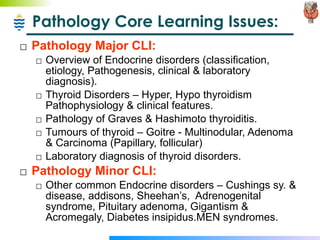
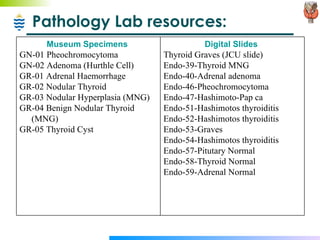
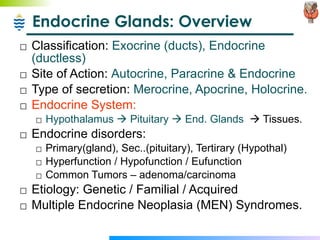
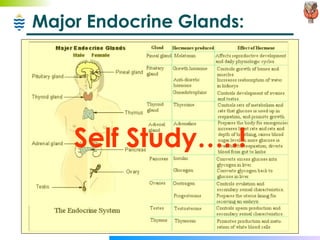
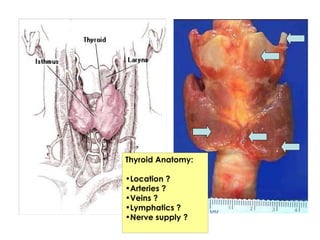
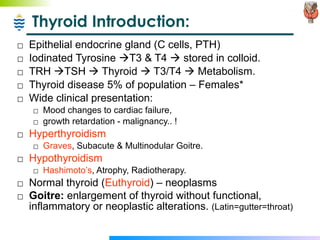
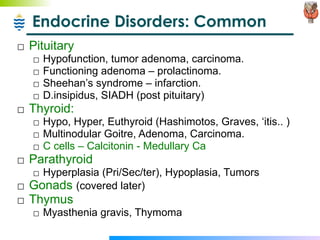
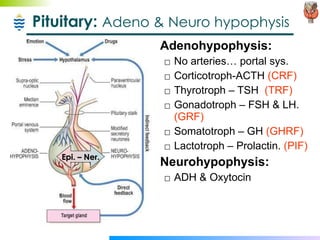
The document discusses thyroid pathology including:
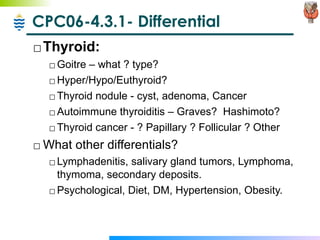
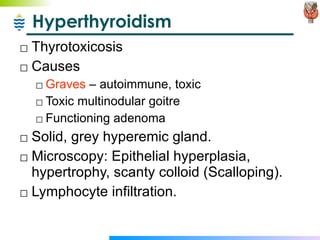
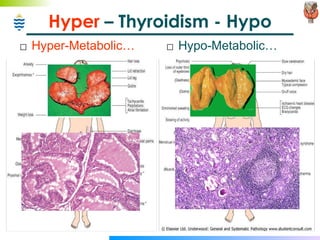
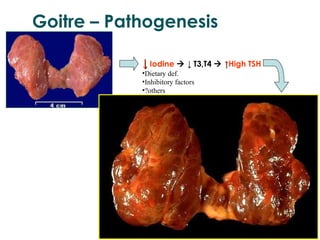
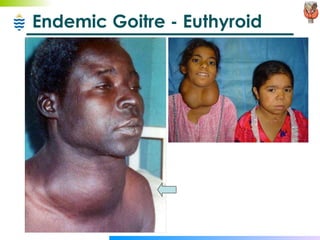
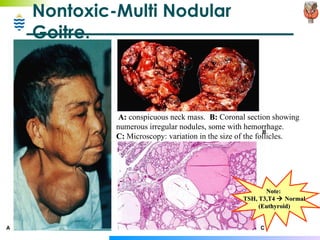
- Types of thyroid disorders - hyperthyroidism, hypothyroidism, and euthyroid goiters.
