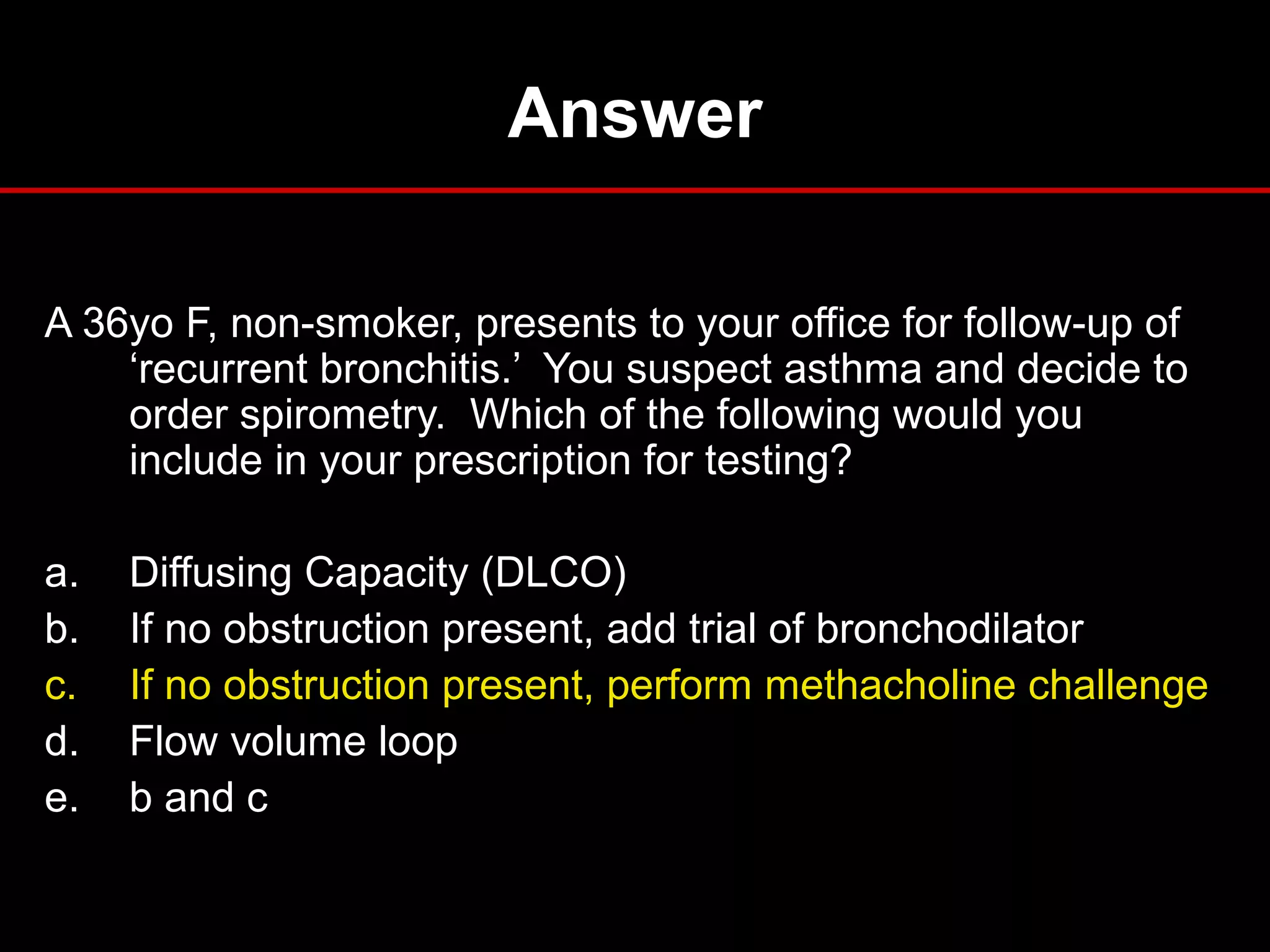
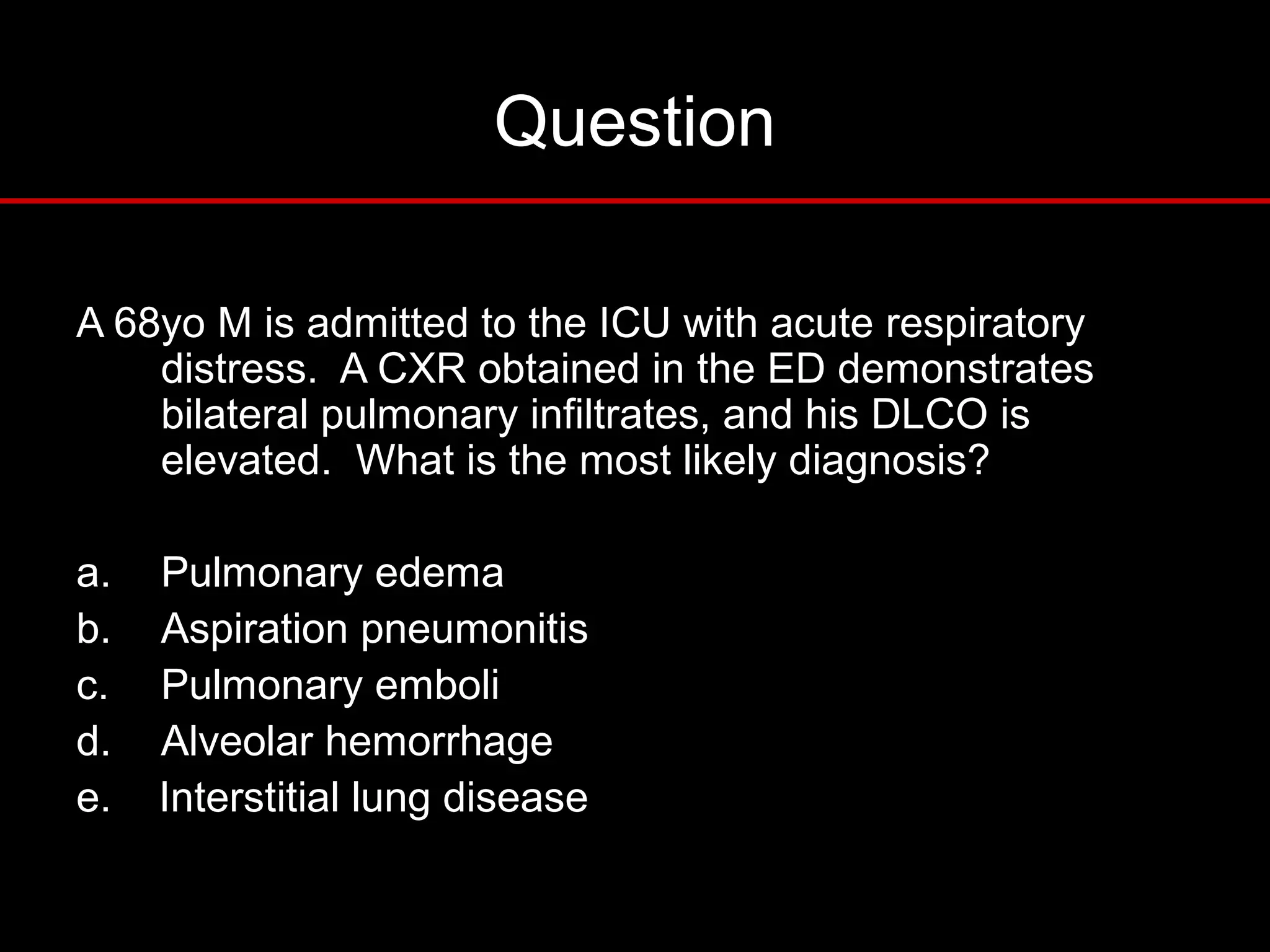
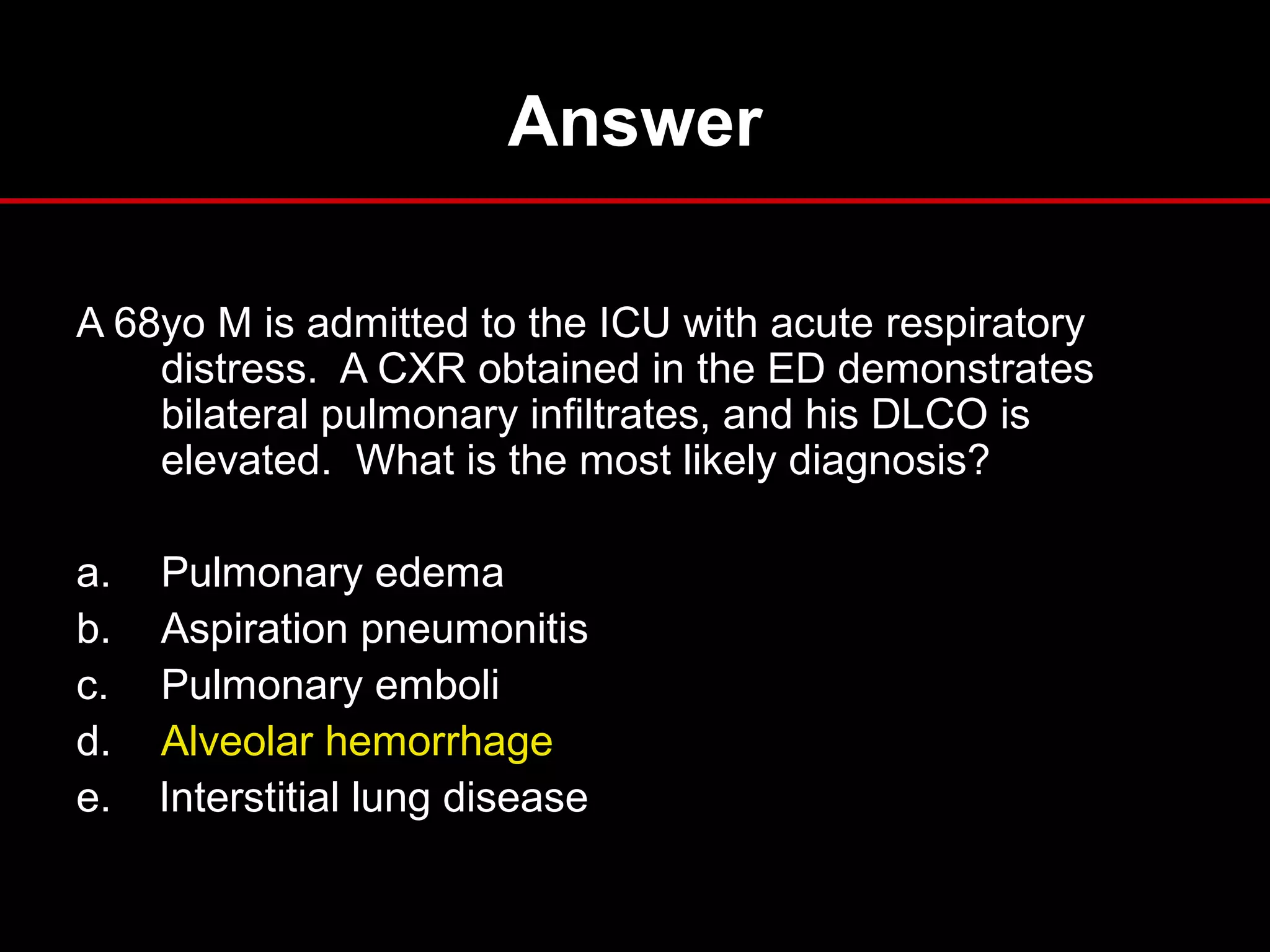
This document provides an overview of pulmonary function testing (PFT), including the components measured, indications for testing, interpretation of results, and clinical applications. It describes common PFT measurements like spirometry, lung volumes, diffusing capacity, and bronchoprovocation testing. Obstructive and restrictive patterns are discussed. The document also reviews indications for PFTs in diagnosis and prognosis of lung diseases and provides examples of PFT patterns in conditions like asthma, COPD, and interstitial lung disease.