This document discusses bronchiectasis, including its definition, etiology, clinical features, diagnosis, management, and complications. Some key points:
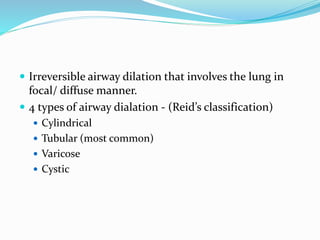
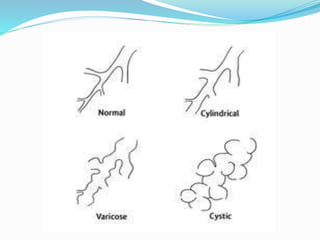
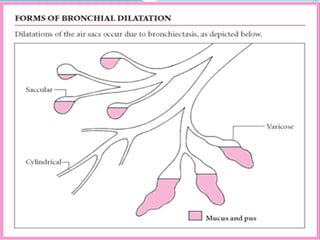
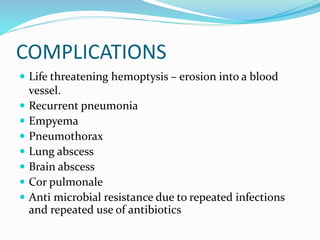
- Bronchiectasis is irreversible dilation of the airways caused by infection or other insults that damages the airways and impairs mucus clearance.
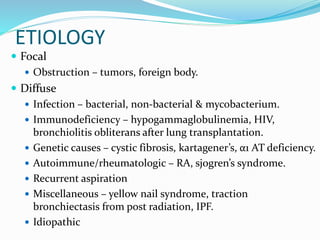
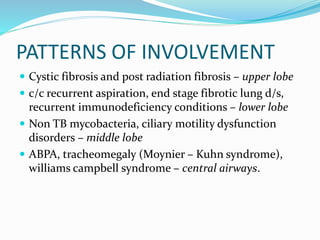
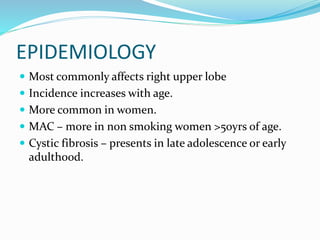
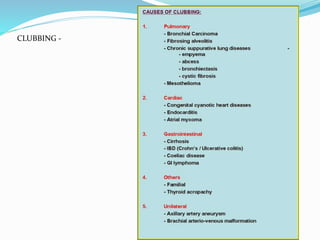
- It has various etiologies including infection, immunodeficiency, genetic disorders, and aspiration. Recurrent infections lead to a vicious cycle of inflammation and further airway damage.
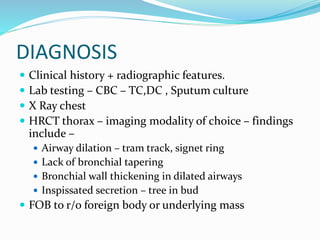
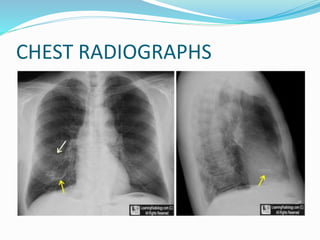
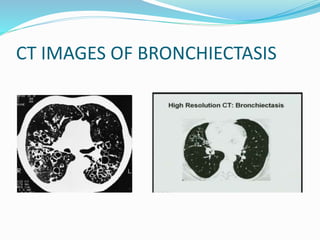
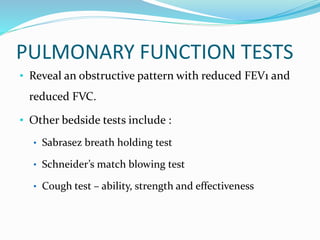
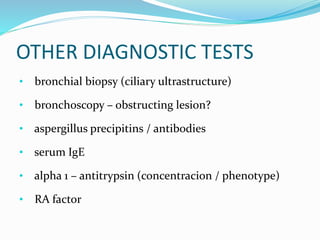
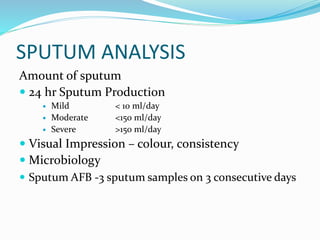
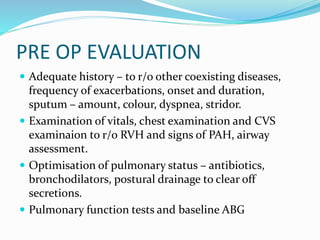
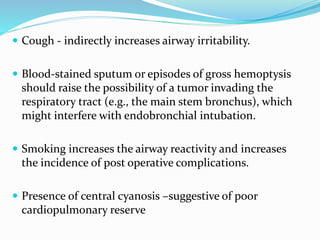
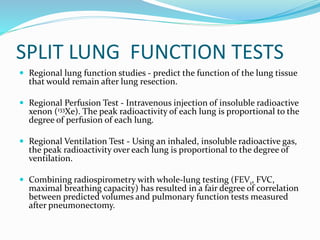
- Symptoms include chronic productive cough and sputum. Investigations include chest CT, which shows characteristic findings like airway dilation.
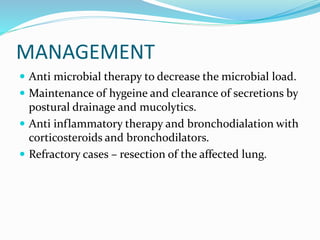
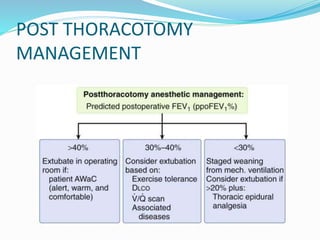
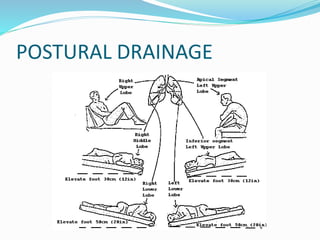
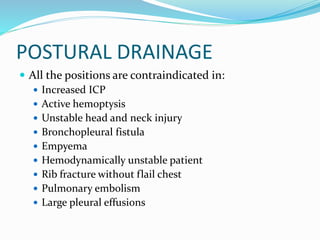
- Management focuses on airway clearance, antibiotics for infections, and