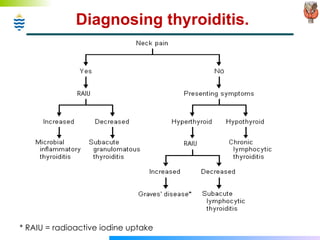
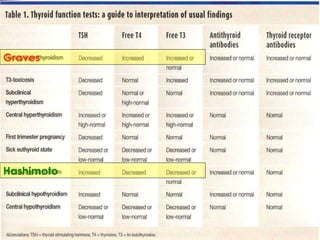
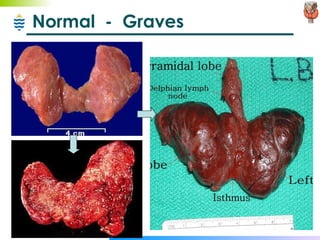
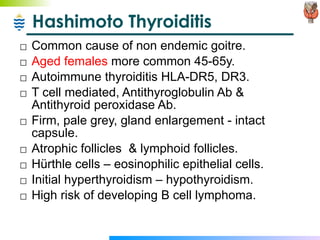
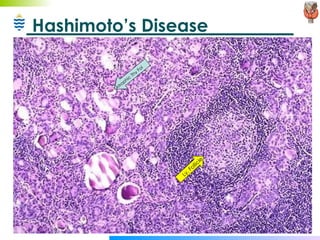
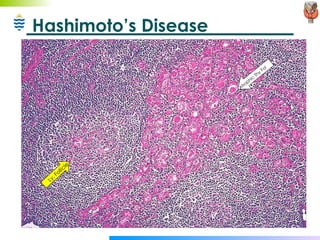
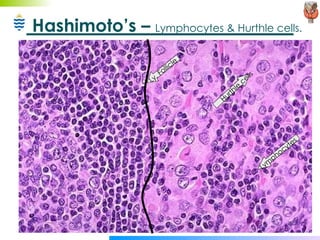
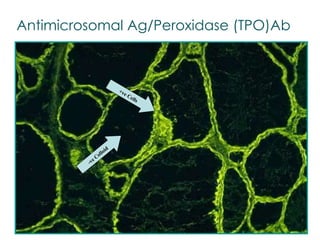
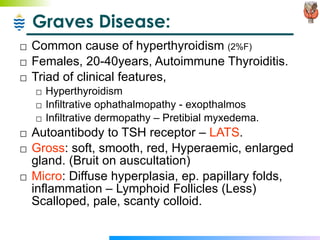
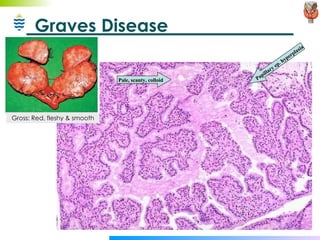
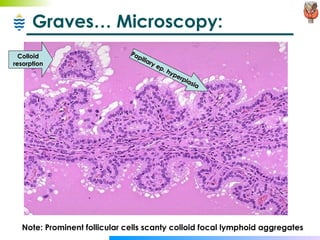
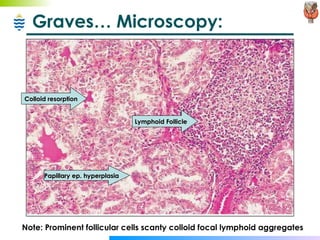
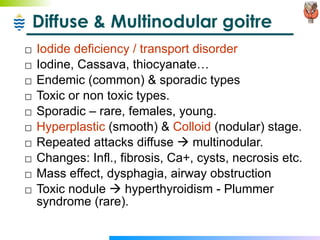
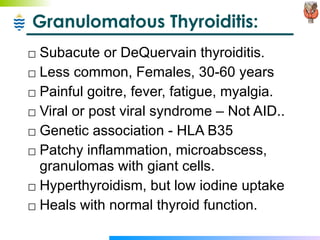
- Common causes like Graves' disease, Hashimoto's thyroiditis, multinodular goiter.
