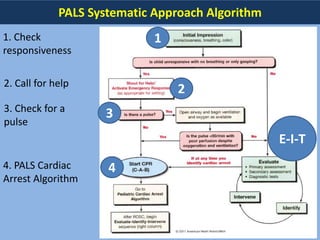
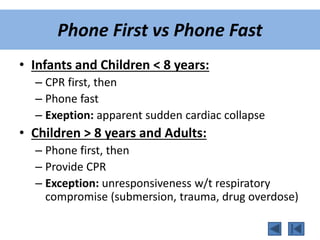
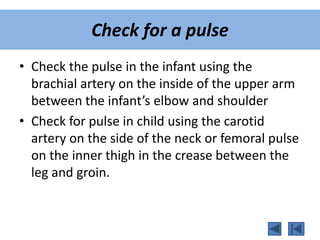
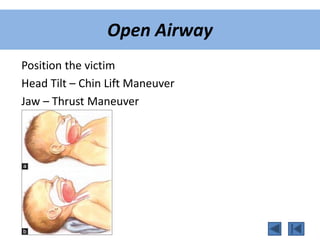
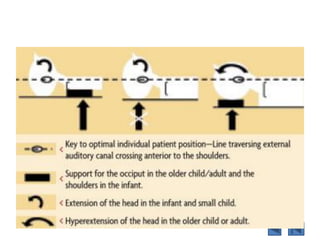
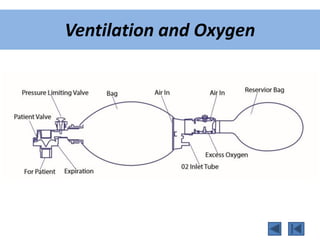
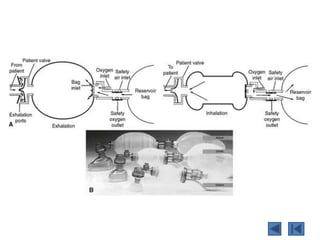
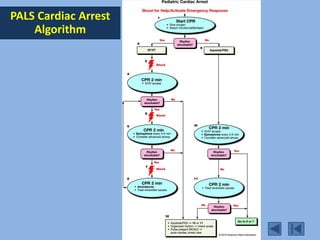
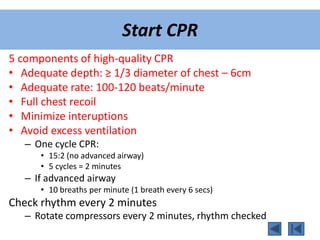
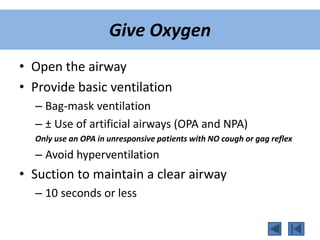
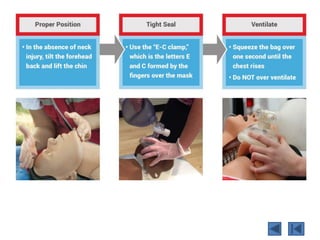
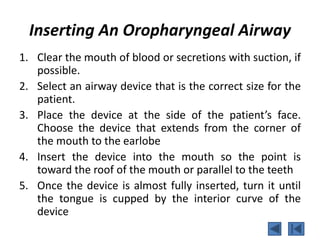
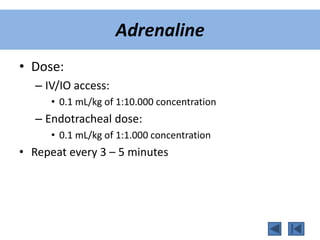
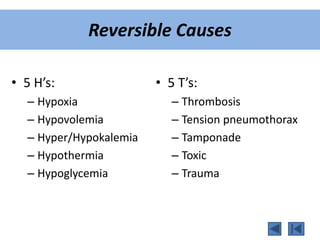
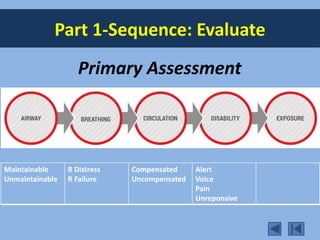
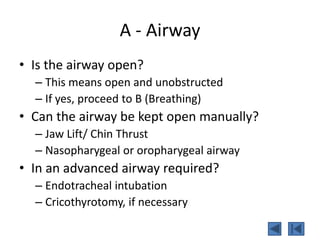
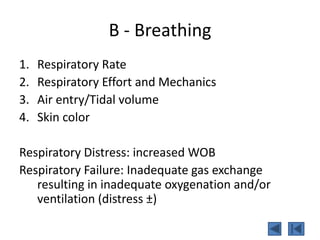
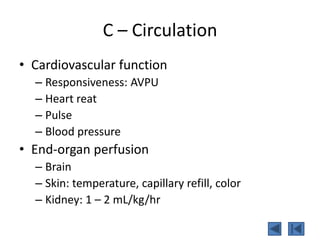
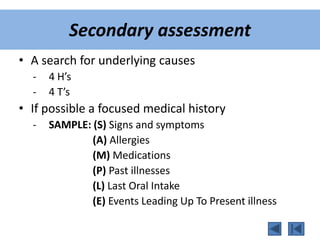
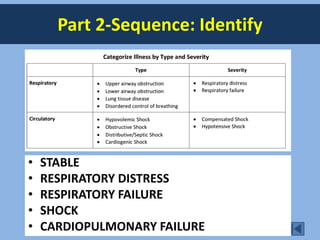
This document provides guidelines for pediatric advanced life support (PALS). It outlines the systematic approach algorithm which begins with checking responsiveness, calling for help, and checking for a pulse. The BLS assessment evaluates consciousness, breathing, and skin color to determine if the child is unresponsive with no breathing. For infants and children under 8, CPR should be provided first before calling for help, while those over 8 receive phone assistance first before CPR. The guidelines describe performing CPR, providing oxygen, inserting airways, monitoring the child, establishing IV/IO access, administering adrenaline, and considering reversible causes and an advanced airway. The primary and secondary assessment evaluates the child's airway, breathing, circulation, and