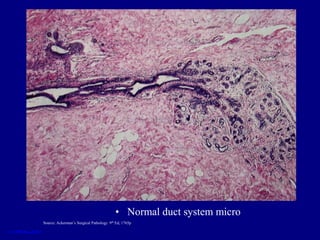
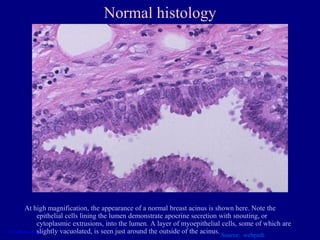
The document discusses normal breast anatomy and histology, as well as non-proliferative and proliferative breast conditions including fibrocystic changes, ductectasia, fat necrosis, epithelial hyperplasia, sclerosing adenosis, and papillomas. Both clinical presentations and microscopic features are described for various common breast diseases. The goal is to provide pathology residents with an overview of normal breast features and pathological lesions.