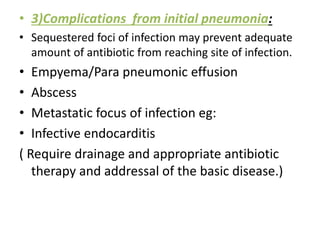
This document defines non-resolving pneumonia and discusses its causes and diagnostic evaluation. Non-resolving pneumonia is defined as persistence of clinical symptoms and radiographic abnormalities for longer than expected despite adequate antibiotic therapy. Common causes include inappropriate antibiotic therapy, complications of the initial infection, host factors, and presence of resistant or unusual pathogens. A thorough diagnostic evaluation includes assessing treatment response, looking for complications or superinfections, evaluating for unusual organisms, and examining host immune function. Radiological imaging, bronchoscopy with protected specimen brushing or biopsy, and CT-guided biopsies can help identify causative organisms or underlying conditions.