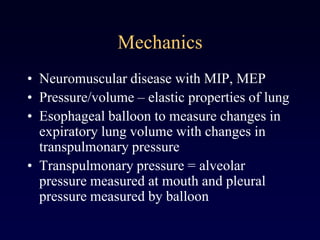
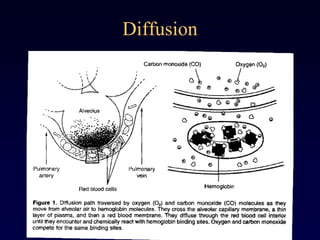
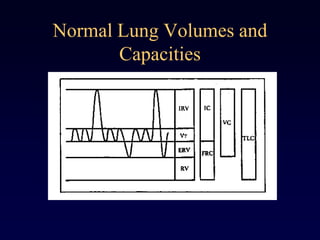
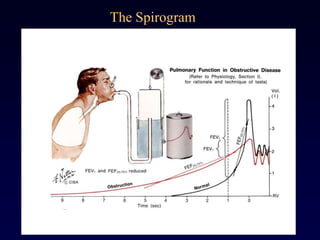
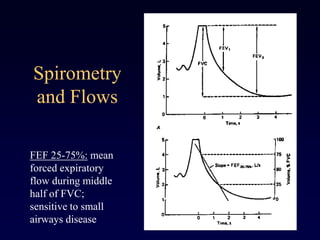
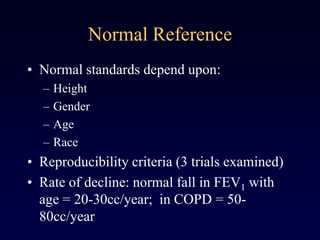
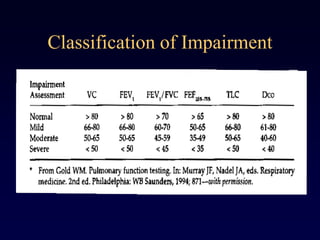
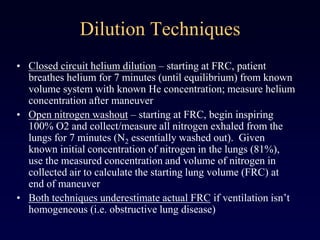
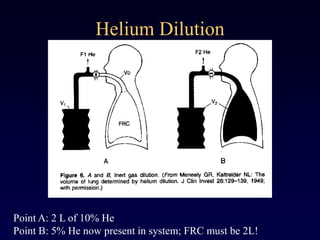
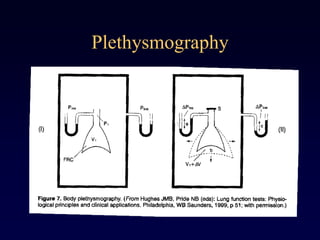
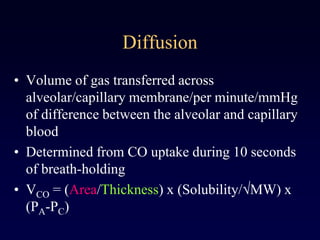
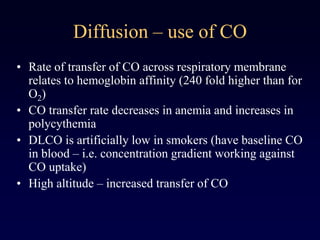
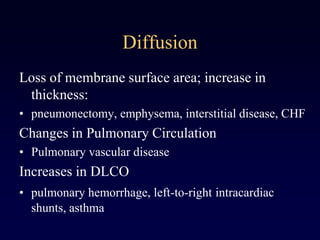
Pulmonary function tests (PFTs) are used to characterize and monitor pulmonary disease. Common PFTs include spirometry to assess airflow limitation, lung volume measurements to detect restriction, diffusion capacity to evaluate gas exchange, and bronchoprovocation tests to identify airway hyperresponsiveness. Spirometry yields values like FEV1, FVC, and their ratio that are used to classify obstructive and restrictive patterns. Lung volumes are directly measured using techniques like plethysmography and indirectly calculated from spirometry. Diffusion capacity reflects membrane thickness and surface area via carbon monoxide transfer. PFTs provide objective data to diagnose and manage respiratory conditions.

![Pulmonary Gas Exchange
• Evaluating Hypoxemia:
• Hypoxemia with normal A-a gradient: hypoventilation
• Hypoxemia with increased A-a gradient: V/Q
mismatch, right-to-left shunt, diffusion impairment
• P(A-a)O2 = [PiO2 –(PaCO2/R)] – PaO2
• P(A-a)O2 = [0.21(PB-47) – (PaCO2/0.8)] –PaO2
• P(A-a)O2 = 150 – (PaCO2/0.8) – PaCO2](https://image.slidesharecdn.com/pulmonaryfunctionexam-140501005202-phpapp02/85/Pulmonary-function-exam-29-320.jpg)