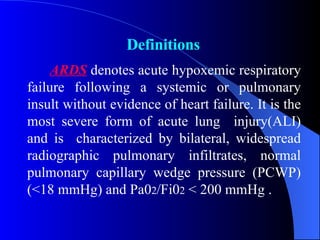
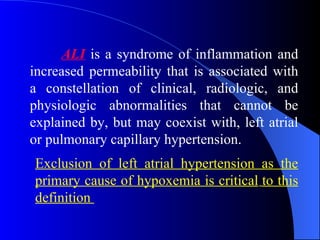
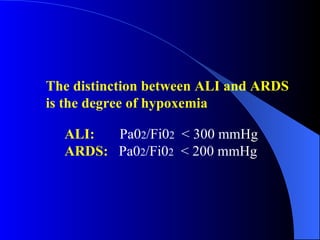
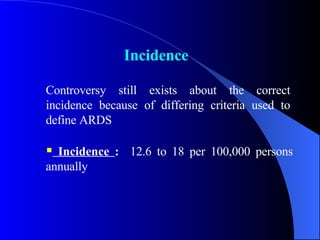
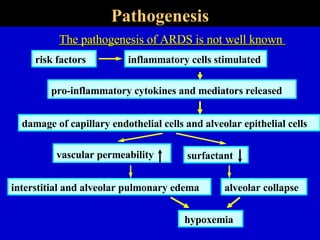
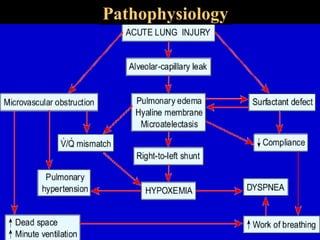
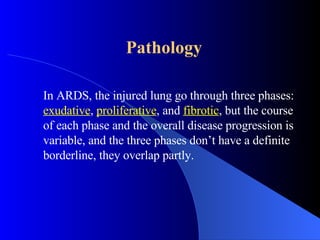
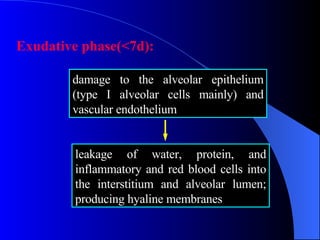
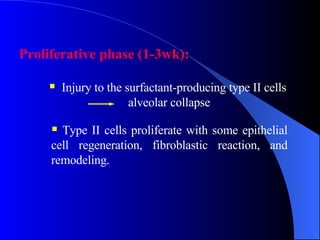
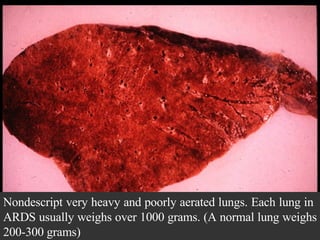
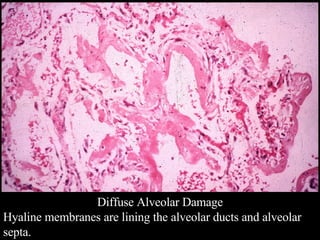
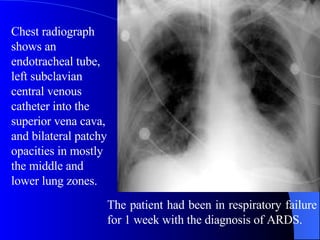
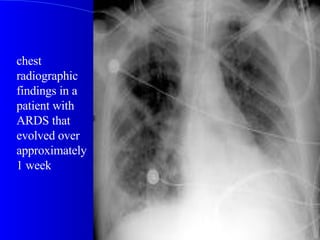
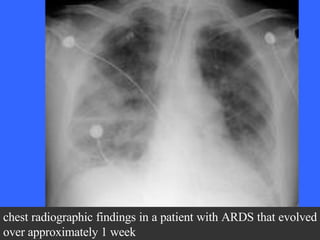
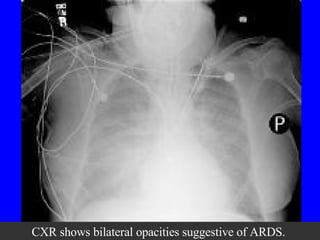
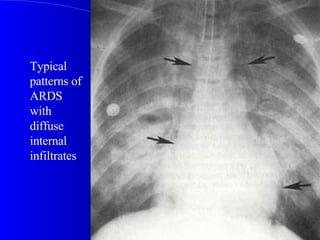
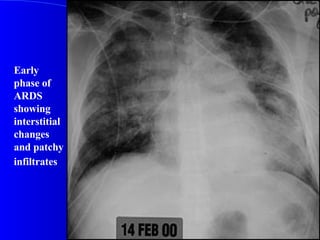
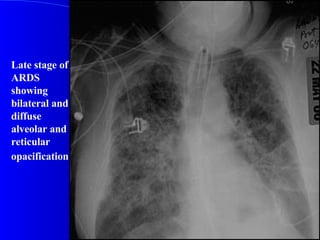
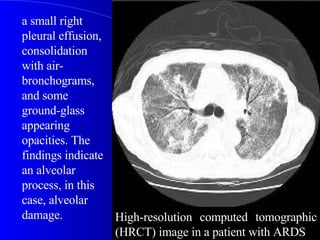
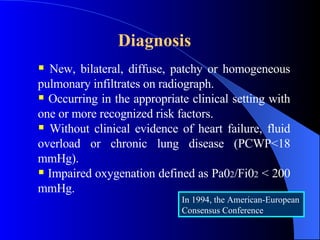
Acute Respiratory Distress Syndrome (ARDS) is an acute hypoxemic respiratory failure following a lung or systemic insult without heart failure. It involves diffuse bilateral lung infiltrates, normal heart functioning, and profound hypoxemia. Common causes include pneumonia, aspiration, and sepsis. Patients experience rapid onset of labored breathing and hypoxemia. Chest imaging shows bilateral infiltrates. Treatment focuses on supportive care, mechanical ventilation with low tidal volumes, and treating the underlying condition. While the mortality rate is high, especially with sepsis, outcomes have improved in recent decades.