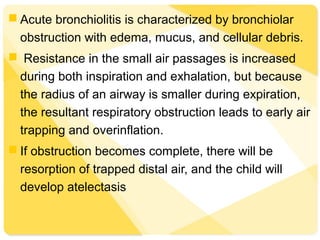
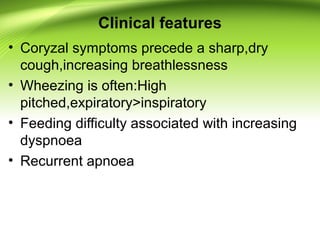
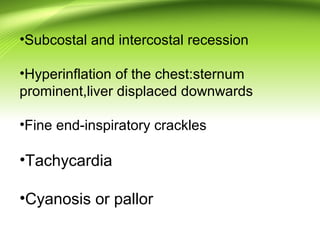
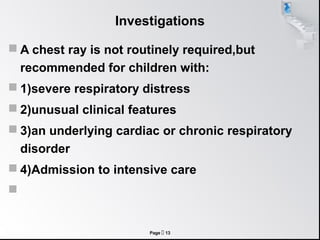
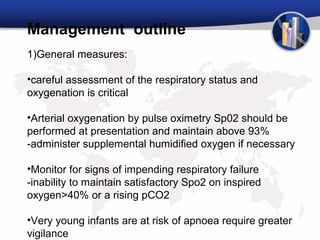
Bronchiolitis is an inflammation of the small airways (bronchioles) commonly caused by viral infection, especially respiratory syncytial virus (RSV) in infants under 1 year old. It causes wheezing and difficulty breathing. Clinical features include cough, wheezing, respiratory distress, and feeding difficulties. Chest x-ray may show hyperinflation of the lungs. Diagnosis is usually made clinically based on symptoms and age of the child. Treatment focuses on supportive care and monitoring for signs of worsening respiratory distress.