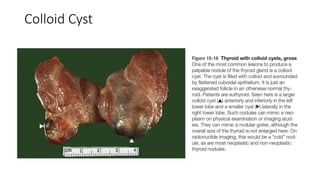
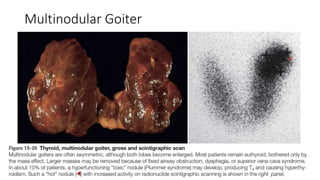
The document provides an overview of thyroid gland embryology, anatomy, common pathologies, and the steps for grossing a thyroid specimen in the laboratory. The thyroid gland develops from an endodermal outpouching in the embryo and normally descends to the anterior neck. Common pathologies include Hashimoto's thyroiditis, Graves' disease, multinodular goiter, and various thyroid cancers. When grossing a thyroid specimen, the pathologist examines, describes, weighs, measures, and sections the gland to identify any lesions for histological analysis.