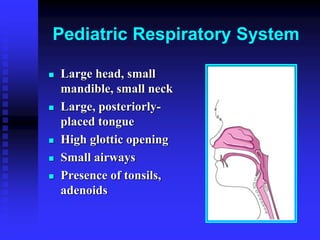
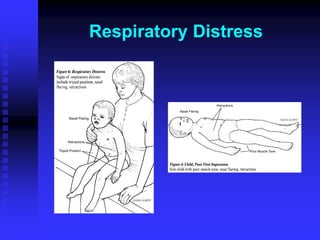
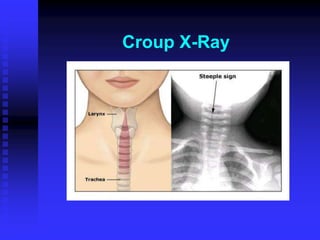
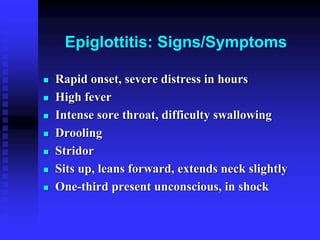
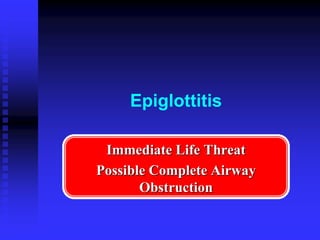
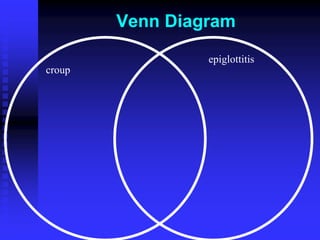
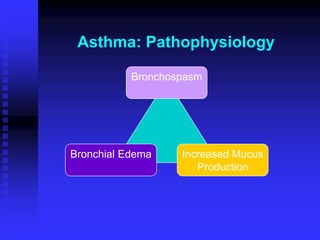
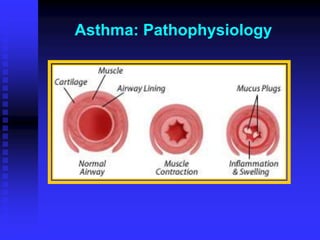
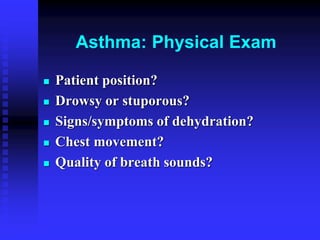
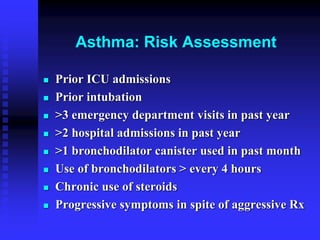
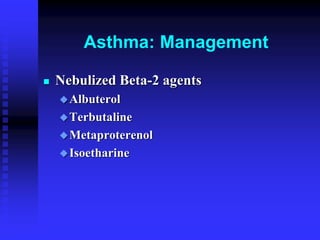
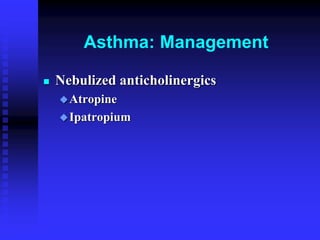
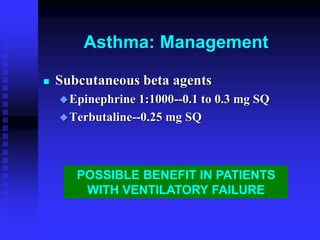
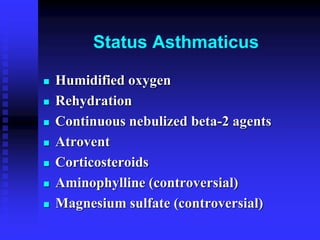
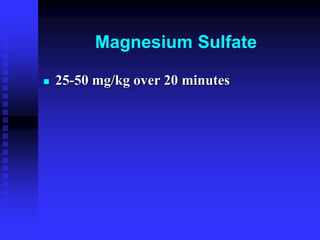
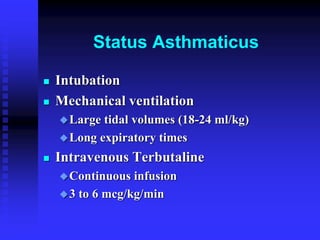
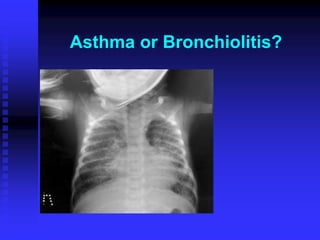
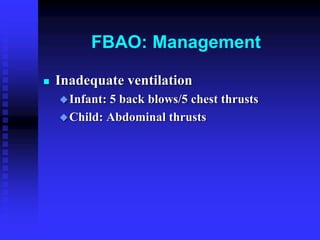
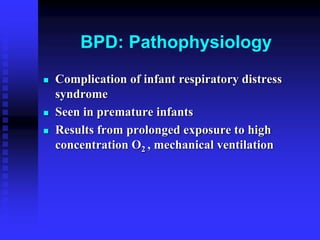
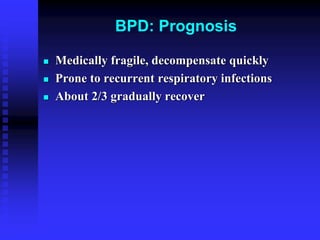
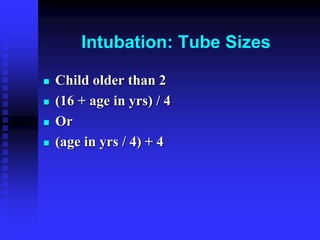
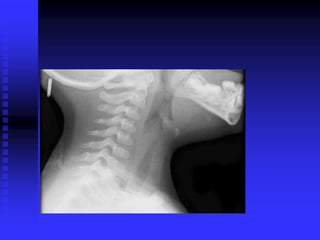
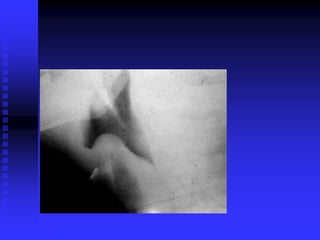
This document discusses various pediatric respiratory emergencies. It describes how the pediatric respiratory system makes children more vulnerable to respiratory failure. The most common causes of respiratory distress and failure in children are croup, epiglottitis, asthma, bronchiolitis, foreign body aspiration, and bronchopulmonary dysplasia. Each condition is discussed in detail, including pathophysiology, signs and symptoms, risk assessment, and management strategies. Special attention is given to distinguishing between similar conditions like asthma and bronchiolitis. Intubation tube sizes for children of different ages are also provided.