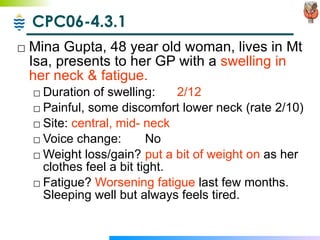
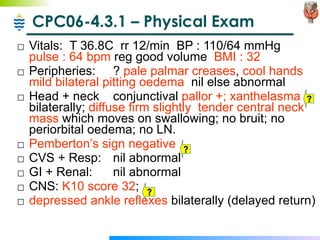
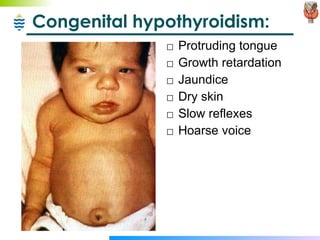
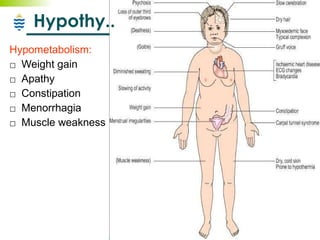
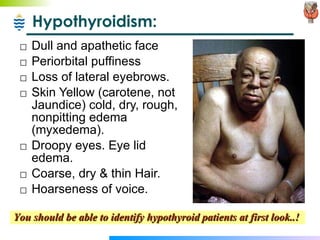
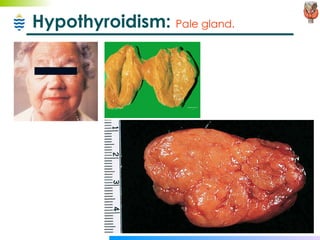
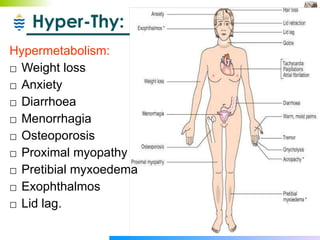
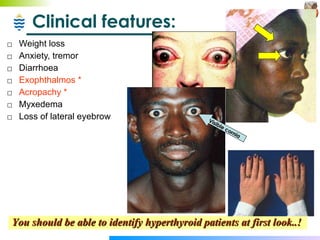
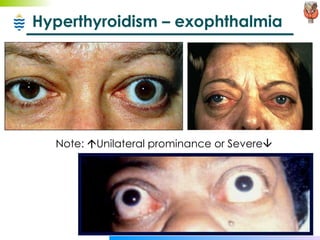
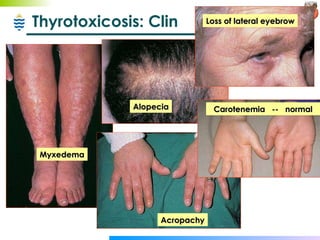
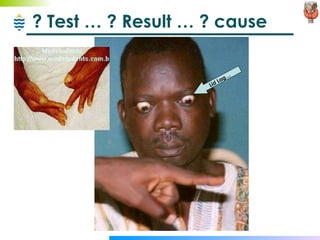
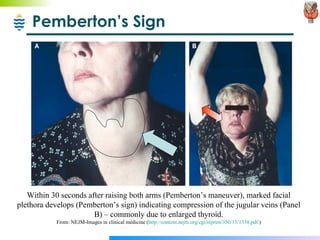
- Clinical features of hyperthyroidism and hypothyroidism.
