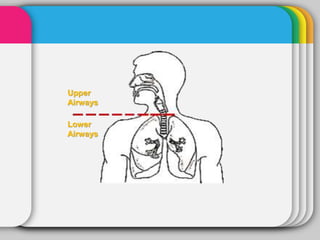
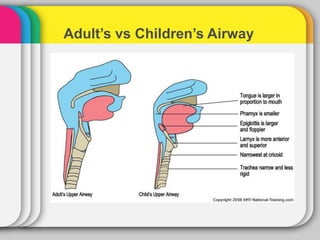
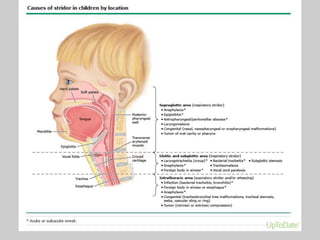
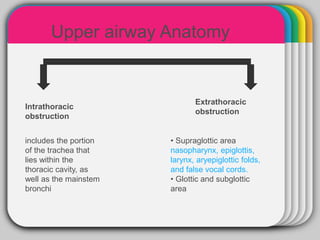
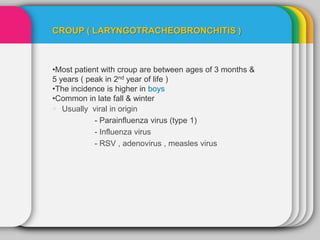
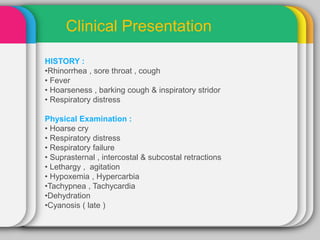
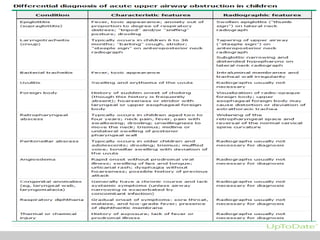
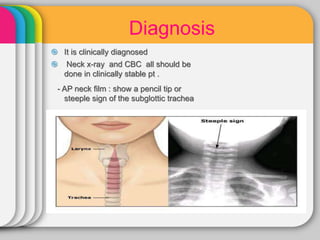
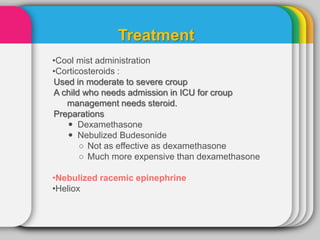
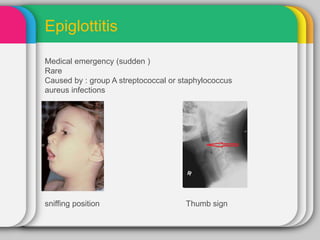
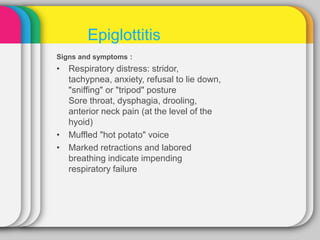
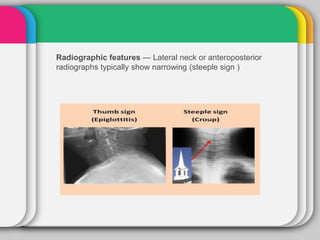
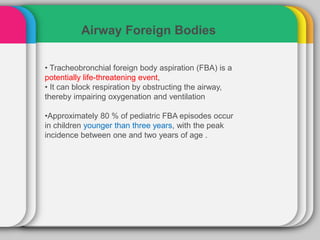
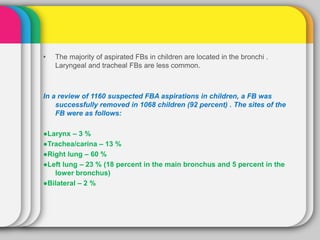
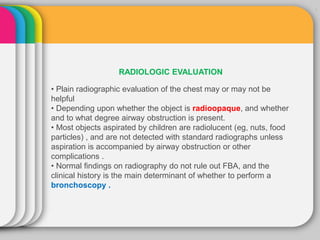
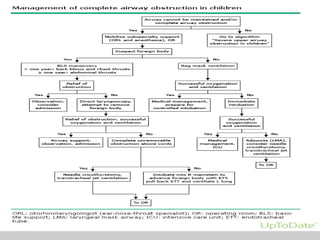
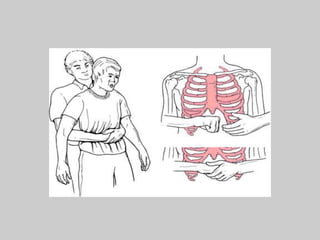
Upper airway obstruction can occur from the nose to the larynx. Croup is most common in children ages 3 months to 5 years and is usually caused by a viral infection like parainfluenza. Epiglottitis is a medical emergency typically caused by bacterial infections and can lead to sudden airway obstruction. Foreign body aspiration is also common in young children and requires prompt diagnosis and removal to prevent complications.