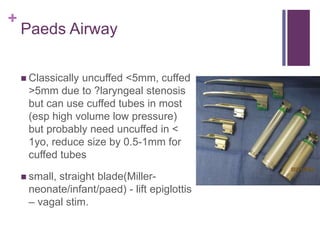
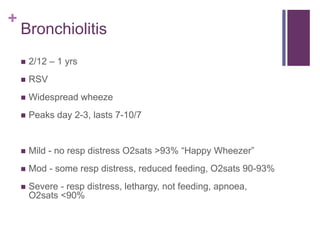
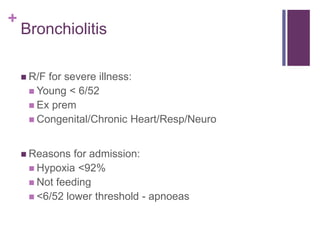
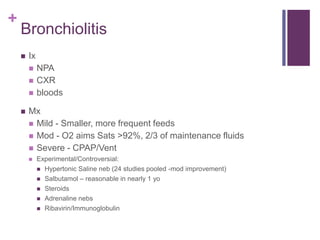
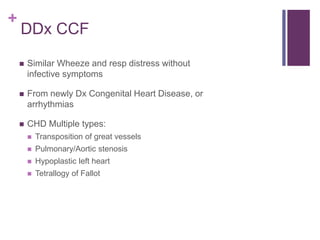
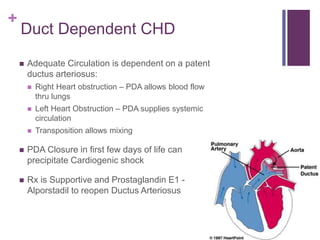
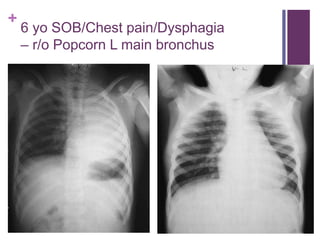
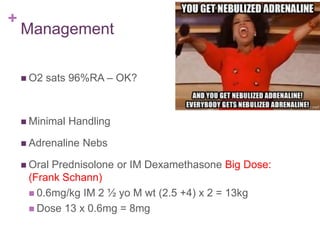
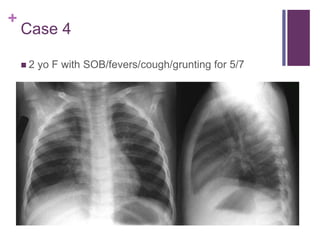
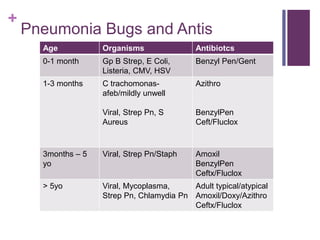
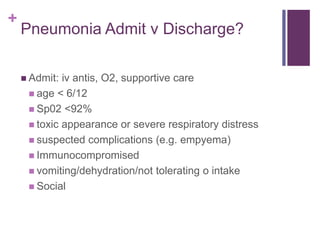
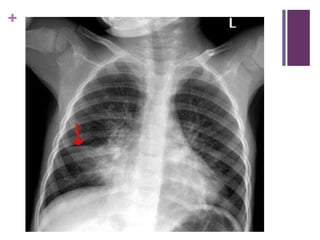
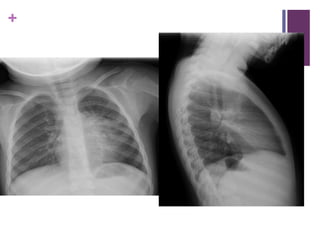
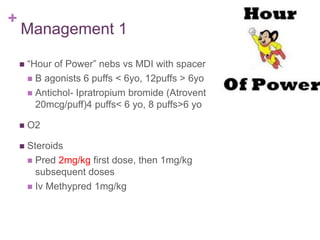
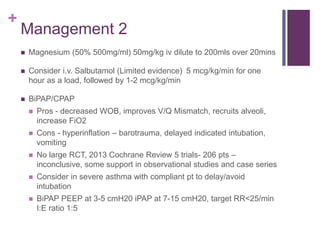
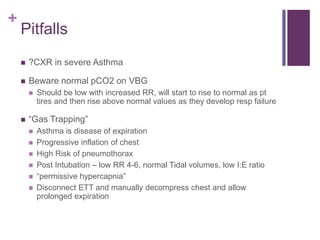
This document discusses shortness of breath in pediatric patients. It outlines common causes like respiratory infections, congestive heart failure, foreign body inhalation, and metabolic derangements. Assessment focuses on work of breathing, accessary muscle use, and associated symptoms. Key differences in the pediatric airway are described, along with implications for airway management. Five case examples demonstrate approaches to common conditions like bronchiolitis, croup, pneumonia, asthma, and foreign body inhalation. Management strategies for each condition are provided.