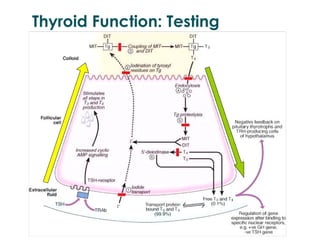
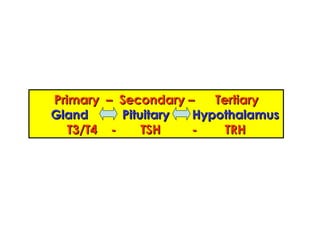
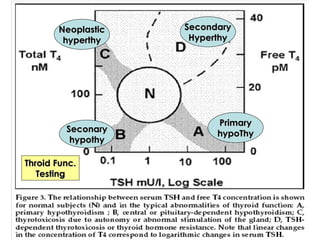
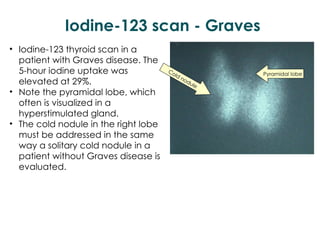
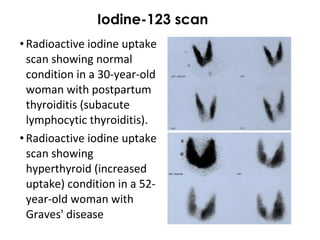
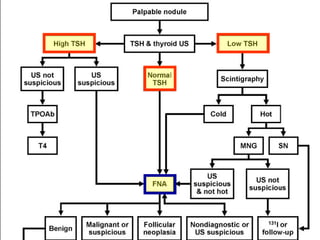
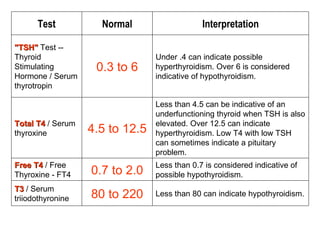
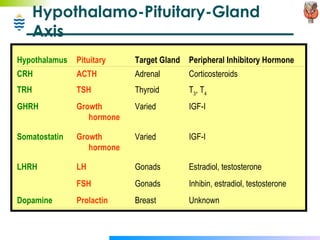
- Investigations like thyroid function tests and radioactive iodine uptake scans.
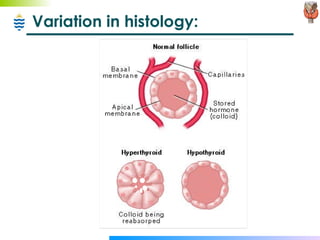
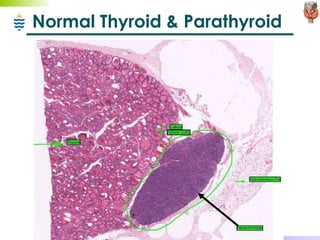
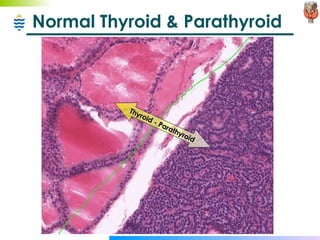
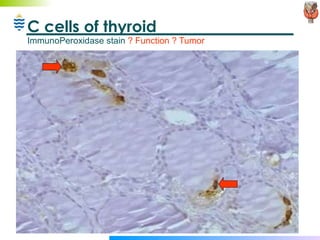
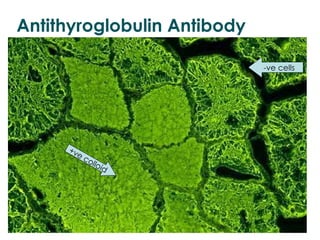
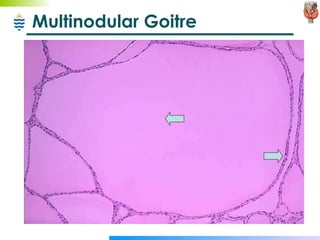
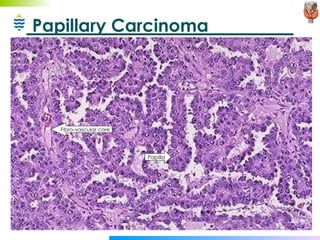
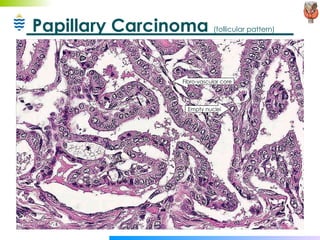
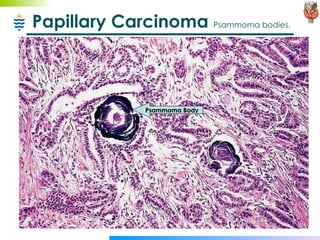
