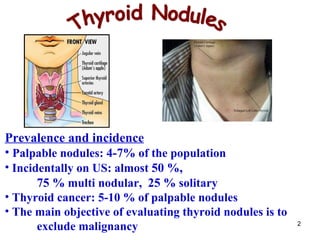
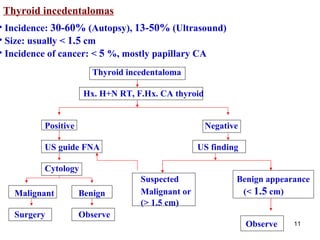
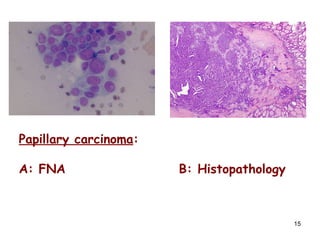
- Thyroid nodules are very common, found in 4-7% of people on physical exam and almost 50% on ultrasound, with most people having multiple nodules. Thyroid cancer is found in 5-10% of palpable nodules.
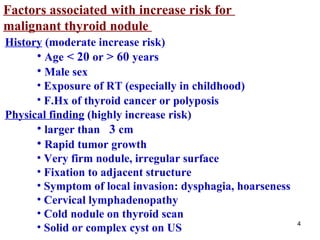
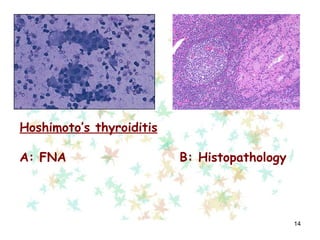
- Factors that increase cancer risk include nodule size over 3 cm, male sex, radiation exposure, family history of thyroid cancer, and symptoms of local invasion. Features suggesting benign nodules include a family history of autoimmune disease and benign nodules.
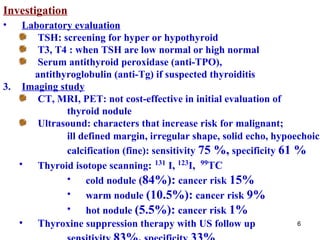
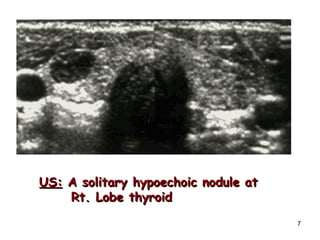
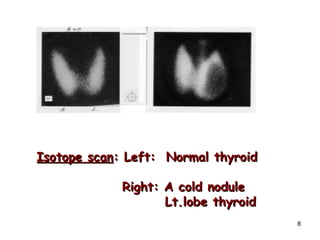
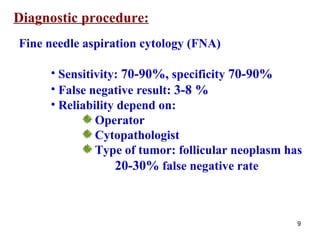
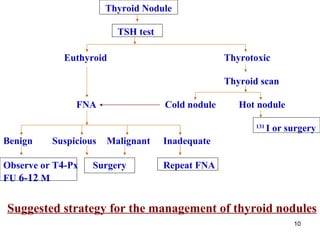
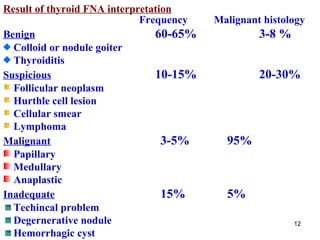
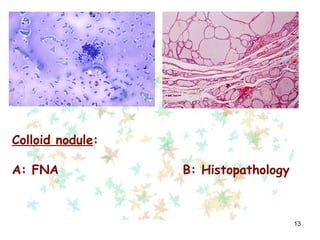
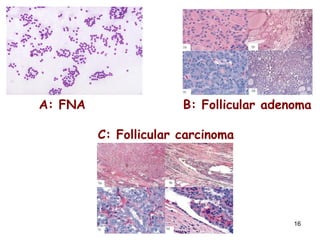
- Evaluation involves ultrasound, thyroid function tests, and fine needle aspiration of suspicious nodules, with surgery for nodules found to be malignant or indeterminate