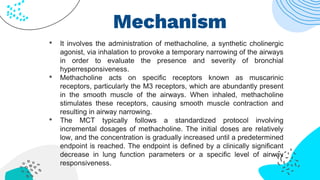
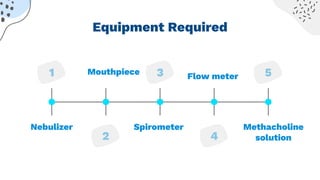
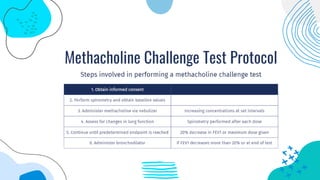
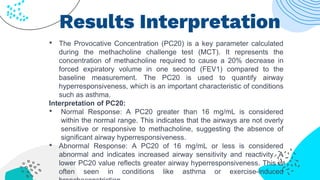
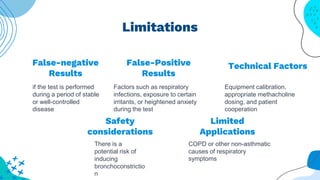
The methacholine challenge test is used to diagnose and manage respiratory disorders like asthma. It involves inhaling increasing doses of methacholine, which acts on airway muscle receptors to cause contraction. Spirometry is then used to measure the sensitivity of the airways. A PC20 value is calculated from the spirometry results to quantify airway hyperresponsiveness, with a value below 16 mg/mL indicating abnormal sensitivity. While the test provides information about asthma and other conditions, there are limitations like potential safety issues from induced bronchoconstriction and factors that could produce false positive or negative results.