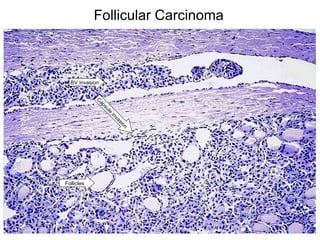
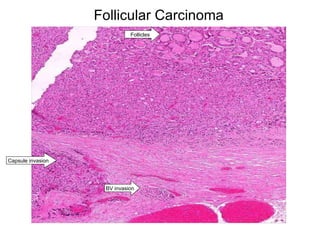
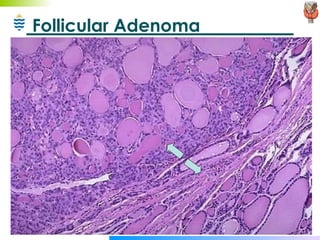
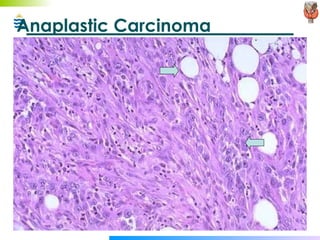
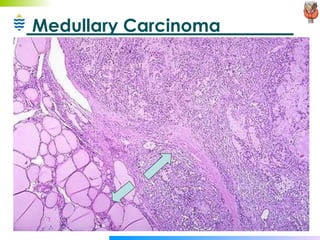
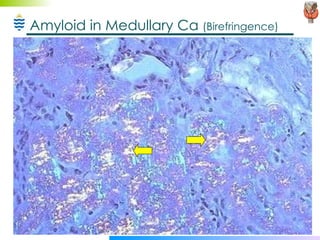
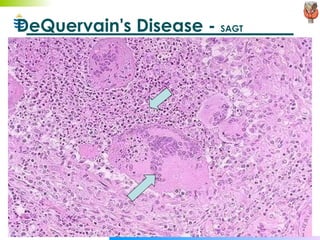
- Microscopic findings in various thyroid conditions.
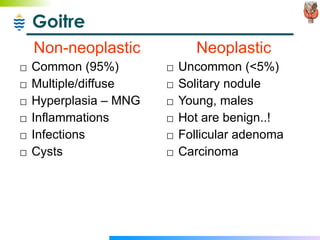
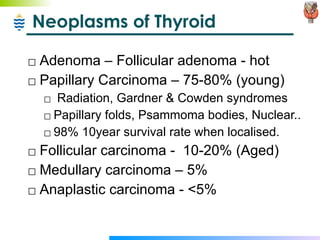
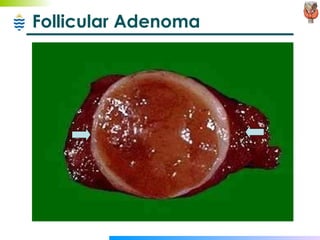
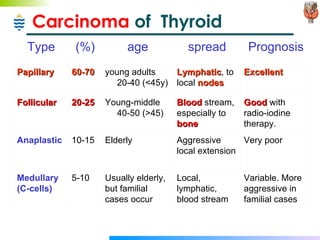
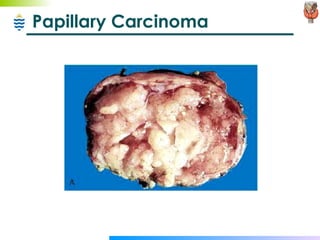
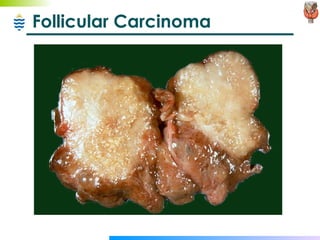
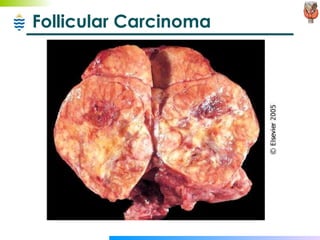
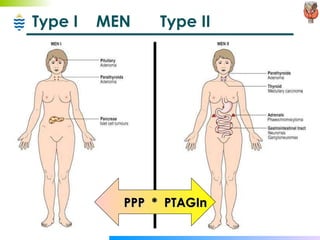
- Thyroid neoplasms including adenomas, papillary carcinoma, follicular carcinoma, and others.